Quality Indicators to Assess the End-of-Life Care in the Intensive Care Unit-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Objectives: Intensive Care Units (ICU) in Hong
Kong incorporated palliative care in the daily practice. We would like
to evaluate the quality of end-of-life care (EoLC) in the ICU.
Design, setting and participants: Quality
indicators consist of 4 domains and 12 indicators were devised. The four
domains were early identification of dying patients; communication and
information; end-of-life care to the patient and care after death. Next,
we applied these indicators to assess the EoLC of patients who died in a
20-beds mixed ICU from 1st Jul to 30th Sep 2012.
Main outcome measures: The 12 EoL quality indicators
Results: Out of the 38 patient records, 33
were included for analysis. There were no objective criteria to identify
dying patients. All the studied families received an EoL
physician-family conference. Although high documentation rate (90.9%) of
the treatment plan and resuscitation status; only 3.0% of the family
conferences addressed the psychological, social and religious needs. No
written information was used. Medication was prescribed in 46.7% for
symptom control and life-sustaining treatments (LST) were withheld and
withdrawn in 90.9% and 45.5%, respectively. In indicated patients, only
66.6% had the process reviewed. Lastly, care after death was
acknowledged in 48.4%.
Conclusion: These 12 EoL quality indicators
were specific designed for ICU patients and easy to implement. Areas for
improvement included early identification of dying patients; training
on assessment of the social, psychological and religious needs of the
patient's family; distribution of information leaflets; assessment and
management of symptoms; and regular review of the process.
Keywords: End-of-life issues; Intensive care; EoLC Abbreviations: VHA: Veterans Health Administration; LCP: Liverpool Care Pathway; EoL: End of Life; LST: Life-Sustaining Treatment
Introduction
End-of-life care is an integral part of care in ICU
especially when treatments fail to accomplish the original goal of
treatment. Uncertainty of disease prognostication was one of the
challenges in EoLC in ICU, and the decision was usually based on the
number of organ failures or selected diagnosis like global cerebral
ischemia after cardiac arrest [1,2].
As most critically ill patients were either sedated or unconscious, the
decision making process invariably involved the patient's family.
Symptom assessment and management in ventilated and sedated patients
posed another challenge of EoLC in the ICU. In order not to unduly
prolong the dying process, withholding or withdrawal of life-sustaining
treatment (LST) usually preceded the death of patients in ICU and it
varied from 0-70% [1,3,4].
In Hong Kong, the EoLC was provided by the ICU team who incorporated
palliative care in the daily practice. In order to evaluate the quality
of the care provided to the dying patients in the ICU, we search for
quality indicators used for this particular group of patients.
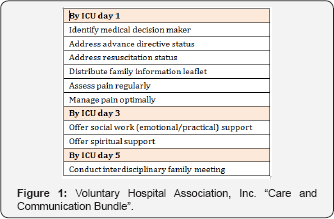
In United States (US), "Care and Communication
Bundle" proposed by Veterans Health Administration (VHA) had been used
to assess the quality of EoLC in the ICU [2,5]. In this bundle, they used Day of ICU admission as the trigger for initiation of end-of-life discussion (Figure 1). However, this practice might not suit our local setting. In Unit Kingdom (UK), the Liverpool Care Pathway (LCP) [6]
had served as the main mechanism to ensure quality of EoLC, especially
in the last days of life. The LCP had 3 key sessions (initial
assessment, ongoing assessment and care after death) and 4 key domains
of care (Physical, psychological, social and spiritual). As LCP had
attracted a lot of criticism, the Independent Review Panel recommended
its use be abandoned [7].
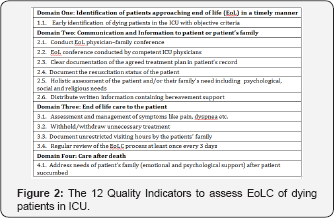
By referring to the quality indicators used from these two countries,
we try to devise a quality tool comprising of 4 domains, namely
Domain One: Identification of the patients approaching end-of-life in timely manner
Domain Two: Communication and information to patient or patient's family
Domain Three: End-of-life care to the patient
Domain Four: Care after death
Under these 4 domains, there were total of 12 indicators as shown in Figure 2. We then applied these 12 indicators to assess the EoLC in a group of dying patients in the ICU.
Method
Prior Ethics Committee approval was obtained to
retrieve the records of patients who died in ICU from 1st Jul to 30th
Sep 2012. End of life (EoL) physician-family conference was defined as
the family interview in which the ICU doctor brought up the issue of
comfort care with the patient's family and the signing of the hospital
DNAR (Do Not Attempt Resuscitation) form. Patients excluded from the
analysis were those who had no close relatives identified; those
families who refused the end-of-life care and patients with unexpected
deterioration in the ICU.
The other data collected include the demographic
data, the APACHE II and IV score, the SOFA score at the time of the EoL
decision, the time from ICU admission to the decision of EoLC, and the
time from activation of EoLC to the death of the patients.
We used these 12 indicators to assess the quality of
EoLC in the ICU. Descriptive statistics were used when appropriate. The
results were expressed as percentages. The denominator was all the ICU
patients with EoLC in the ICU and the numerator refers to the episodes
that fulfilled the criteria.
Result
A total of 38 patients died in the ICU and 5 were
excluded from analysis. Three patients had unanticipated deterioration;
one patient had no close relatives in Hong Kong and one family requested
active treatment until the patient succumbed.
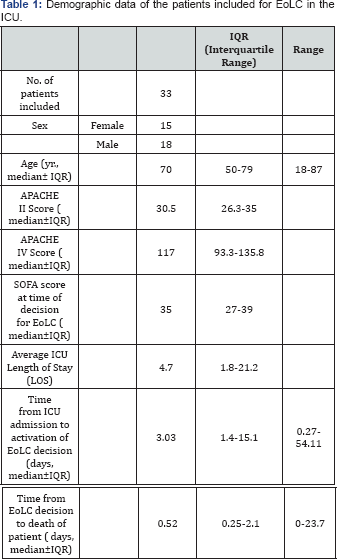
The demographic, APACHE II and IV score of the 33 patients were shown in Table 1.
The median SOFA score at the time of the decision for EoLC was 35
(IQR=27-39); signifying the patients had high probability of dying at
time of decision.
There were no objective criteria for early
identification of patients approaching end-of-life. The median time from
ICU admission to decision of EoLC was 3.0 days (IQR = 1.4-15.1). The
median time from decision of the EoL to death of patient was short and
variable (median of 0.52 days, range from 0 to 23.7 days). Although EoL
physician-family interviews were provided to the family of the dying
patients in the ICU, 84.8% were conducted by an ICU specialist or higher
ICU trainees. There was high rate (90.9%) of documentation of the
treatment plan and resuscitation status of the patients (Table2).
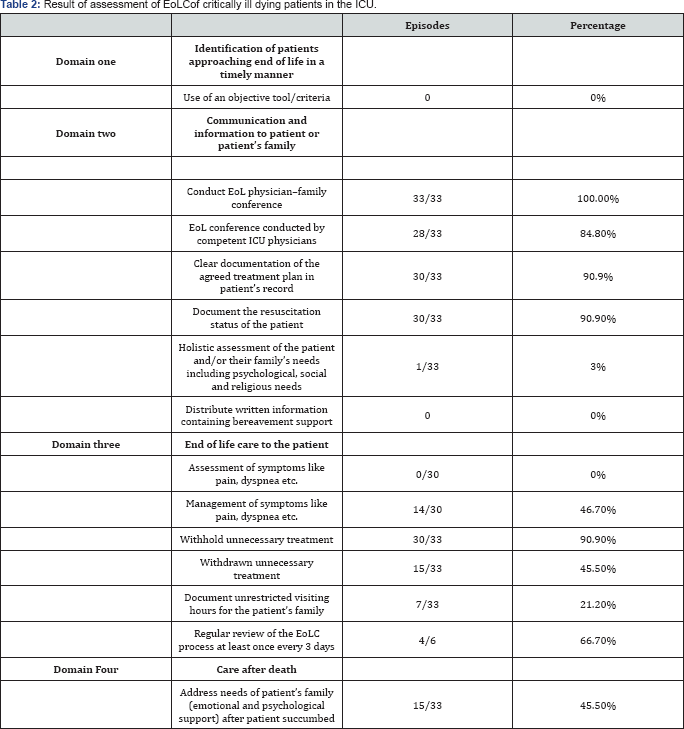
For management of symptoms, 3 patients were excluded
because of severe brain injury. Out of 30 patients, 14 (46.7%) were
prescribed medication for symptom control. There was no formal
assessment of symptoms. Treatment were withheld in 90% of patients had
and less than half (45.5%) had treatment withdrawn. Among the patients
with treatment withdrawn, 5 had ventilator support decreased; 5 had
inotrope decreased; 8 had stopped dialysis support and 6 had unnecessary
medications stopped. Six patients survived more than 3 days after
initiation of the EoLC; 4 of them (66.7%) had the process reviewed again
(Table 2).
As for the patients' families; the areas that were
least assessed were the psychological, social and religious needs of the
patients’ families. We did not have any written information to provide
to the patients' families to explain the meaning of end- of-life care.
Although unrestricted visiting hours were allowed for the family, this
was recorded in the documentation in 7 out of 33 EoL records. After the
patient succumbed, the hospital had its own policy on last offices and
handling of the deceased’s body. However, the needs of the patient's
family was acknowledged in less than half of the cases (45.5%) (Table 2).
Discussion
Between the "Consultative Model" and the "Integrated Model" of palliative care service provision in the ICU [2],
most Hong Kong ICUs have adopted the latter model. In a study by Yap et
al, almost all ICU doctors in Hong Kong would apply the
"Do-Not-Resuscitate" order; 99% and 89% of them would withhold or
withdraw therapy in dying patients, respectively [8]. In general,
limitation of therapy was applied when we were quite confident that the
patient would die or had no chance of meaningful recovery. In order to
evaluate the EoLC in the ICU, we need to identify the quality indicators
that reflect the whole process of care; from identification of dying
patients to care after death. Indeed, implementation of palliative care
quality measures had been regarded as one of the most promising
strategies to improve EoLC service [5].
In the UK before 2014, the Liverpool Care Pathway (LCP) [6] had served as the main mechanism to ensure quality of EoLC, especially in the last days of life [9]. However, there were limited experiences of using the LCP for EoLC in the critically ill patient [10]
. For indicators that were specific to ICU, the Robert Wood Johnson
Foundation Critical Care End-of-life Peer Workgroup proposed the use of
seven domains and 53 quality indicators [11].
To facilitate the use of these indicators in daily practice, the
Veterans Health Administration (VHA) developed the "Care and
Communication Bundle" and narrow down to nine measures [2]. In contrast to most ICU in US,ICU admission in Hong Kong was limited by bed availability [1,8].
Hence, the use ICU stay Days 1, 3 and 5, as the trigger for EoLC might
not be applicable to us. With some modification, we chose 4 basic
domains and 12 indicators to assess the quality of EoLC in our local
settings.
The importance of the "diagnosis of dying" has been brought up by the recent independent review of the LCP and another study [7,9,12].
In Buckley's study, instead of listing the objective criteria to
identify the dying patients in the ICU, they retrospectively reported
the reasons for initiating a discussion on limitation of therapy with
the family [1].
In Buckley study, the mean time from ICU admission to the EoLC decision
was 7.8 +/- 13 days. In our study, the median time for ICU admission to
the decision for activation of EoLC was 3 days (IQR=1.4-15.1 days).
Both studies shown a wide variation in the timing of bringing up the EoL
discussion. The inherited uncertainty in disease trajectories and
prognostication of non-malignant disease [13]
has made the identification of triggering factors rather difficult in
critical illness. Although there were reported triggering criteria for
activation of palliative care consultation [2,14], there were no
unifying objective criteria for early identification of dying patients
among critically ill patients. This may lead to wide variation in the
decision to activate EoLC.
After the implementation of the Care and
Communication Bundle in ICUs in the US, the overall reported pain
assessment and management in three ICUs had improved to 76% and 81%
respectively [15].
In this current study, all the patients were intubated, rendering the
assessment of pain and other symptoms more difficult. In 46.7% of
indicated patients, medications were prescribed for symptom relief.
Assessment of symptoms was important as some patients (e.g. those with
severe brain injury) might not need medication for pain relief while
those who needed them might not have the medication prescribed to meet
their need. Lastly, after the start of the EoL care program, it was
important to have regular reviews of the patients who survived longer
than expected.
In the ICUs at US, the assessment or offering of social and spiritual support ranged from 30-61 % [15-17].
In this study, there was a scarcity of such support to patients'
families both before and after the death of the patient. One study has
shown that the use of a brochure on the subject of bereavement together
with a proactive family conference could enable the families to feel
supported and to decrease the Post-Traumatic Stress Score 3 months after
the death of the patient [18]. Holistic care for the family of critically ill patients during EoLC was one of the major areas for improvement in our ICU.
The limitations of this study were it was a small
retrospective case series; the indicators used were not validated in
other studies; and it only reflected the perspective and practice of
EoLC among the Chinese at Hong Kong. Easy to implement quality
indicators were important as they might help to highlight the quality
gap in EoLC in the ICU. With the use of these indicators, it helped to
identify any missing links between the translation of guideline or
policy into quality care to critically ill dying patients in the ICU.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment