Using Ultrasound to Confirm Endotracheal Tube Position in the Intensive Care Unit-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Aim: To determine the accuracy
of ultrasound in confirming endotracheal tube placement compared with
standard techniques in the intensive care unit.
Subject and Methods:: This was a
prospectively designed study. Eligible patients were 18 years or older,
that were admitted to the medical intensive care unit, that required
endotracheal intubation due to their underlying clinical condition. An
immediate post intubation Ultrasound examination was performed by an
intensivist, who was not involved in clinical management of the patient
and was blinded to the result of the standard confirmatory methods of
endotracheal tube placement. The clinician performing the intubation was
blinded to the results of the ultrasound examination findings.
Results:: According to the
standard method used to confirm proper endotracheal tube position, which
includes clinical assessment by chest and epigastric auscultation, and a
colometric end tidal CO2 connected to the endotracheal tube, all twenty
patients had a correctly placed endotracheal tube; however, the
post-intubation chest radiograph showed a right main stem intubation in
one patient that was missed by the standard method of confirmation.
Ultrasound examination confirmed the proper placement of the
endotracheal tube in 19 patients, and was also able to detect the right
main stem intubation in that one patient. Based on the results of our
study, the diagnostic accuracy of the ultrasound method in confirming
proper endotracheal tube position was 100% (20/20) and that of the
standard method 95% (19/20).
Conclusion: This study
demonstrates that US imaging has a high diagnostic accuracy to
immediately confirm proper ETT placement post-intubation in an intensive
care unit.
Keywords: Ultrasound (US); Endotracheal tube (ETT) position; Intensive care; End tidal CO2; Chest radiographAbbreviations: US: Ultrasound; ETT: Endotracheal Tube; ICU: Intensive Care Unit; AHA: American Heart Association
Introduction
It is important to confirm proper placement of the
endotracheal tube (ETT) as there is significant morbidity and mortality
associated with inadvertent esophageal intubation [1-3]. Endotracheal
intubation is a frequently performed procedure in an intensive care unit
(ICU) and an intensivist has to be adept at performing intubation and
confirming ETT position [4]. An ideal technique to confirm the position
of ETT is one that provides verification of tracheal location of the ETT
at a level above the carina to ensure bilateral ventilation. The 2010
American Heart Association (AHA) guidelines for adult advanced life
support (ACLS) recommend the use of both clinical assessment and
confirmation devices to verify ETT placement [3].
Visualizing chest expansion, auscultating bilateral
lung fields and epigastrium, along with continuous waveform capnography
is considered the most reliable method of confirming correct
ETT placement. Besides waveform capnography there are other confirmatory
devices, such as, no waveform exhaled carbon dioxide detectors,
esophageal detector devices, and transthoracic impedance detectors.
Direct visualization of the glottis and passing the ETT under direct
vision is considered the gold standard, but in many patients with
difficult airways, it may not be possible to visualize the glottis [5].
Despite all the numerous techniques described to
confirm proper ETT placement, none of the methods are absolutely
reliable, or readily available in many ICU’s [3,6]. Waveform capnography
is unreliable in patients with low pulmonary blood flow, airway
obstruction, low cardiac output states, and epinephrine use [6]. A
routine practice in most ICU’s is to obtain post-intubation chest
radiography to confirm the location of ETT above the carina [7].
Chest radiographs take time to be performed and are not very
helpful for immediately confirming a proper position of the ETT.
With the rise in use of point-of-care ultrasound to assess
patients in ICU’s, ultrasound machines are readily available in
most ICU’s [8,9]. Sonographic confirmation of correct ETT position
has been described in adults, with either direct visualization of
the tracheal tube [10-14], indirect signs of ventilation, such as
bilateral pleural sliding [15] and diaphragm motion [16-19] or
both [20]. An ultrasound (US) examination can be performed
immediately and rapidly after intubation, with great accuracy to
confirm ETT position [21].
We conducted a pilot study with a goal to determine the
feasibility of US to confirm ETT position immediately post
intubation, prior to the chest radiograph. The study design was
approved by the institutional review board (IRB), and a waiver for
informed consent was obtained as an emergency situation made
it infeasible to obtain the same.
Material and Methods
This was a prospective, double blinded, and single center
pilot study conducted at our Medical Intensive Care Unit. Eligible
patients were 18 years or older intubated emergently in the
ICU due to their underlying clinical condition. Exclusion criteria
included patients with subcutaneous emphysema, pneumothorax,
a history of pneumonectomy and pleurodesis. US imaging for
pleural sliding is not technically feasible in these patients, as
the US waves tend to reflect strongly wherever air meets tissue
secondary to high acoustic impedance.
An anesthesiologist or an intensivist performed the
intubation and confirmed the proper position of the ETT using
the standard method. All patients were sedated and paralyzed for
intubation. The standard method in our ICU to assess proper ETT
location immediately post-intubation includes the use of clinical
assessment and a colometric end tidal CO2 (ETCO2) detecting
device (Easy Cap II, Nellcor Inc., Hayward, CA). The ETCO2
detector connects to the end of the ETT and a persistent color
change from purple to yellow after five breath cycles is accepted
as a verification of correct placement of ETT. A chest radiograph is
then performed and interpreted by the clinician who intubated the
patient to confirm ETT’s location above the carina. An immediate
post intubation US examination was performed by an intensivist,
who was not involved in clinical management of the patient and
was blinded to the result of the standard confirmatory methods of
ETT placement, and the clinician performing the intubation was
blinded to the US examination findings.
US images were obtained using MicroMaxx (Sonosite
Inc.,
Bothell, WA) machine with a 5-8 MHz curved array transducer. The
examination was performed at a level just above the suprasternal
notch in transverse and longitudinal views (Figure 1). A
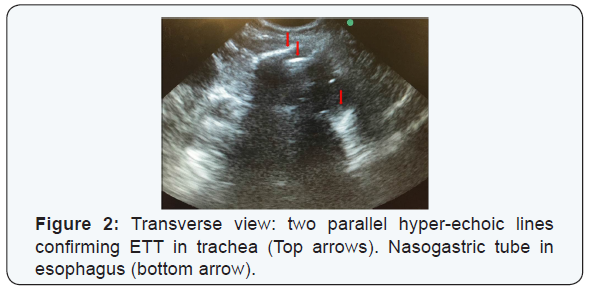
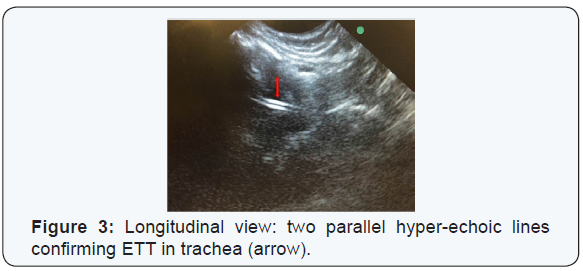
confirmation of a tracheal presence of ETT was interpreted as [1]
the presence of two parallel hyper-echoic lines in the transverse or
longitudinal images (Figure 2&3) [2] a non-intubated or empty
esophagus. By moving the probe laterally it can be confirmed
whether the esophagus is empty or distended by the ETT, as an
ETT in the esophagus gives a similar image as when in the trachea.
Presence of hyper-echoic lines laterally to the trachea, but absent
in the trachea, confirmed an esophageal intubation indicate that
the ETT is outside the trachea [22].
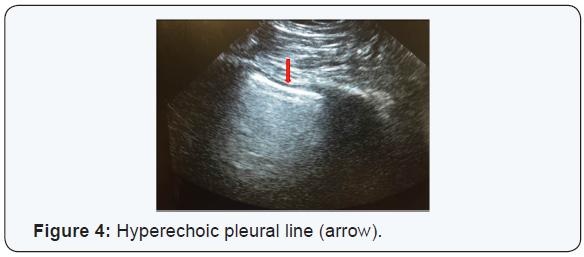
Bilateral presence of pleural sliding on US examination was
used as an evidence of ETT location above the carina. To confirm
pleural sliding, the probe was placed in the 3rd of the 4th intercostal
space bilaterally and the presence of a hyper-echoic line
moving with respiration indicates that the lung is being ventilated
(Figure 4). All US examinations were performed by the same
intensivist trained in the use of point-of-care US in managing ICU
patients.
The clinician performing the intubation completed a
data collection sheet post-intubation, which recorded the indication for
intubation, intubation difficulty scale score (Cormack-Lehane scale)
[23], size of the ETT, the confirmatory methods of ETT position and the
chest radiograph findings. The intensivist performing the US examination
recorded the US findings on a separate data collection sheet, which
included the interpretation of the images for tracheal presence and
pleural sliding. These two data sheets were then stored in a secure
location for later analysis.
The null hypothesis of our study was that there is
no difference in the diagnostic accuracy of the standard method and the
US method for immediate confirmation on proper ETT position. Fischer’s
exact test was used for analysis. Statistical analysis was performed
using Graph Pad Prism version 6.04 for Windows (Graph Pad Software, La
Jolla California USA).
Results
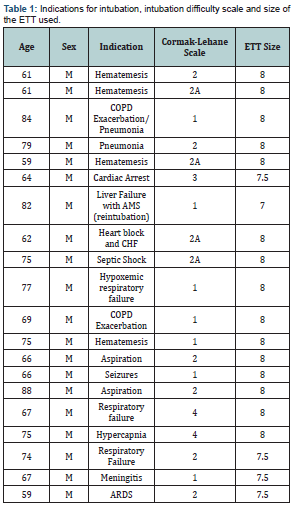
All patients in the study were males with an average
age of 70.5 years. The indications for intubation, intubation difficulty
scale and the size of the ETT is shown in Table 1. As per the standard
method used to confirm ETT position, all twenty patients had a correctly
placed ETT, but the post-intubation chest radiograph showed a right
main stem intubation in one patient that was missed by the standard
method of confirmation. US examination confirmed the proper placement of
the ETT in 19 patients and was able to detect the right main stem
intubation in that one patient. Hence the diagnostic accuracy of the US
method was 100% (20/20) and that of the standard method 95% (19/20),
with a p value of 1.0. The sensitivity and ppv of the US method was 100%
(CI 79.9 - 100%), and the standard method had a 100% (CI 79.1 - 100%)
sensitivity and 95% (CI 73.1 - 99.7%) ppv.
Discussion
The 2010 AHA guidelines for ACLS recommend the
use of clinical assessment and confirmatory devices to verify ETT
position [3]. Clinical assessment includes auscultation of the chest and
epigastrium and observing chest rise with ventilation, but these
methods have been shown to be unreliable [7], and esophageal intubation
has been shown to go undetected in 0.4-15% [1,3]. In the event of
cardiac arrest, clinical assessment methods require an interruption of
chest compressions, which is not, recommended as per the AHA guidelines
as it decreases the perfusion time [3]. A chaotic noisy environment
during cardiac arrest, or an obese patient can result in inaccurate
clinical assessment.
ETCO2 detection with either semi-quantitative or
quantitative methods has been shown to be a reliable method for
confirming a tracheal position of ETT, with quantitative waveform
capnography considered the goal standard method [3,22]. But, these
devices, especially waveform quantitative capnography are not routinely
available in many ICU’s [24,25]. ETCO2 detection can be severely limited
in conditions of low pulmonary blood flow or airway obstruction [6]. In
these situations it can result in a false negative finding, which can
lead to unnecessary reintubation attempts.
Insertion of an ETT with direct visualization of the
glottis and viewing the ETT as it passes through the vocal cords is the
gold standard method to confirm a tracheal position of the ETT. But, in
patients with difficult airways, one may not be able to visualize the
vocal cords, and the tube can get dislodged prior to securing the
airway. Also, just relying on direct visualization of the vocal cords
can miss a main-stem intubation. Therefore, each method has its
limitations and intensivists have to rely on several methods immediately
post-intubation to confirm a proper position of the ETT.
US can be a very useful adjunct to the standard
methods of confirming proper ETT position. Point-of-care US use has
risen significantly in the critical care field over the last decade
[8,9], and US machines are now readily available in most ICU’s. There
have been several studies describing the utility of US in assessing
proper ETT position [5,10-12,14-16,18,24-26]. A prospective study
evaluating the accuracy and timeliness of US compared to quantitative
waveform capnography showed a 98.2% (CI 93.7- 99.5%) accuracy of the US
method and a median operating time of 9 seconds [19]. The same
investigators showed that US is a very accurate method to confirm ETT
position in patients with in and out of hospital
cardio-pulmonary-resuscitation (CPR) [20]. The use of US during CPR has
advantages, as its use does not involve interruption of chest
compressions, unlike the clinical assessment method. US images are not
affected by poor perfusion or airway obstruction, as would the methods
used to detect ETCO2, which rely on perfusion for delivery of carbon
dioxide to the lungs. In their study there were five patients with
tracheal intubation who were falsely determined to have esophageal
intubation by waveform capnography resulting from low perfusion state
[19]. Intensivists use US routinely to evaluate critically ill patients
or those undergoing CPR for potentially reversible causes, and US to
assess ETT position can be quickly performed, without interrupting
resuscitation.
Studies with US have used different methods to
confirm ETT position, which can be divided into direct and indirect
methods. Direct methods involve confirming a tracheal location of the
ETT by imaging the trachea, either in real-time as the ETT is passing
through the vocal cords into the trachea, or after intubation
[10,11,13,14]. ETT in the trachea produces two parallel hyper-echoic
lines with posterior shadowing. An esophageal intubation, as described
by Drescher et al., was best seen in transverse views as a second airway
lateral to the trachea [22]. In the study by Werner et al. the
esophagus was noticed to be in the left lateral location in 29 of the 33
patients [14]. Relying on the direct method, one can miss a main-stem
intubation, which most likely will be seen on a chest radiographs done
post-intubation. But, chest radiographs post-intubation take time and it
can result in a delayed diagnosis of main-stem intubation, which can be
detrimental in patients with severe hypoxemia or pneumothorax on the
same side as the tube [27].
Indirect methods utilize presence of lung
ventilation, as ascertained with pleural sliding or diaphragm motion, as
evidence of correct ETT location [15-18,28]. With ventilation the
visceral and parietal pleural surfaces slide against each other, which
on US imaging is seen as a hyper-echoic line moving with respiration
[9]. Pleural sliding by itself may not be the best method to confirm
correct ETT position as pleural sliding maybe absent due to reasons
other than an improper ETT location. Prior scarring of the pleura,
pneumonectomy, atelectasis etc. can result in absent pleural sliding and
can result in a false negative finding of an improperly located ETT.
Patients not paralyzed during intubation can have spontaneous breaths,
which can result in pleural sliding and an impression of a correctly
placed ETT, when it might be in the esophagus. Similarly spontaneous
breaths can produce diaphragm motion and can result in a false positive
finding of correct ETT position, and in patients with paralyzed
diaphragms it will be difficult to interpret findings.
In this study we showed that the US method had a
perfect diagnostic accuracy, and that our hypothesis stays, concluding
that there is no difference in the diagnostic accuracy between the two
methods. The US method should be done sequentially, with tracheal US
verifying a tracheal location of ETT followed by evaluation for pleural
sliding and/or diaphragm motion bilaterally. Relying on just one method
can lead to errors in judgment. We are not recommending that the US
method replace, but, rather be used as an adjunct to the standard
methods to confirm ETT position. ICU’s without ETCO2 detectors, patients
with difficult airways, low perfusion states with likelihood of errors
in capnography etc. are some of the situations where the US method can
be useful. Immediate detection of a misplaced tube with US would help
prevent inadvertent ventilation with AMBU-bag, stomach distention, and
possible vomiting and aspiration.
There are several limitations to our study
and the results cannot be generalized. The study has a small sample size
with a high rate of successful intubations, with no esophageal
intubations. A high rate of successful intubation makes it difficult to
compare techniques and interpret results. It is a single center study
involving a single expert user of the US method, hence the results
cannot be generalized to centers lacking the same expertise. The
strength of the study is that it was a prospective double blind study,
performed on patients in clinical emergencies in the ICU rather than in a
controlled environment on cadavers. This study suggests that ultrasound
can be used in the immediate post intubation period to quickly confirm
the ETT position, while still waiting for the chest radiograph to be
performed. In some instances, chest radiograph is not immediately
available to confirm ETT position, prolong time to ETT position
confirmation maybe problematic in those critically ill tenuous patients
in which inappropriate ETT for prolong periods might lead to
complications. In summary, US confirmation of ETT position should be
used as adjuvant to chest radiograph not as a replacement.
Conclusion
US imaging is an accurate method for immediate
confirmation of ETT position in an intensive care unit and can be a
useful adjunct to the standard methods of confirmation. In the event
that capnography is unavailable, US can be a handy tool to verify ETT
position.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment