Clinical Efficacy of Clonidine versus Fentanyl as Spinal Adjuvant to 0.5% Hyperbaric Bupivacaine for Knee Arthroscopy under Subarachnoid Block- A Comparative Evaluation-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Background: Neuraxial techniques are
safe and possess many benefits with drawback of short duration of
anesthetic action. A small mass of local anesthetic can produce profound
and reproducible surgical anesthesia. The present was aimed to compare
the clinical efficacy and safety of clonidine versus fentanyl as spinal
adjuvant to 0.5% hyperbaric bupivacaine for knee arthroscopy.
Patients and Method:Sixty adult
patients of American Society of Anaesthesiologists (ASA) physical status
I and II of both genders, aged 18 to 58 years, were randomized into two
groups of 30 patients each to receive either with 0.5 ml of clonidine,
30 μg (Group I BC) or 0.5 ml of fentanyl, 25 μg (Group II BF) with 3.5
mL0.5% hyperbaric bupivacaine. Sensory and motor block characteristics
and time to first rescue analgesic (i.v. tramadol 100 mg) were recorded
as primary end points. Drug related side effects of pruritus, nausea,
vomiting and respiratory depression were recorded as secondary outcomes.
Results:The onset of sensory and
motor block, cephalic dermatome extension, and the time to two dermatome
regression were prolonged in patients of clonidine group with
statistical significant difference (p=0.039). Duration of analgesia was
also extended in patients of clonidine group (283.00 ± 40.18 min vs
231.50 ± 46.18min in fentanyl group) with statistically highly
significant difference. Intraoperative hemodynamic changes were
comparable and no medication was required. Mild pruritus observed in 5
patients of fentanyl group. Post spinal shivering, nausea, vomiting and
respiratory depression did not occur in any patient.
Conclusion:Clonidine 30 μg as spinal
adjuvant to 0.5% bupivacaine was clinically more efficient than
fentanyl for potentiating the block characteristics and enhancing the
postoperative analgesia.
Keywords: Bupivacaine; Clonidine; Fentanyl; Knee arthroscopy; Subarachnoid blockIntroduction
Subarachnoid block is commonly used regional
anesthetic technique for patients who require surgical anesthesia for
lower extremities, perineum, pelvic girdle or lower abdomen. It
may be useful in patients with difficult airway or suffered from
co-morbidities of severe respiratory disease. Spinal anesthesia
covering the mid-thoracic level yields a contracted small intestine
to provide superior surgical conditions in combination with profound
muscle relaxation of abdominal muscles.
Local anesthetic reversibly blocks the nerve conduction by
blocking the sodium and potassium ion channels in the nerve
membrane. Blockade of neural transmission in the posterior
nerve root fibres interrupts somatic and visceral sensation and
blockade of anterior nerve root fibres prevents efferent motor and
autonomic outflow. Thus local anesthetic progressively inhibits
the transmission of autonomic, sensory and motor impulses,
resulting in sympathetic blockade, analgesia and anesthesia.
Subarachnoid blockade with 0.5% hyperbaric bupivacaine
provides sensory and motor blockade for surgeries lasting for
about 2 hours but co-administration of spinal adjuvants allow
reduction in the required dose of local anesthetics with the
advantage of generating the same degree of analgesia. Several
adjuvants such as opioids and alpha-2 agonists are used to
enhance the onset and duration of spinal anesthesia and sedation
along with their ability to provide enhanced post-operative
analgesia [1].
The highly lipid soluble drugs such as fentanyl and sufentanil
have a more rapid onset than hydrophilic opioids such as morphine.
Fentanyl acts primarily as agonist at μ-opioid receptors to produce
analgesia of long duration and reduces the systemic toxicity by
allowing dose reduction of local anesthetic. But this combination
of local anesthesia with opioids may lead to undesirable effects
of pruritus, nausea, vomiting, urinary retention and respiratory
depression [2,3].
Alpha-2 adrenoceptor agonists are also used as spinal
adjuvant. They act on pre-junctional and post-junction α-2
adrenoreceptors in the dorsal horn of spinal cord. Clonidine is
a centrally acting selective partial α2 adrenergic agonist and
prolongs the duration of sensory and motor blockade by virtue
of its ability to decrease sympathetic nervous system outflow. It
increases the duration of analgesia, intensify the motor block and
prolongs the duration of postoperative analgesia but it can cause
hypotension and bradycardia [4].
Addition of clonidine or fentanyl has been shown to be
beneficial, based on prior studies. In our place, the practice of
spinal anesthesia does not include intrathecal clonidine, though
clonidine is freely available. Intrathecal fentanyl is frequently
administered but the availability of fentanyl is restricted. The
present study may support the prior research of other countries.
The present prospective randomized double blind study
was aimed to compare the clinical efficacy and safety of
intrathecalclonidine versus fentanyl as adjuvant to 0.5%
hyperbaric bupivacaine in patients undergoing knee arthroscopy.
Patients and Method
After approval from Institutional Ethical Committee and
written informed consent, 60 adult patients of American Society of
Anaesthesiologists (ASA) physical status I and II of both genders,
aged 18 to 58 years, weighing 45-85 kg with height of 150-175 cm,
scheduled for elective infraumblical surgery under subarachnoid block, were enrolled for present prospective randomized double
blind study, conducted at Department of Anaesthesiology and
Critical Care, Chattrapati Shivaji Subharti Hospital associated to
Subharti Medical college, Meerut, India.
The patients with history of severe cardiac or pulmonary
disease, poorly controlled hypertension, morbid obesity,
neurologic disease, hepatic or renal dysfunction, metabolic
disorders, and deformity of spinal column, bleeding or coagulation
disorder, known hypersensitivity to study drugs or using any
drug that modifies pain perception or infection at site of lumbar
puncture were excluded from study. Refusal to technique and uncooperative
patients were also excluded from study.
All patients were admitted prior to day of surgery and were
premedicated with tablet alprazolam 0.5mg and tablet ranitidine
150mg on the night before surgery. Six hours fasting was ensured
before the surgery.
All selected sixty patients were randomized into two equal
groups of 30 patients each according to computer generated
random number table. Patients of Group I were given intrathecal
3.5mL of 0.5% hyperbaric bupivacaine with 0.5ml of clonidine
(30μg) and patients of Group II were given intrathecal 3.5mL of
0.5% hyperbaric bupivacaine with 0.5ml of fentanyl (25μg). The
total volume of drug was kept 4mL to ensure the blinding of study.
Study medication was prepared by an anaesthesiologist who was
neither aware of the study protocol nor further involved for data
collection.
After arrival in the operation theatre, standard monitors for
heart rate, electrocardiogram, pulse oximetry and non-invasive
blood pressure were attached for monitoring of vitals parameters.
Intravenous line with 18 G intracath was secured and lactated
Ringer solution was infused at rate of 10mL/kg over 15 minutes,
before initiation of subarachnoid block. Patients were instructed
on the methods of sensory and motor assessments and were
explained regarding the visual analogue scale (VAS) scoring
system.
The subarachnoid block was carried out under all strict aseptic
precaution in sitting position by midline approach at L2-3 or L3-4
intervertebral space using the 25 G Quincke’s spinal needle. After
identification of the correct space, 4 ml of study drug solution
was injected slowly according to group allocation. Immediately
after intrathecal injection, the patient was made to lie supine and
10° Trendelenberg tilt of table was done to achieve the adequate
level of surgical anesthesia (T10 dermatome). All patients were
supplemented with 100% oxygen at the rate of 4L/min via the
venti face mask.
Sensory and motor blockade characteristics
The subarachnoid block was carried out under all
strict aseptic
All time intervals were calculated from the time of end of
intrathecal injection. The sensory and motor block characteristics
were assessed at 2 minute interval till the surgical anesthesia was
achieved. The segmental level of sensory block was assessed by pin prick
method bilaterally along the mid clavicular line using short bevelled
26 G hypodermic needle. The motor block of the lower extremities was
evaluated bilaterally by modified Bromage Scale (0-3): 0 = full movement
and able to raise straight leg against resistance; 1= unable to raise
extended leg at the hip but able to flex knee; 2= unable to flex the
knee but able to move ankle joint; 3= unable to move hip, knee or ankle
(no motor activity).
The subarachnoid block was carried out under all
strict aseptic
The onset time of sensory blockade at T10 dermatome, maximum cephalic
dermatome level, and time taken to two dermatome regression of sensory
analgesia were recorded. Time taken to achieve complete motor blockade
and total recovery time from motor blockade was also recorded. The
surgical anesthesia was considered when T10 dermatome was anesthetized.
The subarachnoid block was carried out under all
strict aseptic
Postoperatively the sensory and motor block levels were assessed at 15
minutes intervals until normal sensations are returned. Duration of
sensory analgesia was taken from onset of spinal anesthesia to time of
administration of first rescue analgesic, reflected on visual analogue
scale (VAS >3).
The subarachnoid block was carried out under all
strict aseptic
VAS is a psychometric response scale and patients specified their level
of pain by indicating a position along a continuous line between two
endpoints of 0 -10 where 0=no pain to 10=worst possible pain.
Hemodynamic parameters
The subarachnoid block was carried out under all
strict aseptic
The hemodynamic parameters of systemic arterial pressure, heart rate,
pulse oximetry and electrocardiography (ECG) were monitored
preoperatively and then at every 5 minute intervals after initiation of
subarachnoid block, till end of surgery and followed by at every 15
minutes interval in postoperative room. For the present study,
hypotension was defined as systolic blood pressure of less than 20% of
base line value or less than 100 mm Hg. It was treated primarily by
increasing the rate of infusion and additionally with bolus of
mephenteramine 6mg intravenously if required further. Bradycardia was
defined as heart rate less than 60 beats per minute and was treated with
intravenous atropine 0.6mg.
Level of sedation
The subarachnoid block was carried out under all
strict aseptic
The sedation score was evaluated by Ramsay Sedation Scale at every 30
minutes considering the time of giving the study drug as zero. Ramsay
Sedation Scale: 1-Patient anxious, agitated or restless; 2. Patient
co-operative, oriented and tranquil alert; 3-Patient responds to
commands; 4-Asleep but arousable with brisk response; 5-Asleep with
sluggish response; 6-Asleep with no response.
Adverse events
The subarachnoid block was carried out under all
strict aseptic
All patients were observed for pruritus, nausea, vomiting, respiratory
depression (defined as respiratory rate less than 10 breaths/ minute),
shivering or any other adverse effects. Respiratory discomfort was
managed by increasing the flow of oxygen. Nausea and vomiting was
treated by intravenous ondansetron (4 mg).
The subarachnoid block was carried out under all
strict aseptic
After the end of surgery, the patients were shifted to the recovery room
and monitored for any changes in vital signs. Postoperative analgesia
was monitored at every 15 minutes interval for the 1st hour and then at
every 30 minute interval for next two hours. Rescue analgesia was given
with inj. tramadol 100mg with ondansetron 4 mg intravenously when VAS
score was ≥ 3.
Study Population Size
The subarachnoid block was carried out under all
strict aseptic
The sample size was calculated with standard computer programme which
computed that approximately 23 to 25 patients should be included in each
group in order to detect at least clinically significant difference of
30 min in mean duration of postoperative analgesia between the groups
for type 1 error of 0.05 with power of 80% and 95% confidence limit.
Assuming a 5% drop out rate, the final sample size was set at 60
patients for better validation of results.
Statistical analysis
The subarachnoid block was carried out under all
strict aseptic
The results obtained in the study are presented in a tabulated manner as
Mean ± Standard Deviation (SD) considering the later as the best
predictor for statistical analysis. Data was analyzed using Stat graphic
centurion, version 16 (Stat point Technologies INC, Warrenton). The
demographic data for categorical variables were compared using
chi-square test and statistical significance in mean difference was done
by using analysis of variance (ANOVA). A p value of 0.05 was considered
to indicate statistical significance.
Results
The present study compared the clinical efficacy and
safety of clonidine versus fentanyl as spinal adjuvant to 0.5%
hyperbaric bupivacaine for subarachnoid block on 60 adult consenting
patients. There was no protocol deviation and study was successfully
completed. Data of all patients were included for statistical analysis.
They were cooperative with subsequent assessment of subarachnoid block
characteristics and VAS score.
The demographic data for age, weight, height, BMI, American Society of
Anaesthesiologist (ASA) physical status classification and duration of
surgery were comparable between the groups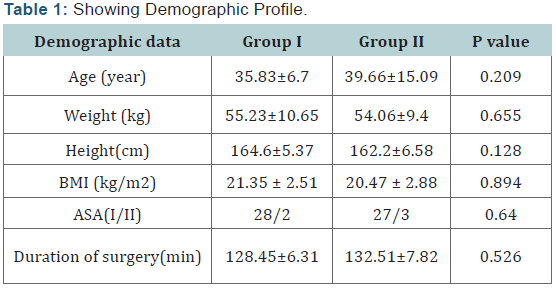
Sensory blockade profile
The subarachnoid block was carried out under all
strict aseptic
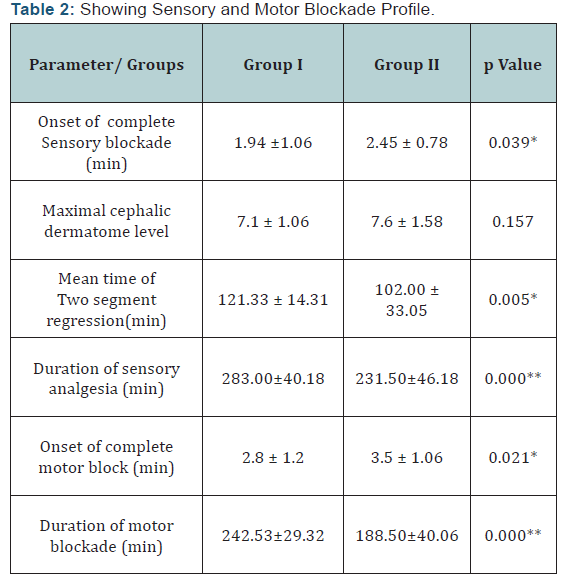
The mean time required to achieve complete sensory blockade was 1.94
±1.06 min in patients of Group I and 2.45 ± 0.78 min in patients of
Group II with statistically significant difference (P=0.039). Mean
maximal cephalic dermatome level was comparable between the groups. Mean
time for two segment regression was 121.33± 14.31 min in patients of
Group I and 102.00 ± 33.05 min in patients of Group II. The duration of
two segment regression varied significantly between the groups (p=0.05).
Mean duration of sensory analgesia was 283.00 ± 40.18 min with
clonidine and 231.50 ± 46.18 min with fentanyl and showed statistically
significant difference (P=0.000) (Table 2).
The subarachnoid block was carried out under all
strict aseptic
Data are expressed as Mean and Standard deviation (SD);*P Value <0.05
is statistically significant; **P value < 0.001 is statistically
highly significant.
The subarachnoid block was carried out under all
strict aseptic
Mean time to achieve complete motor block was 2.8 ± 1.2 min in patients
of Group I and 3.5 ± 1.06 min in patients of Group II with statistically
significant difference (P=0.021). Mean duration of complete motor block
was 242.53±29.32 min in patients of Group I and 188.50±40.06 min in
patients of Group II with statistically highly significant difference
(P=0.000) (Table2).
Hemodynamic profile
The subarachnoid block was carried out under all
strict aseptic
The hemodynamic parameters of mean arterial blood pressure, mean heart
rate, respiratory rate and oxygen saturation at baseline were
comparable.
The subarachnoid block was carried out under all
strict aseptic
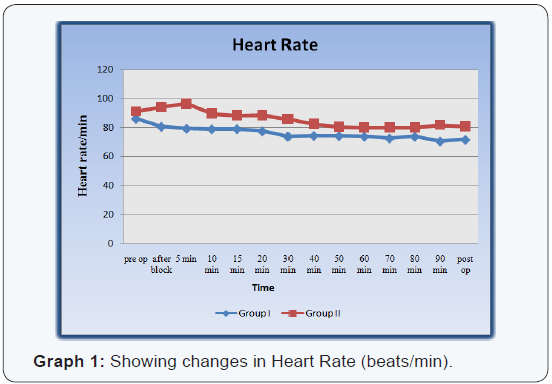
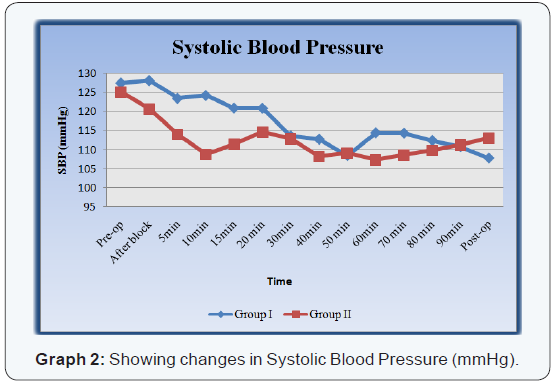
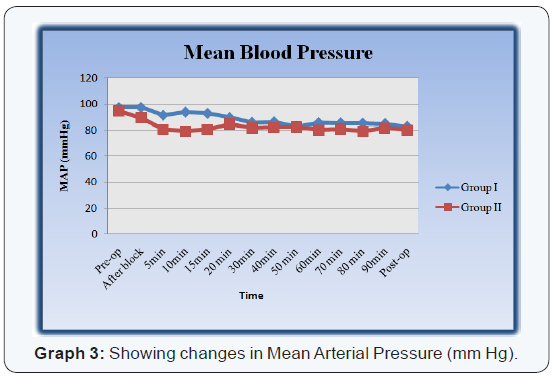
After 5 min of subarachnoid block (SAB), the mean heart rate and mean
systolic blood pressure showed gradual decline in patients of both group
until after 30 min of SAB [Graph 1,2]. After 5 min of subarachnoid
block, the mean arterial pressure of all patients was decreased till 15
min with statistically highly significant difference. Later on, the mean
arterial pressure (MAP) became stable in patients of both groups and
the difference between the groups was comparable. [Graph 3] Incidence of
hypotension and bradycardia during the intraoperative period was
minimal and did not require any medical intervention.
The subarachnoid block was carried out under all
strict aseptic
Sedation score was recorded every 30 min for two hours, considering the
time of study drug given as zero. Mean sedation score was 1.063±0.4 in
patients of Group I and 1.133±0.50 in patients of Group II, which was
comparable (p=0.606), which signifies negligible sedation by clonidine
and fentanyl. All patients were calm and cooperative.
The subarachnoid block was carried out under all
strict aseptic
Mild pruritus was observed in 5(16.7%) patients of Group II which was
successfully treated with intravenous inj. phentermine. The respiratory
rate in patients of both groups was comparable and no episodes of
respiratory depression or tachypnoea occurred in either group.
Peripheral oxygen saturation remained well within normal limits with
mild fluctuations. No patient suffered from post spinal shivering,
nausea, vomiting or respiratory depression. None of the patient needed
supplemented analgesia during surgery.
Visual analogue scale
The subarachnoid block was carried out under all
strict aseptic
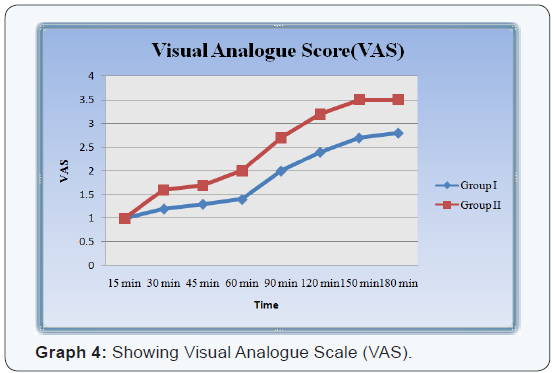
Visual Analogue Scale (VAS) in each patient of Group I and II was
recorded every 15 minutes for first hour after surgery followed by every
30mins for next two hours. The difference in the intensity of pain was
statistically highly significant between the groups. It was higher in
patients of Group II. Rescue analgesia was not required in any patient
till 3 hours after surgery [Graph 4].
Discussion
Neuraxial anesthetic techniques are preferred for
infraumblical surgeries due to rapid onset of surgical anesthesia and
complete muscular relaxation. It is beneficial in patients of
anticipated difficult airway or suffering from comorbid conditions such
as respiratory diseases. The technique is simple, economical, and
reproducible with reduction in the incidences of venous thrombosis. The
postoperative analgesia can be extended by using spinal adjuvants
without affecting their early mobilization.
The subarachnoid block was carried out under all
strict aseptic
In augmentation strategies wide variety of opioids and non-opioids are
used as an adjuvant to subarachnoid block to improve the quality of
block and surgical anaesthesia with prolongation of postoperative
analgesia. Clinical studies have shown that opioids and alpha 2
adrenergic agonist administered intrathecally were able to relieve
visceral pain [5].
The subarachnoid block was carried out under all
strict aseptic
In present study, 17.5mg hyperbaric bupivacaine was used to establish
the subarachnoid block because10mg hyperbaric bupivacaineor less carry a
risk of inadequate block as proven by Pederson et al while generous
dosages guaranteed the effective surgical anesthesia [6]. In the present
study we have used both clonidine and fentanyl as spinal adjuvant to
hyperbaric bupivacaine and achieved a comparable higher level of sensory
blockade. But the onset and duration of sensory and motor blockade
showed statistically significant difference between the groups. The
onset of sensory blockade was rapid and duration of sensory blockade was
enhanced by clonidine when compared to fentanyl.
The subarachnoid block was carried out under all
strict aseptic
The clonidine is lipid soluble and easily penetrates the blood–brain
barrier to provide effective and extended analgesia by binding to
presynaptic C-fibres and postsynaptic dorsal horn neurons. Its analgesic
action is a result of decreased release of C-fiber transmitters and
hyperpolarisation of postsynaptic dorsal horn neurons. The prolongations
of blockmay result from synergism between bupivacaine and clonidine to
motor neurons in the dorsal horn. Intrathecal clonidine has
antinociceptive action for both somatic and visceral pain.
The subarachnoid block was carried out under all
strict aseptic
In our study, clonidine in dose of 30μg was chosen which favoured the
study of Prabha P et al. [7] They concluded that 30μg of clonidine has
significantly increased the cephalic spread and duration of analgesia as
compared to bupivacaine alone [7]. This is also supported by the study
carried out by Chiari et al. [8]. These authors reported that the risk
of hypotension is more with higher dosages of clonidine (150μg).
The subarachnoid block was carried out under all
strict aseptic
Fentanyl is a lipophilic μ-receptor agonist opioid and intrathecal
fentanyl exerts its affect by combining with opioid receptors in the
dorsal horn of spinal cord with supra spinal spread to provide good
perioperative analgesia. We used 25μg fentanyl in another group as
spinal adjuvant to 0.5% hyperbaric bupivacaine for subarachnoid block.
Ramchandra VS et al. [9] also concluded that intrathecal 25μg fentanyl
to bupivacaine provides good analgesia with less sedation and is a
better option where sedation is not desirable [9].
The subarachnoid block was carried out under all
strict aseptic
In present study, the sensory blockade profile was significantly better
in patients with clonidine when compared to fentanyl. Similar results
were also observed by Strebel et al. [10] Gecaj-Gashi et al. [11] and
Singh et al. [12]. They all reported the rapid onset of sensory block in
patients receiving intrathecal clonidine. The mean time of two segment
regression and complete sensory blockade was also significantly
prolonged with clonidine when compared to fentanyl. This was also in
accordance to the study of Tilker et al. [13] who reported that the time
taken for regression of sensory block was statistically higher in
clonidine group [13].
The subarachnoid block was carried out under all
strict aseptic
In our study, the duration of postoperative analgesia showed
statistically significant extension in patients of clonidine group as
compared fentanyl group, which is also supported by the study of Strebel
et al. [10] and Tilker et al. [13] The complementary action of local
anesthetics and α-2 adrenoreceptors agonists accounts for their profound
analgesic properties.
The subarachnoid block was carried out under all strict aseptic
Gupta K et al. [14] studied the analgesic efficacy of intrathecal
clonidine 30μg versus butorphanol 0.20mg during orthopaedic
surgeries. Though both drugs have intensified the sensory
block and increased the duration of analgesia but clonidine was
considered as better alternative to opioids as spinal adjuvant
for orthopaedic surgeries [14]. The onset of motor block was
significantly earlier in patients of clonidine group and our results
are similar to the studies conducted by Singh et al. [12] Strebel et
al. [10] and Gecaj-Gashi et al. [11] However in the study conducted
by Tilker et al, the onset time of motor block was comparable in
patients of both the groups.
The subarachnoid block was carried out under all strict aseptic
In our study, clonidine significantly prolonged the duration of
motor block which is also supported by the studies of Elia et al.
[15] and Jain et al. [16] who reported 0 pain score in clonidine
with bupivacaine as compared to 0.5% bupivacaine alone [16].
The prolongation of the motor block of spinal anesthesia may be
the result of binding of α2 adrenoreceptors agonists to the motor
neurons in the dorsal horn.
The subarachnoid block was carried out under all strict aseptic
Hypotension was observed in 1(3.3%) patient of clonidine
group and 3(10%) patient of fentanyl group which was managed
by increasing the rate of crystalloid solution infusion and
no vasopressor medication was required. It could be due to
adequate preloading prior to institution of subarachnoid block.
Bradycardia did not occur in either group reflecting the safety of
low doses of spinal adjuvant. The results of present study are in
accordance with Singh et al [12] & Nazareth et al. [17]. They also
reported stable hemodynamic parameters in the groups receiving
intrathecal clonidine and fentanyl. No significant changes in the
respiratory rate and oxygen saturation were observed in any
patients of both the groups.
The subarachnoid block was carried out under all strict aseptic
Postoperatively, significantly lower VAS scores were observed
in patients receiving intrathecal clonidine, indicating good
postoperative analgesic effect. Our results are comparable to
those of Strebel et al. [10] Merivirta et al. [18] and Tilkar et al.
[13]. There was no incidence of post-spinal shivering, nausea and
vomiting in either group. All patients were calm and comfortable.
Conclusion
Clonidine, 30μg as spinal adjuvant to 0.5% bupivacaine was
clinically more efficient than fentanyl 25μg for potentiating
the subarachnoid block characteristics and enhancement of
postoperative analgesia. All patients were calm and cooperative
during surgery and no respiratory depression occurred in any
patient. The incidences of hypotension or bradycardia were
comparable and needed no medical intervention.
Limitation of Study
The present study was conducted on patients with stable
cardio respiratory status (ASA I&II). These patients needed spinal
adjuvants to enhance the duration of anesthesia with low dosages
of local anesthetic drug.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment