The Effect on Overall Cost and Health-Related Quality of Life by Inpatient Trajectories 3 Years Before and After Critical Illness-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Background: Pre-existing disease is
the most important factor in the prediction of health-related quality
of life (HRQoL) after intensive care. We hypothesised that the
“inpatient care trajectories” in the years before admission to the ICU
is a stronger predictor of HRQoL and mortality after intensive care than
pre-existing disease, and that it has significant effects on overall
costs.
Method:A retrospective
investigation in two combined medical and surgical ICUs in Sweden.
Inpatient care was assessed from the County administrative registry.
HRQoL (SF-36) was measured at 6, 12, 24, and 36 months after discharge.
Results:Of 1092 patients, 459
(73%) had pre-existing diseases, and among them 360 (57%) had at least
one inpatient episode less than 3 years before the ICU period, during
which the group used significantly more hospital resources than the
combined cost for all ICU care during the same time. The addition of
episodes of inpatient care to the regression model strongly reduced the
effect of pre-existing disease on HRQoL and was also a strong predictor
for early mortality after ICU.
Keywords: Long-term
survival; Health-related quality of life; Hospital inpatient care
episodes; Intensive Care; Mortality; Pre-existing diseasesAbbreviations: HRQoL: Health-Related Quality of Life; ICU: Intensive care unit; DRG: Diagnosis Related Groups; ICD: International Classification of Diseases; SF-36: Short Form 36; PF: Physical Functioning; RP: Role limited by Physical problems; BP: Bodily Pain; GH: General Health; VT: Vitality: SF; Social Functioning; RE: Role limited by Emotional problems; MH: Mental Health
Introduction
Intensive care (IC) uses substantial resources for
few patients [1]. In a recent study we showed that patients who require
IC have a high rate (73%) of pre-existing diseases, and that these
pre-existing diseases had a considerable impact on the patients’
perceived health-related quality of life (HRQoL) after critical illness
[2,3]. We still do not know, however, how much the pre-existing diseases
influenced the patterns of episodes of inpatient care several years
before admission to the Intensive Care Unit (ICU) and after. If such a
pattern exists it may be a better estimate of the previous burden of
disease than the diagnoses per se, and so improve the prediction of
HRQoL and mortality after discharge from the ICU. The economic aspects
of such periods are also of interest as the cost of care during the year
in which time is spent in the ICU is substantial, and an economic
burden on society. A special characteristic for Sweden is that all
inpatient events are centrally recorded, and each individual can be
traced by the matchless social security number. This provides a unique
chance to trace all inpatient events.
The objectives of this study were to describe the
extent of the episodes of inpatient care recorded during the three years
before admission to the ICU and to assess if there is any association
between this proxy of pre-existing disease on HRQoL
and mortality after IC. We hypothesised that the number of
inpatient care episodes before admission to ICU was a better
estimate of the burden of disease before that admission than
separate diagnoses, and that it could further explain HRQoL
and effects on mortality recorded after admission to the
ICU. We also hypothesised that given the rate of pre-existing
diseases reported among patients in the ICU, the corresponding
cost of inpatient care before and after admission to the ICU is
appreciable (inpatient care was also recorded for up to three
years after ICU care), and an important factor in the examination
of ICU-related costs.
Materials and Methods
Design and patients
The group studied was part of a larger group that had
previously been examined from several different perspectives,
[2-7] described in detail elsewhere [3].
From that study we extracted the participating patients
from two of the three ICUs. All patients were 18 years or over;
were consecutively admitted to the intensive care unit at the
university hospital between 1 August 2000 and 30 June 2004, or
the intensive care unit of the general hospital between 1March
2002 and 30 June 2004; remained in the ICU for more than 24
hours; and were alive 6 months after discharge from hospital.
Both ICUs admit roughly 600-750 patients each year.
Patients with primary coronary disease, those recovering after
heart surgery and neurosurgery, neonates, and patients with
burns are treated at other specialist units, and were excluded.
Nearly all the admissions to the study ICUs were emergencies,
and the primary admission diagnoses usually disturbances
of the respiratory or the circulatory systems, gastrointestinal
problems, and multiple trauma or sepsis.
We studied patients who were; 18 years or over; consecutively
admitted to the ICUs between 2000 and 2004; remained in the
ICU for more than 24 hours; were alive 6 months after discharge
from hospital; and consented to participate in the study.
The clinical databases in each hospital were used to extract
data on age, sex, diagnosis on admission, APACHE II score,
duration of stay in ICU and in hospital, time spent on a ventilator,
and outcome.
The study was approved by the Committee for Ethical
Research at the University of Health in Linköping. Written
informed consent was waived by the ERB.
Previous episode(s) of inpatient care
The episodes of inpatient care were recorded prospectively
from the hospitals’ central databases, but data were missing
for 18 patients. For the patients included in the study the episodes were extracted for years three, two, and one before
the year of admission to the ICU. For the year of admission to
the ICU, including the period in the ICU and the care in the ward
afterwards, we extracted the episodes of inpatient care during
and after discharge from hospital. We also extracted the data for
years one, two, and three after discharge.
Economy
To calculate the costs involved, the calculation was based
on the codes for Diagnosis Related Groups (DRG) [8]. DRG is
a system by which patients admitted to hospital are classified
by their medical diagnosis together with information about
the cost. A special medical statement is economically-weighted
based on diagnoses from the International Classification of
Diseases (ICD), age, sex, condition at discharge, and the presence
of complications or coexisting diseases. This means that patients
within each DRG category are similar clinically, and are expected
to use the same amount of resources.
Questionnaires and Instruments
Structured questionnaires were mailed to the study
population 6, 12, 24, and 36 months after discharge from hospital
[2,3]. The questionnaires contained questions about the patients’
background (civil state, children living at home, born in Sweden
or not, education, employment before and after admission to
the ICU, sick leave before and 6 months after discharge from the
ICU and hospital, and pre-existing diagnosis). The questionnaire
also asked, “Have you had any illness, reduced bodily function
or other medical problem for more than 6 months before the
ICU period” with the answer “yes” or “no”. This question also
gave the pre-specified choices of illness: “cancer, diabetes, heart
failure, asthma/allergy, rheumatic, gastrointestinal, blood,
kidney, psychiatric, neurological disease, thyroid or any other
metabolic disturbance, or any other long-term illness”. The last
option was an open question with a slot for free text. The open
question was used in less than 3% of cases.
Health-related Quality of Life
The Swedish version of the Medical Outcome Short Form
version 1 (SF-36) [9,10] was chosen to evaluate HRQoL. The
instrument is internationally known and has often been used
[11]. It has previously been applied in IC [2,3,12,13] and has
been recommended as the best instrument for measuring HRQoL
in trials in critical care [14].
SF-36 has been validated in a representative Swedish
sample [15]. It has 36 questions and generates a health profile
of 8 subscale scores: physical functioning (PF), role limited by
physical problems (RP), bodily pain (BP), general health (GH),
vitality (VT), social functioning (SF), role limited by emotional
problems (RE), and mental health (MH) [9,15]. The scores of all
the subscales are transformed to a scale ranging from 0 (worst)
to 100 (best). To maximise the statistical power, the six-month follow-up data was used for this purpose (n=631).
Statistical methods
Data are presented as descriptive statistics. Unadjusted twosample
comparisons (the chi square test and Student’s t test)
were used to assess differences in background characteristics
between the groups as appropriate. In the comparison of HRQoL
(SF-36) between the groups (no episodes of inpatient care, 1 and
>1 episodes of inpatient care) we used ANOVA.
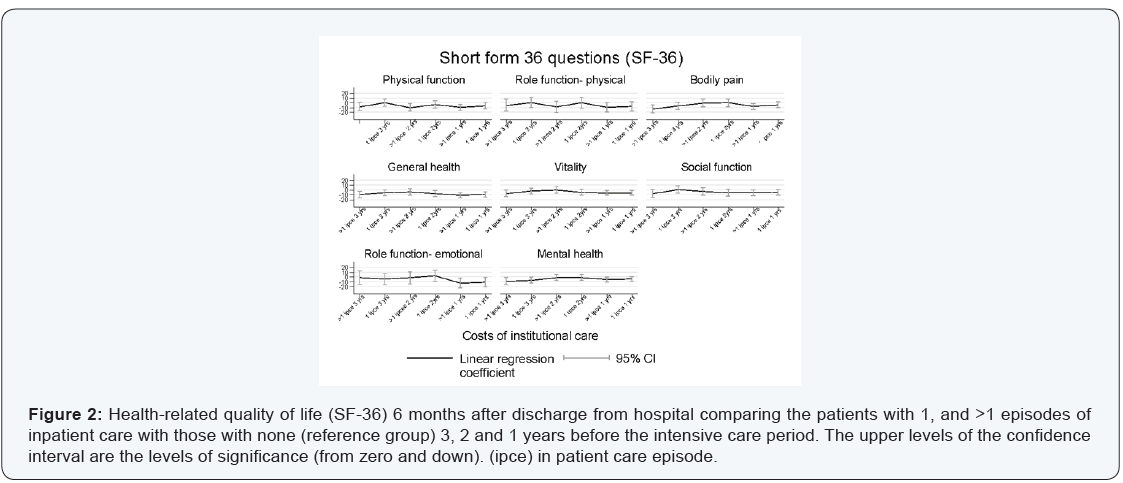
To model the impact of in-patient care episodes one, two
and three years before on HRQoL, a linear regression model was
used with each dimension of SF-36 as dependent variable and
sex, age and the hospital in-patient care episodes one, two and
three years before as independent variables. From the model,
the coefficients for the hospital in-patient care episodes together
with their 95% confidence interval were plotted.
Data are presented as two-tailed values and 95 % CI, and
were analysed with the help of SPSS (version 20.0, SPSS Inc.
Chicago, USA).
Results
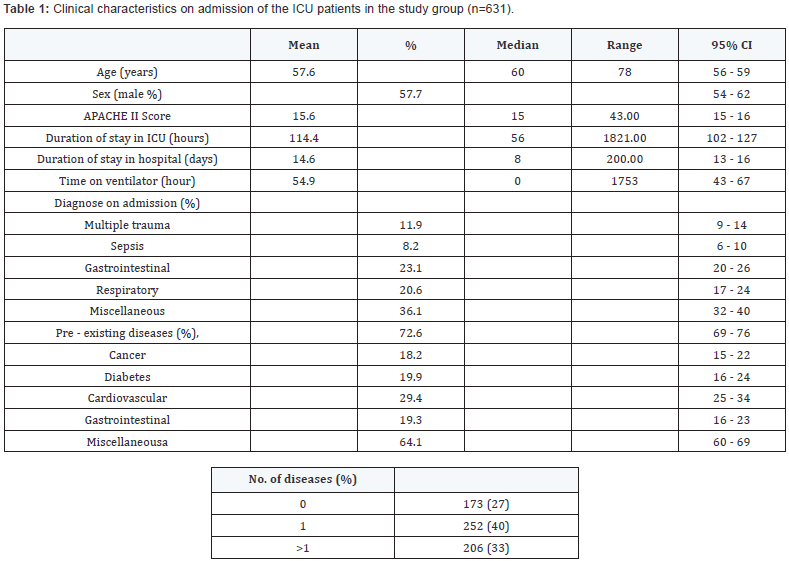
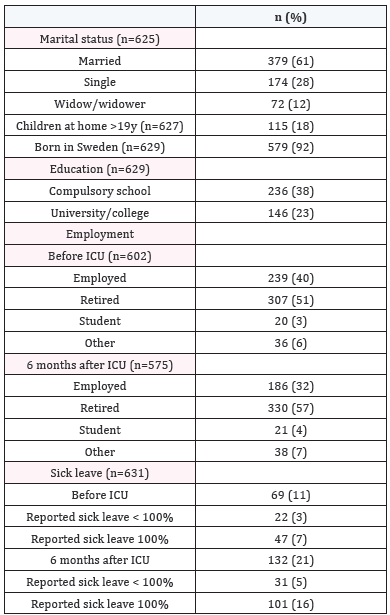
Clinical and personal characteristics of the patients
A total of 1092 patients met the inclusion criteria. After
two reminders 631 patients (58%) answered the mailed
questionnaire. The patients who did not respond in the study
differed from the group who responded in that they had shorter
length of stay in the ICU (P<0.001), and shorter time on ventilator
(P=0.02). There were no significant differences between the
non-responders and responders in gender, age, APACHE II
score or length of stay in hospital. The clinical characteristics of
the ICU patients in the study group are shown in Table 1, and
the socio-economic characteristics are shown in Table 2. The
patients from the university hospital ICU were younger (56 vs
61 years (p=0.001)), had higher disability or Apache II scores
(16.2 vs 14.7 (p=0.019), and more admissions with a diagnosis
of multiple trauma and sepsis (n=53, 14.3% vs n=22, 8.4% and
n=38, 10.2% vs n=15, 5.7% (p=<0.001)) respectively. There
were no significant differences between the two hospital groups
in sex, duration of stay in ICU or in hospital, time on ventilator, or
pre-existing disease (data not shown).
Episodes of inpatient care
Of the patients included, 360 (57%) had at least one episode
of inpatient care within the 3 years before the admission to ICU.
The ICU patients with pre-existing diseases used significantly
more hospital resources 3, 2, and 1 year before admission to
the ICU (p= 0.008, <0.001, and <0.001), and up to 3 years after
discharge regarding amount of care (number of visits) (p=
0.003), duration of stay (p=0.001), and costs (p=0.002), but
there were no differences during the ICU period in that preexisting
disease did not increase the cost of the stay in ICU. Most
importantly, there was a significant increase in the number of
episodes of inpatient care for the 3 years before admission to
ICU (p<0.001).
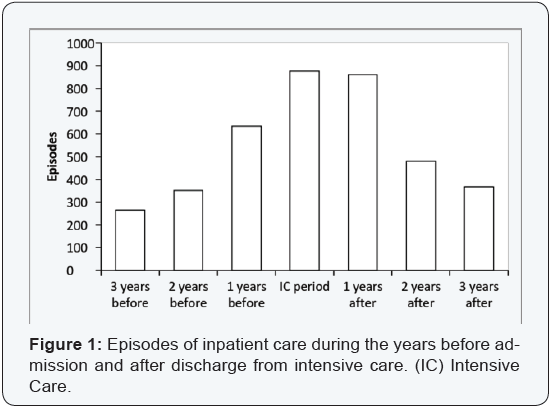
A total of 3669 inpatient care episodes were recorded: 939
occasions during the 3 years before the year of the admission
to the ICU, 953 during the year of IC, and a total of 1777 from
years 1-3 after discharge from the ICU by all the 631 patients
included in the study. The episodes of inpatient care increased from month 30 before the IC period, and 145 (23%) of the study
group had at least one inpatient care episode three years before
the IC period; 158 (25%) two years before; and 278 (44%) one
year before the IC period. After IC the number of inpatient care
slowly decreased and 334 (53%), 208 (33%), and 170 (27%)
of the study group had at least one inpatient care episode 1, 2,
and 3 years, respectively, after the period in IC (Figure 1). The
number after IC also includes those patients who died during
this period.
A total of 461 (73%) of the former IC patients had preexisting
disease which was present at least 6 months before
admission to the ICU. One year before their admission (p=0.003),
and one (p=0.001), two (p=0.002), and three years (p=0.046)
after their admission to IC the patients with pre-existing diseases
had significantly more inpatient episodes than the previously
healthy patients in the ICU.
The diagnoses on admission had no significant effect on
the episodes of inpatient care apart from gastrointestinal and
respiratory diseases one year before (p<0.001) and one year
after (p=0.001) the time spent in IC.
 DRG: Diagnosis Related Group; ICU: Intensive Care Units
DRG: Diagnosis Related Group; ICU: Intensive Care Units
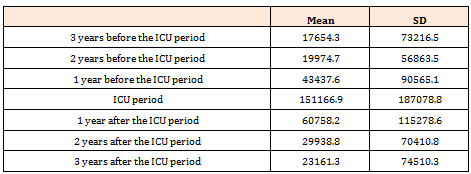
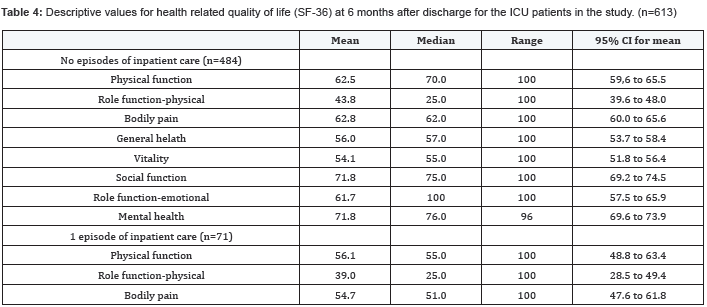
The costs in DRG/year for the episodes of inpatient
care are
shown in Table 3. The peak is during the period in IC and one
month after, to be in total at nearly the same level before as after the
time spent in IC. When all care during the 3 years before and
after the ICU stay is added for those patients who had episodes
of inpatient care, the total DRG cost was roughly 50% higher
than the total cost of ICU for all the patients.
When we examined the effect of episodes of inpatient care
before the ICU period we found that patients who had previously
been an inpatient were older (p<0.02) and had more pre-existing
diseases (p< 0.007).
Health-related quality of life
Six months after discharge the results for HRQoL (age and
sex adjusted) between the three groups being compared were
as follows. From three years before the IC period they had 0,
1, and >1, episode of inpatient care compared with the group
with no episodes of inpatient care. The group with >1 episode
of inpatient care one year before the period spent in the ICU had significantly reduced HRQoL in all 8 SF-36 dimensions, and for
1 episode of inpatient care 5/8 dimensions were significantly
affected (all except role limitation by physical problems, bodily
pain, and social function). Episodes of inpatient care two years
before the admission to ICU had minor effects. For >1 episode of
inpatient care there were significantly reduced effects on HRQoL
for physical function. For 1 episode of inpatient care, there were
effects on general health. Episodes of inpatient care three years
before the admission to the ICU had, for those with >1 episode
of inpatient care, an effect on limitations of role by physical
problems and emotional problems, whereas those with 1 episode
of inpatient care had effects on bodily pain, general health, and
mental health (Figure 2 & Table 4). When we examined the
effect of pre-existing disease and the episodes of inpatient care
in the same linear regression (n=609), the effect of pre-existing
disease was eliminated (β=0.584; p=0.09) when the episodes of
inpatient care were introduced (β=0.014; p=0.003).
Mortality
We found that mortality after ICU increases (p<0.001) if the
episodes of inpatient care are in the year before the admission
to ICU. If 1 episode of inpatient care is recorded the mortality
increases twofold, whereas if there are >1, the mortality is
quadrupled (Table 5).
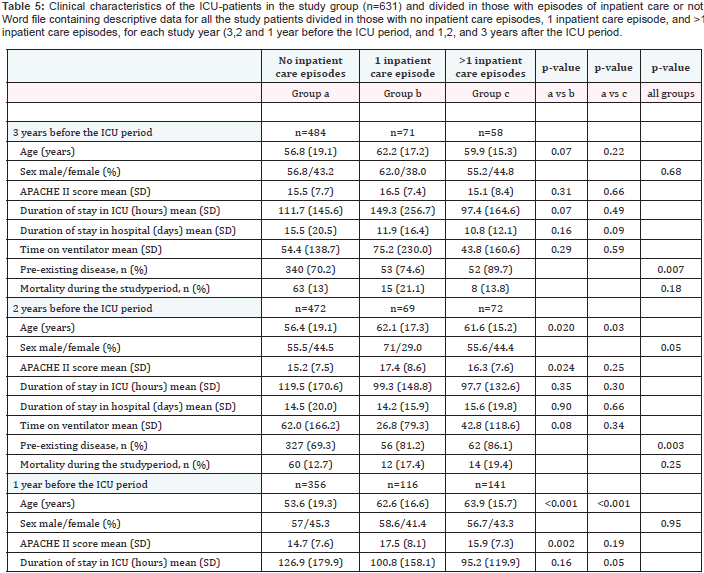 13 patients have missing data of inpatient care episodes.
13 patients have missing data of inpatient care episodes.Discussion
We have made four new and important observations. First,
our results suggest that episodes of inpatient care are a good
measure of the amount of pre-existing illness, and may be a
better proxy for it than diagnoses themselves, particularly for
HRQoL. The episodes before and after the admission to IC were
also closely related to the patient’s pre-existing state of health.
Secondly, episodes of inpatient care before the admission
to ICU had a significantly decreasing effect on HRQoL recorded
after the period in ICU. This was seen particularly if there was
more than 1 episode, and if the episode was in the year before
the admission to IC. The results suggest that 1 or >1 episode
of inpatient care during the year before the admission to ICU
is significant for all dimensions of HRQoL. This was the most
important effect recorded on HRQoL.
Thirdly, a large proportion of the patients who will later be
admitted to the ICU had important episodes of inpatient care
during the period from three years before admission to the
ICU. Most of these inpatient events happened near to the time
of admission to the ICU, and 57% of the patients had least 1
episode as early as three years before the admission to IC. For
these patients the DRG costs were 50% higher during the three years before and after admission to the ICU than for the entire
aggregated cost of IC for all the patients in ICU. The costs for
the inpatient episodes increased linearly from year three to year
one before admission to the ICU. There is an inverse pattern
for the years after admission to the ICU, with many episodes of
inpatient care during the first year after admission to ICU. After
three years this effect disappeared.
Fourthly, and importantly, mortality after admission to the
ICU increased significantly if the episodes of inpatient care
were in the year preceding admission to the ICU. If 1 episode of
inpatient care increases the mortality twofold, then if there is >1
the mortality is quadrupled. Our study has extended previous
research that showed that pre-existing diseases had an impact
on mortality, [16-18] and is the first study to our knowledge to
show that the number of episodes of inpatient care also have a
major impact on mortality after admission to the ICU.
We think that the results presented are of general value as
was suggested in previous studies [2,3]. The characteristics of
the population that we studied match western European data
well. The unique circumstance that provided the data for this
study is that the Swedish inpatient registry can provide data
about episodes of inpatient care for all patients cared for in the
Swedish health care system.
The patients who were admitted to hospital for inpatient
care were older and had more pre-existing conditions than
those who were not, and this was the trend from year two before
admission to the ICU to year two afterwards. This indicates that
an unhealthy state that leads to an admission to hospital for
older patients can predict the future need for IC, reduced HRQoL,
and early mortality.
In previous studies we have shown that pre-existing
diseases are of significant importance for perceived HRQoL after
ICU care [2,3,19] and this study emphasises in a different way
the need for assessment of pre-existing diseases in patients in
the ICU because they are common, they increase the risk of ICU
admission, and have an impact on both HRQoL and mortality.
It is possible that the patients with pre-existing diseases have
reduced HRQoL as long as three years before admission to
the ICU. Similarly, analyses from other studies show that the
incidences of pre-existing conditions before admission range
between 48% and 77% of the patients in ICU [16,20,21].
Consequently, the incidence in the present study is not
unique, and indicates that the data would be generalizable at
least in Western Europe. The most common pre-existing disease
in our study was cardiovascular disease (29%, n=134). This is in
line with a previously study from Denmark, in which the authors
had analysed pre-admission morbidity in 28,172 patients in
ICU using the Charlson Comorbidity Index and found that one
of the most common pre-existing conditions was cardiovascular
disease [16].
This work has some limitations. First, the use of only two
centers has limited the selection of patients. However, at the
time of data collection not all hospitals in Sweden had provided
data to the registry. Secondly, we have included only data about
inpatients. A wide field of health care is provided to outpatients,
such as for diabetes, for example. Unfortunately data on
outpatients was not at the time available from the Swedish
patient registry database. Thirdly, criteria for inpatient care
may vary between patients and hospital and also due to other
subjective measures. However, inpatient care beds are usually in
shortage why patients must often need to present a significant
disease pattern to be admitted. We consider this factor less
important for the conclusions. Fourthly, the pre-existing diseases
were self-reported and did not take into account the seriousness
and the burden of each disease [22]. This has been previously
discussed [3]. Fifth, the present study does not take into account
the costs for the withdrawal of drugs. In Sweden, at the time of
the study period, we did not have prescription drugs recorded
centrally. With that in mind the total costs can be altered,
possibly increasing the costs for both periods before and after
admission to the ICU. However, it would not change the effect
of pre-existing diseases on the episodes of inpatient care. Sixth,
it is important for the strengths of the conclusions made in the
present paper to note that there is a significant loss to follow-up.
The low response rate, however, is in the range commonly seen
in similar studies. Lastly, the last data samples are from 2008,
and the final manuscript has been delayed due to the complexity
of data collection. However, we think the large and congruent
changes observed and the treatment pattern changes in these
respects (co-morbidity and costs) are not altered to the extent
over time that it will affect the major conclusions drawn.
Conclusions
Episodes of inpatient care 3 years before and after an
admission to ICU take a large amount of hospital resources and
exceed the total cost of IC. It, inpatient care before ICU, is a better
predictor of HRQoL after IC than pre-existing clinical diagnoses
and a strong predictor for IC and after ICU mortality. This finding
further strengthens the importance of the effect of pre-existing
state of health on outcome after critical illness.
Acknowledgements
The present study is supported, in part, by a grant from The
Health Research Council in the South-East of Sweden (FORSS)
F2002-207, F2004-204, FORSS-5515, and the County Council of
Östergötland, Sweden and by a grant from The Centre for Medical
Technology assessment, Department of Medicine and Health
Sciences, Linköping University County Council of Östergötland,
Linköping, Sweden.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php

Comments
Post a Comment