Postoperative Analgesia by Transmuscular Quadratus Lumborum Block Catheters-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Ultrasound guided Quadratus lumborum (QL) block is a
relatively new regional anesthetic technique which provides effective
postoperative analgesia for abdominal surgeries as a part of multimodal
analgesic regimen. We report a case of hysterectomy where effective
postoperative analgesia was provided by ultrasound guided bilateral QL-3
block and infusion of local anesthetic through catheters inserted
postoperatively.
Keywords: Local anaesthetic;
ropivacaine; Postoperative analgesia; Quadratus lumborum blocks; type-1,
2 and transmuscular (type-3); Truncal blocks; Ultrasound guided blocksIntroduction
Postoperative analgesia is an integral part of
successful surgical outcome. Epidural analgesia with catheter technique
remains the most effective analgesic technique after abdominal surgery.
However, it haslimitation in patients who are either on anticoagulants
and have cardiac morbidity due to significant hemodynamic changes which
may be detrimental to such patients [1,2]. Ultrasound guided Quadratus
lumborum block (QLB) block is a new technique of regional analgesia
[3,4]. There have been reports of excellent post-operative pain
management with the QLB for both abdominal and retroperitoneal surgery
[5,6]. However, postoperative analgesia by bilateral transmuscular
quadratus lumborum blocks (TQLB) or QL-3 block with catheter is rarely
reported. We present a case report where postoperative analgesia was
provided by bilateral transmuscular quadratus lumborum blocks (TQLB) and
infusion of local anaesthetics through inserting catheters ina patient
who had cardiac disease and underwent hysterectomy operation.
Case
A female aged 58yrs posted for abdominal hysterectomy
with bilateral oophorectomy for dysfunctional uterine bleeding and
fibroid. She had coexisting morbidities of rheumatic heart diseases
(mitral valve replacement in 1983 for mitral stenosis), hemiplegia of
left side 1990 (completely recovered), diabetes mellitus, hypertension,
persistent chronic atrial fibrillation and pulmonary hypertension.
Preoperative 2D echocardiography showed moderately stenotic prosthetic
valve, moderate tricuspid regurgitation, mild mitral regurgitation, and
mild aortic regurgitation, dilated left atrium, pulmonary hypertension
and left ventricular ejection fraction 40%. X-rays showed Lower Zone
haziness. Her blood pressure was 160/70 mm Hg, pulse 98/minute
irregular. On auscultation diastolic murmur with metallic clickof
prosthetic mitral valve was present. She was on oral warfarin which was
changed to unfractionated heparin 5000 International units twice daily
5days before the day of surgery. She was also taking antihypertensive,
digoxin, oral hypoglycemic and human act rapid insulin. Laboratory
investigations regarding haemogram, coagulation profile and other
biochemical parameters were within normal limits. An informed consent
about anaesthesia and postoperative analgesia plan was taken. After
overnight fasting on the day of surgery all oral medicines and
intravenous prophylactic antibiotics were given. Blood sugar levels were
monitored 6hrly and insulin dosage were used according to sugar levels.
In operation theatre non-invasive monitoring (ECG,
Oximeter, Noninvasive Blood Pressure) were attached.Under
local anaesthesia and using ultrasound guidanceright sided
internal juglar central venous line was inserted (Linear 6-13
MHz M-Turbo® SonoSite ultrasound system) taking all aseptic
measures. General anaesthesia was induced with intravenous
fentanyl (100 μgm) and 100mg propofol. A size#3 proseal LMA
was inserted and anaesthesia was maintained with 1% isoflurane,
50-50% oxygen-nitrous mixture and vecuronium for muscle
relaxation. Operative course was uneventful except patient
required positive end expiratory pressure (PEEP) of 6 to maintain
saturation above 95%.
After the surgery bilateral ultrasound guided transmuscular
quadrates lumborum (TQL) block was given using curved array
transducer 5–2 MHz (M-Turbo® SonoSite ultrasound system).
In lateral position, the side to be blocked was kept up and
probe was placed in the midaxillary line in the transverse plane
immediately above the iliac crest and then it was slided dorsally
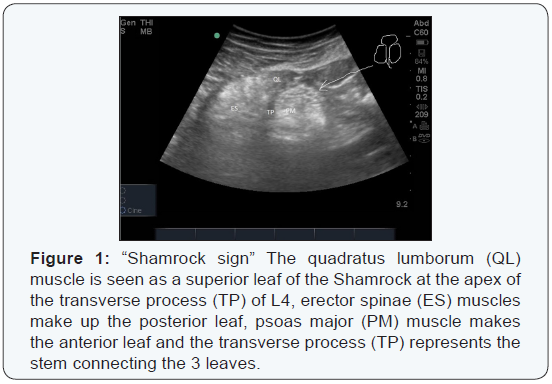
till the Shamrock sign was clearly identified [7]. In “Shamrock
sign” The quadratus lumborum (QL) muscle is seen as a superior
leaf of the Shamrock at the apex of the transverse process (TP) of
L4, erector spinae (ES) muscles make up the posterior leaf, psoas
major (PM) muscle makes the anterior leaf and the transverse
process (TP)represents the stem connecting the 3leaves (Figure
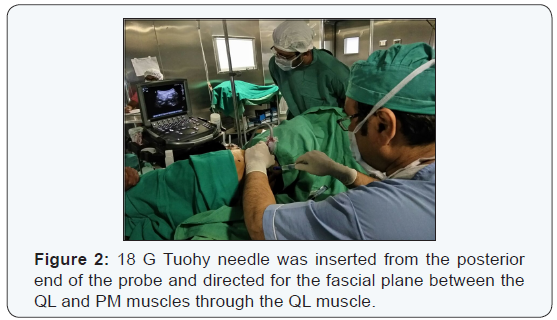
1). 18 G Tuohy needle was inserted from the posterior end of
the probe and directed for the fascial plane between the QL
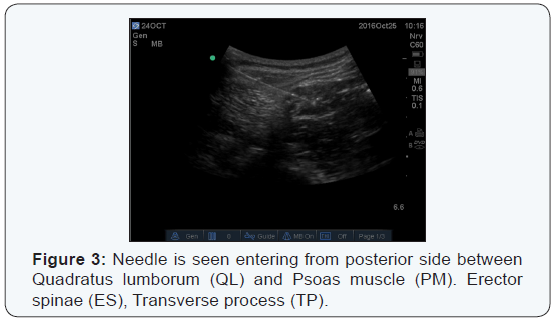
and PM muscles through the QL muscle (Figure 2). Once needle
was confirmed at correct location 25mL 0.3% ropivacaine was
injected [8](Figure 3) and 18G epidural catheter was inserted
3cm beyond the tip and fixed at skin through subcutaneous
tunnel. Other side catheter was also inserted in similar manner.
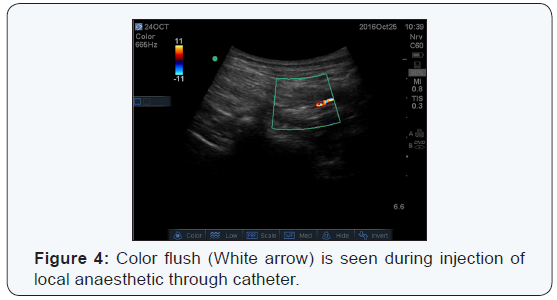
Catheter position was confirmed by injection of local anaesthetic
and using color doppler mode (Figure 4). After reversal patient
was shifted to recovery room. Both the catheters were connected together using a y-connection to a volumetric pump and infusion
of ropivacaine 0.1% and fentanyl 1μg/mL was started @ 14ml/
hour. Additional analgesia was provided by injection paracetamol
1G intravenous 8hrly for first 48 hours and then 12hourly for next
two days. Injection Tramadol 50 mg IV as an when required was
advised for rescue analgesia. Pain scores using Visual Analogue
Scale (VAS)were monitored two hourly for 24 hours and then
4hrly for next 2days. VAS score remain 0-2 on rest (where 0=no
pain and 10=maximum pain) and 0-4 on movement for 3days.
No rescue analgesia was required. Patient also reported high
satisfaction from this technique of pain relief compared to two
previous caesarean section surgery.A contrast study was done
with injection of 5mL contrast (Omnipaque-300®) mixed with
15mL 0.3% ropivacaine which showed spread up to the thoracic
paravertebral space (Figure 4). Catheters were removed after
3days, heparin was tapered and oral anticoagulant was started.
On 5th day patient was discharged home after check dressing.
approach by injecting local anesthetic posterior to
QL (QL block type-2) [9]. He postulated that, injection of local
anasthetic in the facial plane over QL results in extended spread up to
thoracic dermatomes. Carney et al documented through contrast
enhancement from T4 to L2 that, the QL block as an extension of the
local anaesthetic beyond the TAP-plane spreading into the thoracic
paravertebral space with the provision of both visceral and
somatosensory blockade of the abdominal wall [10]. Kadam RV [11]
observed the sensory spread from T8 toL1 in a case of laparotomy done
for tumor excision and have suggested that sensory analgesia is variable
and dependent on many factors including the volume of the drug and site
of injection.
Single injection QL block has been used successfully
for the management of postoperative pain relief after caesarean section
[12] for sub-total gastrectomy in a septic patient [13], laparotomy for
duodenal tumour excision and to manage chronic back pain [14]. The
effective pain relief lasted for 12-14hours. Prolonged and continuous
pain relief has been reported with catheter techniques for acute
abdominal pain management [15] breast reconstruction [16] and laparotomy
[11]. However, they all have used type-2 quadratus lumborum block.
In our case we used a transmuscular approach (QL
block type-3) suggested by Borglum et al. [4] where the local
anaesthetic is injected in the fascial plane between the QL and Psoas
Major (PM) muscles. This technique has more definitive endpoint of
injection and injection into this fascial plane ensured a reliable
spread in to the thoracic paravertebral space (TPVS) [4].The presence of
psoas muscle ahead of needle point also works as safeguard to prevent
inadvertent entry in to the peritoneal space and injury to kidneys.
Transmuscular quadratus lumborum or QL type-3 block
has been used successfully for pain management after caesarean section
[17]. Where 14 hours of effective analgesia was provide by this block.
QL type-3 with catheter has been used effectively to manage pain of hip
arthroplasty in place of epidural analgesia [18]. To our understanding
bilateral catheter technique to provide continuous analgesia is not
reported earlier.
Epidural was an option in our case but on evaluation a relative risk of serious complication we preferred this technique [1,2].
We could achieve effective analgesia by insertion of
bilateral catheter to control visceral as well as somatic pain
postoperatively. However, it would have been interesting to observe
analgesia influence on intraoperative hemodynamics if, catheter would
have been inserted preoperatively.
The unanswered question remains that, which QL block
is more effective? The efficacy of QL block is correlated with spread of
local anesthetic up to the paravertebral space and we have experienced
(unpublished data) that posterior spread of QL-3 is more consistent than
QL-1 and QL-2. This happens because fascia transversalis (FT) covers
the thoracolumbar fascia (TLF), anterior surface of the QL as well as
the antero-lateral surface of the PM [19]. The FT splits in two sheets
at the level of the diaphragm. One sheet becomes the inferior
diaphragmatic fascia and the other sheet passes behind the lateral and
medial arcuate ligaments and continue as endothoracic fascia [20]. Thus,
LA injected in the lumbar region between the PM and QL can spread up to
TPVS [21].
However, there has been no comparative study to suggest one’s superiority over other for safety and efficacy.
Although, QL-3 seems more invasive than QL-2 however,
entry through QL muscle and presence of psoas as a guard in front of
needle make it as a safer choice.
Contrary to QL-1 and QL-2, which can be given in
supine or wedge under hip position. QL-3 requires a lateral decubitus
position and become the major limitation for the procedure even if used
preoperatively because, extra helping hands are required.
We monitored the clinical effect in terms of pain
relief however, sensory spread was not recorded. We feel it was a miss
on our part as it would has helped further studies. This we consider a
limitation of our case report.
Conclusion
In this case report we observed that QL-3 block is an
effective technique for postoperative pain relief after hysterectomy
surgery in a high risk patient. Infusion of local anaesthetic through
catheters inserted during block further helped in continuous pain relief
for desired period. We did not face any complication however, more
studies are required to prove its efficacy and safety in high risk
patients.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment