Tourniquet Pain after Ultrasound-Guided Axillary Blockade-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Objective: To analyse tourniquet pain after
ultrasound guided axillary block (AXB) as the sole anesthetic technique
with no injection of local anaesthetic into the subcutaneous tissue of
the posterior half of the axilla to prevent tourniquet pain.
Material/patients and methods: 84 patients
older than 18 years ASA I-IV undergoing surgery at hand, wrist, forearm
and elbow under ultrasound guided AXB requiring upper arm tourniquet, we
studied prospectively. Exclusion criteria included refusal to
participate, communication problems, pre-existing neuropathy,
coagulopathy or allergy to local anaesthetics. Tourniquet pain was
assessed according to visual analogue scale (VAS) every 15 minutes. We
also analysed differences in tourniquet pain between sedated and
non-sedated patients.
Main results: VAS was 0 during ischemia in 83
patients. One patient reported tourniquet pain. This was mild (VAS = 3)
and reported during the first 15 minutes of ischemia. VAS dropped to 0
from then on. The median ischemia time was 62 minutes (IQR 45-86) and
the median surgery time was 60 minutes (IQR 40-89.5). Intraoperative
sedation was administered to 48.8% of patients. Sedated and non-sedated
groups were similar. No statistical differences were found regarding
tourniquet pain between both groups (p< 0.05).
Conclusion: Ultrasound guided AXB is
sufficient to provide anaesthesia for tourniquet even during prolonged
ischemia. However, to ensure prevention of tourniquet discomfort a
multiple injection technique that include musculocutaneous blockade
should be preferred.
Keywords: Tourniquet pain; Axillary block; Ultrasound-guided peripheral nerve block; Upper limb surgery; Sedation
Background
Regional anaesthesia holds potential advantages when
compared to general anaesthesia. Particularly, brachial plexus blockade
has demonstrated superior analgesia, reduction of opioid-related side
effects and opioid consumption during the first 24 hours after surgery [1]. The axillary blockade (AXB) provides anaesthesia for upper extremity surgery of the elbow, forearm, wrist, and hand [2,3]. It has been shown as effective as supraclavicular (SCB) and infraclavicular (ICB) blocks [4] but its distal location from pleura and phrenic nerve eliminates some of the risks related to those more proximal approaches [5,6].
Ultrasound guidance allows direct observation of
nerves, surrounding structures and local anaesthetic (LA) spread. Its
use decreases complications and onset time [7,8], improves quality [8] and reduces the volume of LA required [9].
Due to the superficial location of the brachial plexus in the axilla,
ultrasound guided AXB provides excellent visibility of both nerves and
needle.
The intercostobrachial nerve (T2) is not part of the
brachial plexus. It communicates with the medial brachial cutaneous
nerve (C8-T1) providing innervation to the skin of the axilla and the
medial and posterior aspect of the arm. The block of these nerves to
prevent tourniquet pain is widely extended and has been traditionally
recommended using an injection of LA into the subcutaneous tissue of the
posterior half of the axilla ("semicircular subcutaneous anaesthesia"
or "ring block") [1014]. However, its importance in reducing tourniquet pain has never been established and is questioned [2,15,16].
The aim of this study was to assess tourniquet pain after ultrasound
guided AXB as the sole anaesthetic technique. Due to the fact that
intraoperative sedation could underestimate tourniquet pain, further
analyses comparing tourniquet pain in sedated and nonsedated patients
were also carried out.
Material and Methods
A prospective observational study of tourniquet pain
on patients who received an ultrasound guided AXB was conducted over a
four month period (January- May 2013) at Galdakao- Usansolo Hospital.
The study was classified as service evaluation and no ethical approval
was needed as required no alteration to the routine standard of care,
there was no therapeutic or equipment intervention, and no planned
change to anaesthetic technique. Written consent from patients was
obtained. Inclusion criteria were patients undergoing surgery at or
below the elbow under ultrasound guided AXB requiring upper arm
tourniquet, age >18 years and ASA (American Society of
Anaesthesiologists) status I-IV. Exclusion criteria were refusal to be
included, communication problems or inability to cooperate, pre-existing
neuropathy, coagulopathy or allergy to LA.
After patient arrival to theatre an intravenous
catheter was placed in the upper limb contralateral to the surgical site
and ASA standard monitoring were applied. Ultrasound guided AXB were
performed by either consultants with expertise in regional anaesthesia
or residents supervised by those consultant. A portable ultrasound
machine (Sonosite M-Turbo®) and high frequency linear probe was used.
Administration of premedication or intraoperative sedation was left to
the discretion of the treating anaesthesiologist. The ultrasound probe
was applied in the axilla to obtain a short-axis view of the axillary
artery. The four terminal nerves (median, ulnar, radial and
musculocutaneous nerve) were sought out and their identity confirmed by
scanning distally along the arm following the characteristic course that
each nerve takes. A 22 gauge needle (Braun Stimuplex D) was used to
surround each individual nerve with LA after skin infiltration with
lidocaine 1% (Figure 1).
The AXB approach (in plane or out of plane) and the type and amount of
LA was decided by the anaesthetist who performed the block.
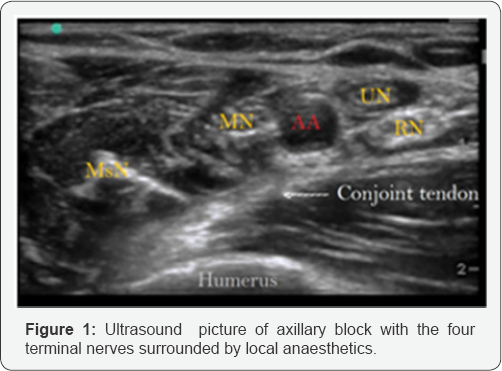
AA: Axillary Artery; RN: Radial Nerve; UN: Ulnar
Nerve; MN: Median Nerve; MsN: Musculocutaneous nerve; Conjoint tendon of
the latissimus dorsi and teres major
Once the block was finished, a pneumatic tourniquet
was applied to all patients on the mid-upper arm over a single wrap of
cotton wool padding. The limb was exsanguinated using an Esmarch bandage
and the tourniquet cuff inflated between 250- 300mmHg.
The variables collected included age, gender, weigh,
ASA status, type of surgery, premedication administered, type and amount
of local anaesthetic used to surround each nerve, time between the end
of the block and the tourniquet inflation, pressure of the tourniquet,
ischemia and surgery time, intraoperative sedation and tourniquet pain.
The primary objective was to analyse tourniquet pain assessed according
to a 0-10cm visual analogue scale (VAS), whereby '0' represents no pain
and '10' represents the worst imaginable pain. Tourniquet pain was
measured directly after the tourniquet was inflated and thereafter every
15 minutes (min) until the tourniquet was deflated. VAS evaluations
were conducted by the same person who performed the block. As a second
objective we analysed differences in tourniquet pain between
intraoperative sedated and non-sedated patients.
Statistical analysis
Descriptive analysis of socio-demographic and
clinical variables was made by using frequencies and percentages for
categorical variables and means and standard deviations for continuous
variables. The exception being variables with a high level of deviation.
These were represented by median and interquartile range. The
differences between sedated and non-sedated patient were evaluated using
the Chi-square test (or Fisher exact test when expected values<5)
for categorical variables and non-parametric Wilcoxon test for
continuous variables. All effects were considered significant at
p<0.05. All statistical analyses were performed using SAS for Windows
statistical software, version 9.2 (SAS Institute, Inc., Carey, NC).
Results
Over the four month period 84 patients were recruited.Patient characteristics and type of surgery are summarized in Table 1.
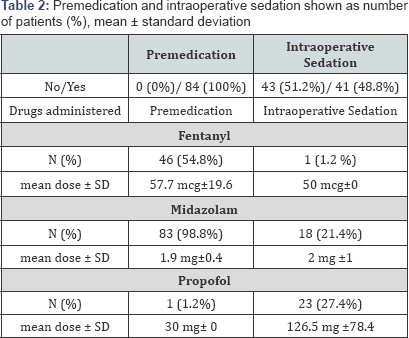
All patients received premedication prior to the block. Intraoperative
sedation was administered to 48.8% of patients. Sedatives used to sedate
patients during surgery were propofol and midazolam but one patient
received 50 mcg of fentanyl (Table 2).
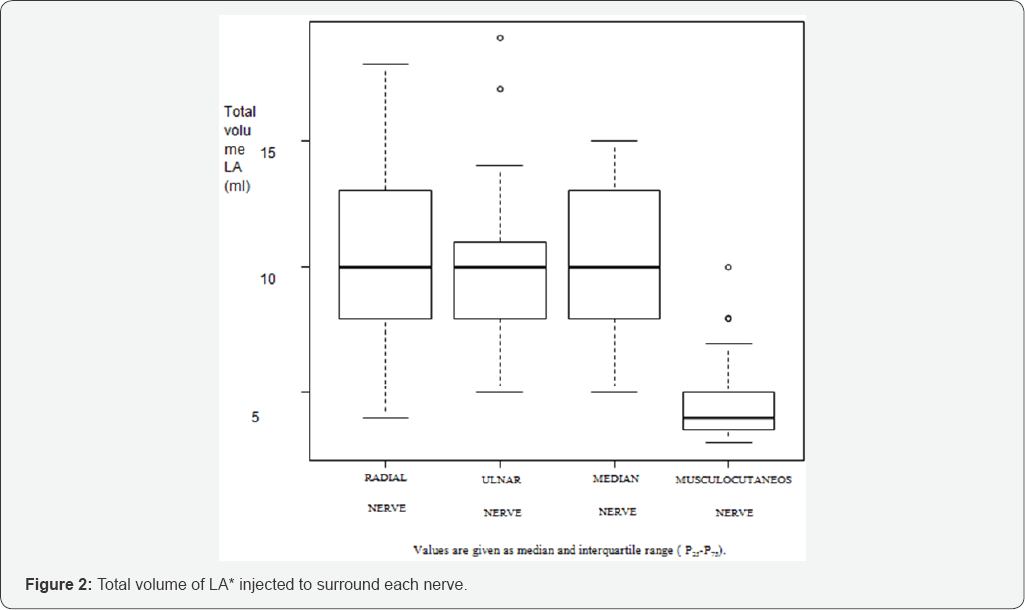
Mepivacaine 1.5% were the LA of choice to surround the four nerves in
all patients. Occasionally Ropivacaine 0.2% or Levobupicaine 0.25% were
added to provide longer analgesia. The mean total volume of LA used was
34.37±5.37 ml (Figure 2).


The median time since the block was finished until
the cuff was inflated was 10min (IQR 5-15). The median surgery time was
60 min (IQR 40-89.5) and the median ischemia time was 62min (IQR 45-86) (Table 3).
Among 84 patients included, 83 scored tourniquet pain
as VAS = 0cm during the time tourniquet was inflated. One of these
patients complained about pain in the surgery field without pain on the
tourniquet site after 180min of surgery and had to undergo general
anaesthesia. In this case, a 30min reperfusion period was used after
135min of ischemia and the total ischemia time with the patient awake
was 150 min. One patient reported tourniquet pain. In this patient VAS
was 3 cm when the cuff was inflated and in the following 15 minutes. He
was administered 50mg of fentanyl and 20mg of propofol respectively.
Since then VAS reminded 0cm until the tourniquet was deflated 31 minutes
later. No more sedatives were administered.
Sedated and non-sedated groups were similar in
demographic variables, ASA status, premedication administrated, type of
surgery, type and amount of LA used, time of ischemia and surgery and
tourniquet pressure. No statistical differences (p< 0.05) were found
regarding tourniquet pain between both groups (Table 4).
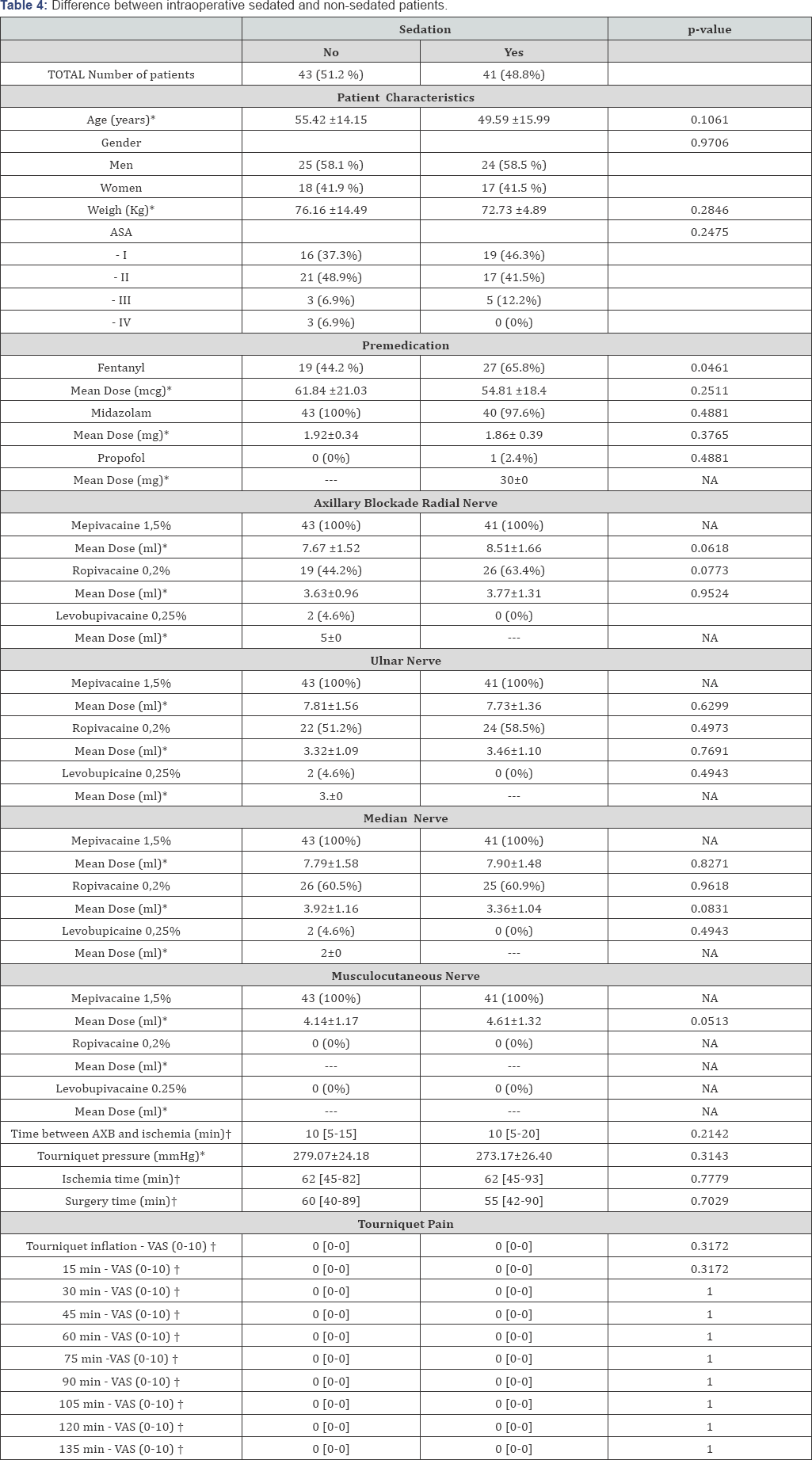
ASA: American Society of Anaesthesiologists; AXB: Axillary Block; VAS: Visual Analogue Scale;
Results shown as number of patients (%). *mean ±
standard deviation (SD). †Median [Interquartile range = p25-p75]. NA =
Not applicable. --- = Unknown.
Discussion
Tourniquets are commonly used in upper limb
procedures to improve visualisation, reduce bleeding and expedite
surgical procedures. Despite its advantages, tourniquet might associate
injury that usually involves nerve or other soft tissues and is often
complicated by the development of tourniquet pain [17].
Contrary to the old belief that a dermal component represents one of
the major causes of tourniquet-related pain, ischemia and compression
have been identified as the main sources of noxious stimuli during the
maintenance of tourniquet inflation [18-21].
Due to these findings, there is progressively more belief that during
AXB a tourniquet is well tolerable without requiring additional dermal
anaesthesia [15,16]. Similarly, popliteal blockade is sufficient for tourniquet on the caff with no need of femoral or saphenous block [22]. It is important to highlight the importance of achieving a "complete" AXB [23]. Pain associated to tourniquet has been showed to be significantly reduced when a multiple injection AXB technique is used [24]. S. Sia et al. [25]
comparing a triple injection AXB technique (blockade of median,
musculocutaneous and radial nerves) and a "selective" approach in which
only the nerves involved in surgery were blocked, reported a significant
increase of patient requesting intraoperative administration of
fentanyl for tourniquet pain in the "selective" group.
Despite the numerous anatomical variations of the
four main nerves at the axilla, median, ulnar and radial nerves they all
lie very close to the axillary artery [25].
Due to this proximity, the injection of a determinate amount of LA to
block one of them could cause blockage of the others. By contrast,
musculocutaneous nerve lies far lateral to the axillary artery, in the
fascial plane between biceps brachii and coracobrachialis muscle. It
innervates the muscles in the anterior compartment of the arm - the
coracobrachialis, biceps brachii and the brachialis. To achieve its
block the needle has to be redirected but its blockade is essential to
prevent tourniquet pain [26].
We identified the four nerves by scanning distally along the arm and
observing the nerve tracing. They were surrounded by LA independently.
Among 84 patients, 83 reported "no pain" [27].
Only one patient complained about tourniquet discomfort (VAS= 3cm)
during the first 15 minutes but VAS dropped to 0 cm from then on. This
is more likely to be attributed to a block in progress than to a real
need of additional blocks. Time between block finished and cuff
inflation was just 3 min in this patient whereas, Tran DQ, et al. [28] concluded that the mean onset time is 18.9 minutes when using 4 injections AXB and lidocaine 1.5% with epinephrine 5mcg/ml.
The use of sedation in regional anaesthesia has been
shown to increase patient satisfaction and can also modify pain
perception [28,29]. However, there were no differences in tourniquet pain between intraoperative sedated and nonsedated patients in our study.
Tourniquet pain has been related to the duration of inflation [18]. Five of our patients had ischemia for more than 120min but none of them complained about tourniquet pain. JP Estebe et al. [30],
reported a tourniquet pain tolerance of approximately 2030 minutes in
volunteers. Tolerance was defined in that study when VAS was > 6cm or
when volunteers decided their pain tolerance limit was reached. In
daily practice, letting patients reach either points is unacceptable.
Patients on the operating table suffering a painful experience could
lead to anxiety, patient movement and unsuccessful surgery. Therefore if
a tourniquet is required for surgery, associated pain should always be
prevented and treated.
Fitzgibbons PG et al. [31]
carried out a review regarding safe tourniquet use recommended
tourniquet pressure of 250mmHg for less than 150min in the upper
extremity. We used tourniquet pressure slightly higher and only one
patient exceeded a total ischemia time of 150min, however a reperfusion
time was used on this patient. Although higher pressures and longer
ischemia times than the ones recommended have not demonstrated increased
complication [32],
tourniquet-related injury resulting from excessive tourniquet inflation
pressure or prolonged ischemic time were not an objective of our study
and were not followed up. Some of the limitations of this study included
a relatively small number of patients, observational methodology and
nonrandomized design. Test of sensory and motor blockade were not
recorded, but no incomplete blocks were reported. No blinded observer
data was collected. Ultrasound guided AXB alone provides enough
anaesthesia to cover tourniquet-related pain even during prolonged
ischemia. Use of additional dermal blocks are not required, however a
multiple injection AXB technique that ensures musculocutaneous blockade
should be performed.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment