Comparison of Neonatal Apgar Score & Umbilical Artery Blood Gas Parameters Among parturients Undergoing Elective Caesarean Section Under Spinal, Epidural & General Anaesthesia: A Prospective Randomized Observational Study-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Introduction: Frequency of lower segment caesarean
section (LSCS) is increasing today. All anaesthetic techniques used for
LSCS may have certain advantages & disadvantages that affect short
and long term neonatal outcome. This study aimed to compare effect of
spinal, epidural and general anaesthesia on neonatal outcome in terms of
Apgar score and umbilical arterial (UA) blood gas parameters.
Method: Total 90 parturients belonging to age group
of 20-30 yrs of ASA grade I and II who were scheduled to undergo
elective LSCS were randomly allocated by chit method into three groups
(n=30). Group SA received spinal anaesthesia, Group EA received epidural
anaesthesia and Group GA received general anaesthesia. Duration between
induction to skin incision (I-SI), skin incision to delivery (SI-D) and
uterine incision to delivery (UI-D) were noted. Intraoperative vitals
like HR, SBP, DBP, RR, SPO2 and ETCO2 at various time intervals were
recorded. Neonatal UA blood gas parameters (pH, PO2, PCO2, HCO3, BE) and
Apgar score (at 1 and 5 minutes) were assessed after delivery of baby.
Result: Demographic profiles of parturients were
comparable. Intraoperative episode of hypotension found more in group SA
than group EA and GA. Mean Apgar score at 1 min, mean UA blood pH and
PO2 were significantly low and mean UA blood PCO2 was significantly high
in group SA and GA as compared to group EA (p<0.05) but difference
in Apgar score at 1 min, mean UA blood pH, PO2 and PCO2 were
statistically insignificant between Group SA and GA. (p>0.05) Mean
Apgar score at 5 min, mean UA HCO3 and BE values were statistically
insignificant and comparable among groups. (p>0.05).
Conclusion: All three anaesthetic techniques were
safe for neonates in elective LSCS, but epidural anaesthesia was
associated with better short term neonatal outcome as compared to spinal
and general anaesthesia for elective LSCS.
Keywords: Spinal; Epidural; General anaesthesia; Apgar score; UA blood gas analysisAbbreviations: LSCS: Lower Segment Caesarean Section; UA: Umbilical Arterial; I-SI: Induction to Skin Incision; SI-D: Skin Incision to Delivery; UI-D: Uterine Incision to Delivery
Introduction
Lower segment caesarean section (LSCS) is a
life-saving procedure for the parturient and her baby. The frequency of
caesarean section continues to rise steadily worldwide [1]. Today, caesarean delivery accounts for more than 30% of all births [2]. In India the incidence of LSCS is increased from 3% to10% between 1992-93 and 2005-06 [3].
Anaesthesia to a parturient affects both mother and fetus, so
anaesthesiologist has to look over both individuals. The type of
anaesthesia administered for LSCS is an important determinant of the
short term and long term maternal and neonatal outcome. Each anaesthesia
method for elective LSCS has their own advantages and disadvantages to
both mother and neonate. Anaesthesiologist must choose the type of
anaesthesia that is safe for mother, have least depressant effect on
neonate and provides optimal working conditions for the obstetricians [4].
The spinal anaesthesia is commonly used method for LSCS, because of
simple and quick technique, requires low volume of drugs for induction,
less or no systemic effects to the baby, low risk of maternal pulmonary
aspiration and an awake mother at the time of delivery but associated
with high risks of an extensive block, fixed duration of anaesthesia,
post-dural puncture headache and high incidence of maternal hypotension
followed by decrease uterine blood flow in placenta, thus impair fetal
acid base status even in an existence of a normal placental store [5-8].
Epidural block for LSCS has increased in popularity
due to its benefits like low incidence of maternal hypotension and
neonatal respiratory depression, less or no postoperative pain and
discomfort to mother. Though general anaesthesia is associated with good
control of airway and ventilation, better maintenance of cardiovascular
stability, but the drugs required for general anaesthesia are multiple
and may produce systemic effects in the baby like low Apgar score and
sedation, directly by placental transfer and indirectly by maternal
physiological and biochemical changes. General anaesthesia is also
associated with maternal risks of difficult intubation, pulmonary
aspiration, delayed recovery, nausea and vomiting [9]. The incidence of maternal mortality may reach up to 10% under general anaesthesia [10].
Apgar score and umbilical artery pH known to provide best measures of
neonatal outcome after LSCS under all three types of anaesthesia and
both can be affected by alterations in the cord blood flow with the
delivery process and different anaesthesia techniques [11].
Due to benefits and risks of the different anaesthetic techniques, it
is important to choose safest anaesthesia for good maternal and neonatal
outcomes irrespective of indications of caesarean section.
No ideal anaesthetic method for minimizing adverse
neonatal outcome has yet been described in literatures. Uniform data
available regarding comparative effects of types of anaesthesia on cord
blood gases of neonates in healthy maternal population are limited. So
the aim of present study was to determine the effect of spinal, epidural
and general anaesthesia on neonatal outcome in terms of Apgar score and
umbilical cord blood gas values in elective LSCS. So that we can
standardize the anaesthesia technique for elective caesarean section
that have least effect on neonatal outcome.
Method
This study was conducted in the Department of
Anaesthesiology and Critical care, Pt. J.N.M. Medical College & Dr.
B.R.A.M. Hospital Raipur, C.G, after approval from the institutional
ethics committee. This prospective, randomized, open label observational
study was done in total 90 parturient belonging to the age group of
20-30 yrs, ASA grade I & II, who were scheduled to undergo LSCS
under spinal, epidural and general anaesthesia. The Parturients were
randomly divided by chit method into three groups of 30 parturients in
each group (n=30), Group SA received spinal anaesthesia; Group EA
received epidural anaesthesia and Group GA received general anaesthesia.
Before the study, a power of study was calculated by using software G
Power 3.0.10, taking mean values from the study of Petropoulos G et al [12]
and considering a probability level of 0.05 (α-error) and power of 0.80
(1-ß) yielded a sample size of 30 parturients for each group.
Parturients complicated with following conditions were excluded from the
study: Anaemia (<10gm/dl), severe PIH, placenta previa, abruptio
placenta, oligohydramnios, gestational diabetes mellitus, morbidly obese
(BMI > 40 kg/ m2), major cardiac abnormalities,
congenital malformations, intrauterine growth retardation and fetal
distress. Induction to delivery time >10 minutes, skin incision to
delivery time >8 minutes and uterine incision to delivery time >3
minute were also excluded from the study.
Pre-anaesthetic evaluation was carried out and
written informed consent was obtained either from the parturient or from
her relatives to carry out the procedure and enrolled her in this study
after explanation. In operation theatre multipara monitor (Philips MP
30) was applied to monitor non-invasive blood pressure, ECG, SPO2 and ETCO2.
Intravenous line was maintained by inserting 18 G i.v. cannula in vein
of dorsum of hand. Premedication was given with inj. Ranitidine 50 mg
i.v. and inj. metoclopramide 10 mg i.v. 30 min before induction to all
the parturient. Parturients were induced with particular anaesthesia
according to groups assigned. In group SA, with all aseptic precautions
subarachnoid space was approached at L3- L4 or L4-L5
interspace with 26 G Quincke spinal needle in sitting position. Inj.
Bupivacaine 0.5% (heavy) 2 ml was injected and parturient was placed in
supine position immediately. A tilt of 10-15 degree was given to achieve
appropriate block height. Block height was checked by spirit swab for
temperature sensation. Parturients in group EA were placed in sitting
position and with all aseptic precautions epidural space was approached
and identified by loss of resistance method at L3-L4 or L4-L5
interspace, epidural catheter was inserted, left in situ and fixed. Inj.
After injection of test dose of Lignocaine with adrenaline 2%, 3ml,
Inj. Bupivacaine 0.5%, 12 ml were given. Block height was checked by
spirit swab for temperature sensation. In group GA, parturients were
induced with i.v. Thiopentone sodium 5-7 mg/ kg after 3 min
preoxygenation with 100% O2. Inj. Succinylcholine 1.5 mg/kg
i.v. was given to facilitate tracheal intubation. Trachea was intubated
with 7-7.5 mm cuffed endotracheal tube. After checking bilateral air
entry, tube was fixed.
Depth of anaesthesia was maintained with O2:N2O
50%:50%, isoflurane and muscle relaxant i.v. Atracurium 0.5 mg/kg bolus
followed by maintenance dose 0.1 mg/kg. At the end of surgery, when
parturient resumed some breathing effort, residual effects was reversed
with i.v. Neostigmine 0.05 mg/ kg and i.v. Glycopyrrolate 0.01 mg/kg.
When the patients were fully awake then the endotracheal tube was
removed with oral suction. Hypotension defined as fall in baseline SBP
>20% was corrected with intravenous crystalloid fluid, if persist
then i.v. Mephentermine 6 mg incremental dose was given. Bradycardia (HR
<60) was corrected with i.v. Atropine 0.6 mg. ECG, Heart rate,
Systolic blood pressure, Diastolic blood pressure, Mean blood pressure,
Respiratory rate, Oxygen saturation and End tidal CO2 were
recorded throughout the procedure and note at the time of induction and
at every 2 minute after induction till delivery of baby. Induction to
skin incision, skin incision to delivery and uterine incision to
delivery time were also noted. Umbilical artery blood sample was taken
from a double clamped segment of umbilical cord and umblical arterial
blood gas analysis was immediately done using COBAS 121 ABG machine.
Apgar score of neonate at 01 and 05 minutes after delivery of the
neonate were assessed. Statistical analysis was done using Graph pad
prism 7 software. Data were analyzed by One way ANOVA test and Tukey’s
multiple comparison test. Tukey’s multiple comparison tests was used for
multiple pair wise group comparison. The results were analyzed by
various statistical techniques like percentage, mean and standard
deviation. p- Value <0.05 considered significant finding.
Results
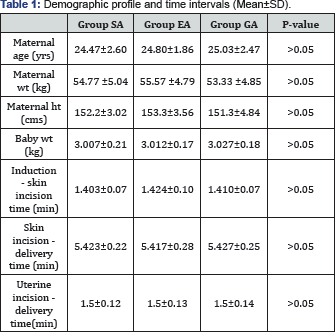
The maternal and neonatal demographic profiles,
induction to skin incision time, skin incision to delivery time and
uterine incision to delivery time were statistically comparable among
three groups (p>0.05) (Table 1).
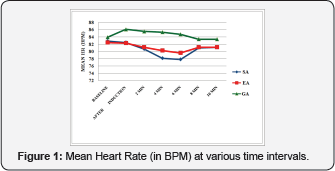
Highly significant fall in maternal HR from baseline was seen just
after induction, at 2 min, 4 min and 6 min in group SA and group EA than
group GA (p<0.001) but bradycardia was not seen in any parturients
and none of the parturient required atropine (Figure 1).
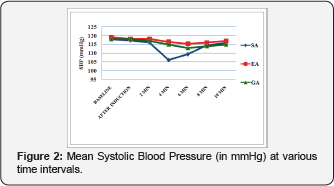
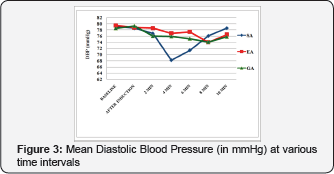
Highly significant fall in SBP and DBP from baseline was seen at 4 min
and 6 min in group SA than group EA and group GA. (p<0.0001) The
difference in mean SBP and DBP was statistically insignificant between
group EA and group GA. (p>0.05) (Figures 2&3)
3 patients in group SA had episode of hypotension that was not severe
and did not require vasopressure. None of the patient in group EA and
group GA had experienced episode of hypotension. Respiratory parameters
RR, SPO2 and ETCO2 were comparable in all three
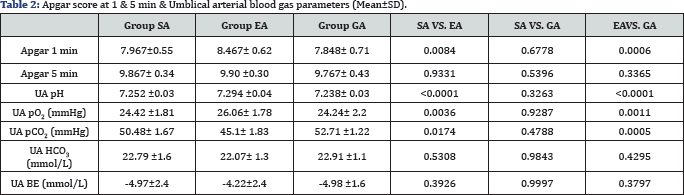
groups. Mean Apgar score of neonates at 1 minute was significantly low
in both group SA and group GA as compared to group EA. This difference
was statistically highly significant between group GA and EA but only
significant between group SA and EA. Difference in mean Apgar score at 1
min between groups SA & GA was insignificant. (p>0.05) Mean
Apgar score at 5 minute was statistically insignificant among groups.
(p>0.05) Mean UA pH and pO2 were significantly low while
mean UA pCO2 was significantly high in group SA and GA as compared to
group EA. (p<0.05) Difference in UA pH, pO2 and pCO2 values were statistically insignificant between SA & GA groups. (p>0.05) The difference in mean UA HCO3 and BE was statistically insignificant among groups (p>0.05) (Table 2).
Discussion
As with increasing incidence of LSCS in India, the
role of anaesthesiologist is also increased. Since beginning spinal
anaesthesia has been used for LSCS but it is associated with maternal
hypotension which impairs uteroplacental flow. In our study heart rate
was decreased from baseline in both spinal and epidural anaesthesia
group but bradycardia (HR <60 per min) was not seen in any
parturients. Heart rate was significantly raising in general anaesthesia
group after induction which was due to sympathetic stimulation during
laryngoscopy. Abdallah MW et al [13]
also observed tachycardia after induction in general anaesthesia group.
Incidence of hypotension was 10% (3 of 30 parturients) in spinal
anaesthesia group in our study, but none of them required vasopressure.
We observed no episode of hypotension in epidural and general
anaesthesia groups. Similar result was observed by Tonni G et al,
Mekonnen S et al and Saygi A et al [14-16]. Frequency of hypotension observed in studies of Kolatat T et al [17] (56.8% in spinal anaesthesia & 51.3 % in epidural anaesthesia) and Sener EB et al [18] (51% in epidural anaesthesia) were more as compared to our study.
This could be due to drugs used by them i.e. Kolatat T et al [17] used 1.2 ml 5% Lignocaine for spinal block and 20 ml of 2% Lignocaine with Adrenaline for epidural block and Sener E B et al [18]
used 20 ml of 0.325% Bupivacaine, were different from our study. In our
study 1 min Apgar scores were low in spinal and general anaesthesia as
compared to epidural anaesthesia, but 5 min Apgar scores were
statistically comparable among groups. Gori F et al, Rasooli S et al and
Saygi A et al [1,19,16]
also found similar results in their studies. Hypotension in spinal
anaesthesia and depressant effect of drugs used for induction of general
anaesthesia might be responsible for low 1 min Apgar score. But these
effects are short term and do not affect 5 min Apgar score. Mean UA pH
was significantly low in spinal and general anaesthesia as compared to
epidural anaesthesia but UA pH<7.15 (acidemia) was not observed in
our study. We also found no significant difference in mean UA pH between
spinal and general anaesthesia. Similar findings were observed by
Kolatat T et al, Sener EB et al, Tonni G et al, Strouch ZY et al and
Rasooli S et al [14,17-20]. In our study UA PO2 was significantly low and PCO2
was significantly high in spinal and general anaesthesia as compared to
epidural anaesthesia, while no significant difference was found in UA
HCO3 and BE values among groups and all these parameters were within normal limits.
Kolatat T et al, Petropoulos G et al, Tonni G et al, Abdallah MW et al and Rasooli S et al [17,12,13,14,19] observed similar findings regarding UA PCO2, HCO3 and BE. Kolatat T et al [17], Petropoulos G et al [12] and Tonni G et al [14] found high UA PO2 in general anaesthesia group and their results were different from our study. They explained it, that high maternal inspired O2 concentration in general anaesthesia result to high UA PO2
in neonates. Long intervals including induction to delivery time >10
minutes, skin incision to delivery time >8 minutes and uterine
incision to delivery time >3 minutes adversely affects neonatal
outcome by decreasing uteroplacental blood flow, but these intervals are
within normal limits in our study. Limitation of our study was small
sample size and also we have not done maternal arterial blood gas
analysis which might be the reason for the neonatal acid base imbalance.
Further study with large sample size including both maternal and
neonatal arterial blood gas analysis should be done to evaluate the
effects of anaesthesia techniques on neonatal outcome.
Conclusion
We concluded that spinal anaesthesia, epidural
anaesthesia and general anaesthesia are safe for both mother and
neonates as maternal blood pressure, Apgar score and umbilical arterial
blood gas values are not significantly affected. However among three
anaesthetic techniques, epidural anaesthesia was associated with better
short term neonatal outcome and could be a preferred anaesthetic choice
for elective lower segment caesarean section.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment