Heerfordt's Syndrome: A New Atypical Clinical Presentation-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Heerfordt’s syndrome is an unusual clinical
manifestation (less than 5%) of sarcoidosis, characterized by parotitis,
uveitis, and peripheral facial palsy, febrile syndrome is usually
associated. Oral corticosteroid is the treatment of choice. We report a
case of a patient in which the syndrome of Heerfordt was retained.
Keywords: Heerfordt’s syndrome, parotitis, uveitis, sarcoidosis, facial palsy.Introduction
The sarcoidosis is a systemic granulomatosis of
unknown cause, characterized by its clinical polymorphism and a wide
variety of its modes of presentation. The combination of fever, uveitis,
parotitis and peripheral facial paralysis defines Heerfordt’s syndrome
which presents an unusual manifestation of this disease. We report a
case of a patient in which the syndrome of Heerfordt was found.
Case Report
A 49 year-old female followed in ophthalmology for
bilateral uveitis, was referred to the ENT consultation for nasal
obstruction with crusting rhinitis. General examination was
unremarkableexcept a low-grade febrile state, especially there was no
facial palsy. The patient has undergone a rhinocavoscopy which revealed
the presence of nodular lesions in the lower horn. A biopsy of the
lesions was performed which results normal. The evolution of the
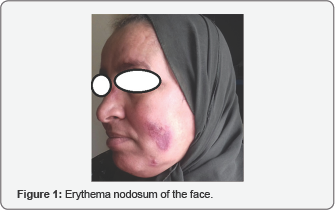
symptomatology was marked by the appearance of erythema nodosum on the
face and the upper limbs (Figure 1).
The diagnosis of sarcoidosis was confirmed by the
biopsy of the cutaneous lesions which showed non-caseatingepithelioid
granulomas.

Facial CT scan highlighted a multinodular bilateral chronic parotitis (Figure 2),
therefore, the diagnosis of Heerfordt’s syndrome was retained in view
of these highly evocative criteria even if the symptomatology was
incomplete given the absence of facial palsy. The patient was initiated
on long-term steroid therapy. After a month of treatment with oral
steroids, clinical symptoms have shown a clear improvement.
Discussion
Sarcoidosis is a chronic inflammatory disorder of
unknown etiology, characterized by noncaseating granulomas involving the
lungs in more than 90% of patients. Ocular, lymph-node, and cutaneous
manifestations are next in frequency, but any organ system can be
affected by the disease.The diagnosis requires exclusion of other
etiologies, such as Sjogren's syndrome, tuberculosis, fungal and
parasitic infections, Wegener's granulomatosis [1].
Otolaryngologic manifestations are identified in 10-15 % of patients, the most common being cervical adenopathy [2].
Salivary glands are less frequently involved, unilateral or bilateral
swelling of the parotid gland was reported in only 6-8% of patients with
sarcoidosis [3]. It can be included in Heerfordt’s syndrome (uveoparotid fever).
Heerfordt’s syndrome is a sarcoidosis syndrome
characterized by mild fever, painless parotid gland enlargement, cranial
nerve involvement, and anterior uveitis [2].
It is considered as one of the first central nervous system
involvements to be described as a neurological presentation of
sarcoidosis. The complete form occurs in approximately 0.3% of all
sarcoidosis cases [4]. The etiology of this condition is still unclear and, as a result, so is the pathogenesis [1].
The incidence of cranial nerve palsy in sarcoidosis is about 5 % [5], with the facial nerve followed by the optic and the trigeminal nerves being the most common nerves involved [6].
Facial palsy forms an important defining component of Heerfordt’s
syndrome. Its approximate incidence in this syndrome is 25-50%. However,
its lack doesn't t eliminate the diagnosis as we have noticed in our
case, in which the diagnosis of Heerfordt’s syndrome was made based on
the association of other highly suggestive criteria such as uveitis and
parotitis.
The combination of both uveitis with blurred vision and facial nerve palsy could be performed as sarcoidosis [7].
As it is obviously noted in the literature that eye involvement was the
most consistent finding in patients presenting with Heerfordt’s
syndrome, along with unilateral or bilateral facial palsy or parotid
gland swelling [1]. Glucocorticosteroids remain the first- line therapy of Heerfordt’s syndrome [1].
This case emphasizes the importance of recognizing
the main signs and clinical symptoms which may be quite modest to
indicate the diagnosis of this syndrome.
Conclusion
Head and neck manifestations of Heerfordt’s syndrome
are non-specific and a high suspicion is required to diagnose the
condition early. In our case, Heerfordt’s syndrome was retained before
the association of parotitis and uveitis confirmed subsequently by the
histological examination. The presence of peripheral facial paralysis is
not necessary to make the diagnosis and must not delay its management.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment