Thoughts on Pain Management, Postoperative Nausea and Vomiting (PONV) & Brain Fog-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Introduction
Persistent anesthesia problems may be summarized as
over- and under-medication, pain management, and postoperative nausea
and vomiting (PONV).
Over- &Under-Medication
Prior to the 1996 FDA approval of a direct cortical
responsemonitor (DCRM), determination of anesthetic dose relied on body
weight, medical & physical assessment (i.e. ASA status), and heart
rate (HR) and blood pressure (BP) changes, especially thesevital signs
changes occurring with initial incision.
The cerebral cortexis the target of anesthetics. The
adult brain weighs approximately 3-4 pounds and doesn't vary
substantially with body weight.Average body weight doses based on the
'70 kg' patient will likely over or under-medicate many patients. ASA
status is also an unlikely guide to individual cortical responses to
body weight based drug doses.
Pharmacokinetics (PK) and pharmacodynamics (PD) as well as target controlled infusion (TCI) are alternative, yet indirect,
measures of cortical response by way of predicting anesthetic blood
levels. These approaches would be acceptable if blood levels, not the
cortex, were the anesthetics' target.
Vital signs (i.e. HR and BP) are brain stem
functions. The American Society of Anesthesiologists’ (ASA) awareness
with recall study showed that half of patients who experienced awareness
had no change in either HR or BP with which to alert their
anesthesiologist [1].
This finding was not an especially surprising since consciousness,
memory and pain perception are cortical, not brain stem, functions.
Under-medication is estimated to occur in only 0.1%
of patients and may result in PTSD in them. Unpleasant an experience as
awareness with recall can be, there are no documented cases of death
from anesthesia awareness. Many of the remaining 99.9% of patients may
be subjected to routine over-medication ( Figure 1).
Not only does one American patient every day perish
(mortality) from anesthesia over-medication but also 16M of the 40M
patients (40%) every year emerge with 'brain fog' (morbidity) [2].
Brain fog may be defined as delayed anesthetic emergence, but also can
include postoperative cognitive dysfunction (POCD) or even delirium [3-5].
Postop brain fog creates additional morbidity while
adding substantial additional costs to the health care system caring for
patients who cannot be quickly processed and discharged from the
system. Additionally, patients must endure the long-term consequences of
their anesthesiologists’ short term care.
The DCRM has been validated in over 3,500 published
studies and can be found in 75% of US hospitals. The question remains
'why is directly measuring the organ being medicated with a DCRM monitor only routinely done 25% of the time?’
Part of the answer may lie in the manner in this
monitor was originally configured. On a unit-less scale of 0-100, the
lower the number, the more sedated the patient. This number is a derived,
not directly measured, value. The 15-30-second delay from real time
places the anesthesiologist in the unfavorable position of catching up
to patient needs instead of being able to anticipate them. This creates a
situation like trying to drive one's car with only the rearview
mirror's information, not especially safe or useful ( Figure 2).

The first anesthesia textbook with a DCRM monitor on its cover also displayed the electromyogram (EMG) of the frontalis muscle (akin to the EKG of the cardiac muscle) in the picture ( Figure 3).
The text described the utility of this real-time signal; i.e. EMG
spikes signal incipient arousal and the need to proactively increase
sedation to return the EMG to baseline [6]. All that is needed to display the EMG is to use the existing software to select and save it as the secondary trend.

Most patients achieve propofol sedation adequate
enough to prevent awareness and recall at 60<BIS<75 (with baseline
EMG) level of with 25-50 mcg-1 .kg'1 .min. Over 18-years’ experience titrating propofol with DCRM, variation of as little as 2.5 mcg-1 .kg-1 .min and as much as 200mcg-1 .kg-1
.min has been observed to achieve the same level of amnesia and
sedation. ‘Apples’ to ‘apples’ comparisons between patients, despite the
nearly hundred-fold observed variation in propofol requirements
to achieve, become more meaningful when using numerically based
definitions of levels of consciousness achieved [7].
Postoperative brain fog likely is a multi-factorial
problem. Until universal DCRM monitoring becomes a standard of care, it
will not be possible to clarify the role routine over-medication plays [8].
It is unlikely beneficial for elderly patients to routinely administer
30% more than what is needed to achieve 60<BIS75. Common sense is
uncommon ( Figure 4) - Voltaire.
Pain Management
Most people know it does no good to close the barn
door after the horses have escaped. But too many anesthesiologists still
need to be convinced that it’s futile to try to prevent postop pain by
allowing surgeons to cut without first blocking the midbrain N-methyl,
D-aspartate (NMDA) receptors [9,10].
Local anesthetic skin injection or incision is an extremely
potent signal to the brain that the "world of danger" has invaded the
"protected world of self." The sedated brain can’t differentiate between
the mugger’s knife and the surgeon’s scalpel (or trocar). While there
are certainly other internal pain receptors, no signal is more
determinant of post-operative pain than of skin incision (or skin
injection). An unprotected incision sets off the major cortical
alarmsthat initiate the wind-up phenomenon.
Surgery is a painful experience.Most
anesthesiologistsbelieve acardinal function is the prevention of pain
during surgery. From 1975 through 1993, this author had never once
considered why there was a need for postop opioid rescue for many, if
not most, patients. In 1992, a clinical trial began using 50 mg IV
ketamine, 2-3 minutes prior to stimulation AFTER propofol hypnosis to
dissociate patients for pre-incisional local anesthesia injection [11,12].
When propofol is incrementally titrated ketamine hallucinations are eliminated [13]. For elective surgery, customary propofol increments are 50 mcg-1.
kg repeated either to loss of lid reflex/loss of verbal response or to
60<BIS<75 with baseline EMG. This DCRM level is usually attained
within 2-3 minutes. Starting with such an apparently homeopathic
propofol dose quickly allows the anesthesiologist to determine an
extremely sensitive patient and avoid prolonged emergence and, likely,
less brain fog.
The benefit of incremental induction is creating a
stable CNS level of propofol to protect from ketamine side effects,
preservation of spontaneous ventilation, maintenance of SpO2, and not creating the difficult airway [14]. Incremental propofol induction most commonly preserves the tone in the masseter, genioglossus and orbicularis oris muscles, maintaining a patent airway. Absent a propofolbolus induction, baseline blood pressureis also maintained.
After observing the first 50 cases emerge without opioid rescue, it was reasonable to concludethe principle reason patients have pain after surgery is that they've had pain during surgery. The lack of opioid rescue continued over the next 1,214 patients [15] and through to the present day of more than a total 6,000 patients.
Dissociation, or immobility to noxious stimulation,
results from mid-brain NMDA blockadelmmobility (i.e. dissociation) has
beenconsistently observed in 100-pound female patients and 250-pound
male patients with the same 50 mg ketamine dose.
Why does the effective dissociative dose of ketamine
not appear to be related to body weight? The adult brain weighs
approximately 3-4 pounds and doesn’t vary with body weight. The midbrain
is a very small part of the adult brain, and the NMDA receptors are a
very small part of the midbrain. Pre-stimulation NMDA block denies the
cortex the knowledge of the intrusion of the outside world of danger.
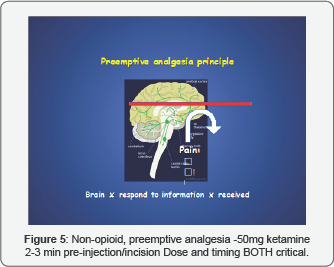
Cognitive dissonance generated by thelack (or
dramatically) reduced opioid rescue with pre-stimulation ketamine dose
is so great that many, if not most, anesthesiologists will need to
observe 10-20 cases to believe them. However, the PACU RNs will notice
more quickly. Surgeons and patients' family members will be as impressed
as the recovery personnel.Once the patient is protected as described
above, the non-opioid, 50mg ketamine ‘miracle’ is achievable with
propofol sedation, regional analgesia/propofol sedation, and general
inhalational anesthesia ( Figure 5).
Postoperative Nausea & Vomiting (PONV)
Much has been written about postoperative nausea and
vomiting (PONV). In 1996, Apfel identified the four most predictive PONV
factors; namely, non-smoking, females, history of PONV, planned use of
postoperative opioids [16]. Apfel subsequently referenced Friedberg's 1999 study [15] in his PONV chapter [17,18].
Apfel's PONV chapter is number 86 of 89 chapters in Millers' Anesthesia.
While patients do not die from PONV, they only wish they were dead.
Greater importance to PONV needs to be heeded by our profession as
patient satisfaction now plays a role in government and other third
party reimbursement.
The data for this five-year review documenting a 0.6%
PONV rate (i.e. 7 of 1,264 patients) were collected by 1997 but not
published until 1999 [15].
These patients turned out to be an Apfel-defined high PONV risk patient
population that received no anti-emetics! No intra-operative opioids or
inhalational ('stinky gases') agent were used [19]. Postoperative opioids were routinely prescribed but rarely used.
Analgesia was provided with adequate local
analgesia. Spontaneous ventilation was preserved using only a single
respiratory depressant, propofol, and scrupulously avoiding
intra-operative opioids. no patients received neuromuscular blocking
agents. This left the possibility of patient movement.
Patient movement under sedation is usually the cause
for great stress on all involved with the surgery, especially the
surgeon who may have pre-operatively injected the operative field with
syringes of lidocaine and epinephrine. Observing vasoconstriction, the
surgeon (incorrectly) surmises adequate analgesia is present and clamors
for more sedation.
The anesthesiologist usually responds with a request
for additional analgesia. Tempers rise leading to the inappropriate
addition of opioids, benzodiazepines etc. or worse, the abandonment of
sedation in favor of general anesthesia (GA) with muscle relaxants. None
of these maneuvers treat the movement most accurately.
The presence or absence of an EMG spike on the DCRM enables a dispassionate
discussion of what the patient most accurately (and minimally) needs to
return the patient to the desired motionless condition. In the pre-DCRM
era, all patient movement was treated as if it could be awareness and
recall. As seen with the headless chicken, a brain is not necessary to
generate movement ( Figure 6).
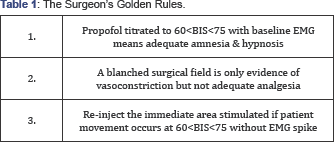
There exists no spinal reflex that can stimulate the EMG of the forehead frontalis muscle. Patient movement without an EMG spike can only be generated by sub-cortical stimulation. This Surgeon's Golden Rules ( Table 1)
needs the anesthesiologist’s time preoperatively with the surgeon to
assure success without increasing the known risks of GA. This author
believes it is very difficult to accept GA risks for patients having
surgery without medical indication; i.e. elective cosmetic surgery. A
more enlightened approach is possible using the absence of the EMG spike
with patient movement to refute the notion that the patient is 'too
light' ( Figure 7) ( Table 1).
Conclusion
When you can measure what you are speaking about, and
express it in numbers, you know something about it; but when you cannot
measure it, when you cannot express it in numbers, your knowledge is of
a meager and unsatisfactory kind; it may be the beginning of knowledge,
but you have scarcely, in your thoughts, advanced to the stage of
science.
William Thompson, knighted Lord Kelvin.
Popular lectures and addresses 1891-1894
Less is more. - Mies van Der Rohe
Without direct cortical measurement of anesthetic
effect, neither science nor minimally trespassing on patients’
physiology will occur. Predictably, problems like over and
under-medication, postoperative pain management and PONV will continue
to plague anesthesiologists and their patients while incurring avoidable
costs. Propofol measurement to 60<BIS<75 with baseline EMG
obviates the perceived need of the commonly used 2 mg midazolam
premedication. Eliminating midazolam also eliminates prolonged emergence
in sensitive and/or elderly patients.
Direct cortical response measurement enables
anesthesiologists to treat patient requirements as the individuals they
are as opposed to the 80% of patients in the middle of the bell curve.
Doing so eliminates outliers, transforms every patients’ ‘mystery’ into
an ‘open book test,’ and creates the basis for more humane, cost
effective anesthesia care.
Over twenty-five years and in more than 6,000
patients, there has not been a single hospital admission for brain fog,
postoperative pain management or PONV. Friedberg’s Triad does indeed
appear to answer anesthesia’s persistent problems.
Acknowledgment
Dr. Friedberg is the president and founder of the
nonprofit Goldilocks Foundation. Neither he, nor the foundation,
receives financial support from brain monitor makers. Dr. Barry
Friedberg has been interviewed extensively about anesthesia and propofol
by FOX, CNN, True TV, and People Magazine during the MichaelJackson
murder trial. A board-certified anesthesiologist for 39 years, Dr.
Friedberg developed propofol ketamine (PK) anesthesia in 1992 and made
PKnumerically reproducible with the addition of the anesthesia brain
monitor (aka Goldilocks anesthesia) in 1998. He has been published and
cited inseveral medical journals and textbooks and was honored with a
U.S. Congressional award for applying his methods on wounded soldiers in
Afghanistan and Iraq.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment