Comparitive Study of Bupivacaine with Nalbuphine and Bupivacaine alone for Post-Operative Analgesia in Subarachnoid Block for Lower Limb Surgeries- Prospective Randomised Study-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Background: Nalbuphine is a synthetic opioid ,
with kappa agonist or partial µ antagonist action. When added as an
adjuvant to intrathecal bupivacaine, it acts on dorsal horn of spinal
cord producing analgesia with decreased incidence of µ receptor side
effects.
Aims and Objectives: To compare the onset,
duration of sensory blockade, duration of motor blockade, 2 segment
regression and duration of post operative analgesia achieved, by
comparing hyperbaric bupivacaine alone with hyperbaric bupivacaine and
nalbuphine after intrathecal administration.
Material and Methods: Randomised double blind
study done on 60 patients, who were undergoing lower limb surgeries
under subarachnoid block. Patients were divided into two groups, group B
receiving 15mg of 0.5% hyperbaric bupivacaine+0.1ml of normal saline
and group N receiving 15mg of hyperbaric bupivacaine+0.1ml of nalbuphine
(1mg). Assessment of duration of motor and sensory blockade was done by
modified bromage scale and pin prick method respectively.
Results: There was no significant variation in
onset of motor and sensory blockade in two groups, but mean time of
post-operative analgesia in group N was highly significant than group
B(P<0.001).
Conclusion: Thus we conclude that
intrathecalnalbuphine at dosage of 1mg can be used as effective adjuvant
along with 0.5% of hyperbaric bupivacaine intrathecally to have good
post-operative analgesia.
Keywords: Nalbuphine; Modified bromage scale; Sub-arachnoid block; hyperbaric bupivacaineIntroduction
Analgesia during post operative period is of main
demand these days. A pain free and stress free postoperative definitely
helps in early mobilization and recovery. Intrathecal administration of
opioids in conjunction with local anaesthetics improves the quality of
intraoperative analgesia and provides superior quality and duration of
analgesia post-operatively [1,2].
Nalbuphine is an opioid, which is structurally
related to oxymorphone, highly lipid soluble with an agonist activity at
kappa and an antagonist activity at µ opioid receptor [3].
When nalbuphine is added as an adjuvant to
intrathecal bupivacaine, it has potential to provide good intraoperative
and post operative analgesia with decreased incidence of µ receptor
side effectslike respiratory depression [4].
The side effects of nalbuphine are like dizziness, bradycardia, nausea,
vomiting, pruritis, urinary retention and sedation. Nalbuphine has
short duration of action due to its lipid solubility and rapid clearance
when compared to morphine [5].
Here we compared the effect of nalbuphine addition to
hperbaric bupivacaine intrathecally with hyperbaric bupivacaine alone
for duration, quality of post operative analgesia and any side effects.
Aims and Objectives
To compare the
- Onset of sensory and motor blockade.?
- Duration of sensory and motor blockade.
- 2 segment regression.
- Duration of post operative analgesia achieved
- To study any side-effects with addition of nalbuphine.
- Haemodynamic parameters.
Materials and Methods
This double blind prospective randomized study was
done from may 2016 to august 2016, on patients who were admitted at
Adichunchanagiri institute of medical sciences, posted for lower limb
surgery under sub arachniod block.
The study was undertaken after obtaining ethical
committee clearance as well as informed consent from all patients. The
sample size was decided in consultation with the statistician and was
based on initial pilot study observations, indicating that approximately
23 patients should be included in each group in order to ensure a power
of 0.80. Assuming a 5% drop out rate, the final sample size was set at
30 patients in each group, which would permit a type 1 alpha error
=0.05, with a type 2 error of beta=0.2.
Study consists of 60 patients of both genders
belonging to ASA I and II aged between 18-65 years, who were undergoing
lower limb surgeries under sub arachnoid block. Patients were randomly
allocated into 2 groups of 30 patients each, group N and group B by
computerized randomization method. Group N received 3ml of 0.5%
Bupivacaine(15mg)+1mg of Nalbuphine, group B received 3ml of 0.5% of
Bupivacaine (15 mg)+0.1ml of normal saline for spinal aneasthesia. Pre
anaesthetic check up was done and patients were kept nil per oral for
about 6-8 hours. Patient was pre medicated with Tb- Alprazolam 0.5mg and
Tb- rantidine 150 mg night before surgery.
Inclusion Criteria
- American Society of Anaesthesiologists (ASA) I and II patients.
- Age group of 18-65 years.
- Patient with written valid consent.
- Patient undergoing elective lower limb surgery.
Exclusion Criteria
- Infection at the site.
- Bleeding disorder.
- Allergic reaction to any anaesthetic drug.
- Patients on tranquilizers, hypnotics, sedatives and other psychotropic drugs.
Patient was shifted to OT, intra operatively an IV
line was secured with 18 G iv cannula, standard monitors(NIBP, SpO2,
ECG) connected and vitals recorded, patients were preloaded with 10ml/kg
ringer lactate solution. Sub arachnoid block was given under strict
aseptic precautions in sitting position preferably in L3-L4 interspinous
space with 25G quinkies spinal needle. The study medication was
prepared by the person who was not involved in the study to ensure
blinding of anaesthetist. Respective agents were injected according to
the group, intra operatively haemodynamic parameters and the following
parameters were noted and used for comparison between the groups.
Time of spinal anaesthesia (drug administration time)
- Time of onset and complete sensory and motor block
- 2 segment regression of the block.
- Duration of sensory block (sensory level was assessed by pin prick method)
- Duration of post-operative analgesia(effective analgesia-time of onset of sensory block to the first request of analgesia by using VAS score).
- Duration of motor block (which was assessed by modified bromage scale)
Modified bromage scale
0-no motor block with full flexion of knees and feet
1-just able to flex knees, full flexion of feet
2-unable to flex knees, but some flexion of feet possible.
3-unable to move legs/feet
Post operatively pain, sensory level, motor level was
evaluated every 30mins for first 2 hours, every 60mins for next 6 hours
and at 12 hours and 24 hours in recovery room. Pain was assessed by VAS
(visual analogue scale). Here patient was given a scale marked from
0-10 and was asked to mark on the scale the degree of pain he /she
experiencing from 0-no pain to 10 maximum pain ,when VAS>3, rescue
analgesia given with injdiclofenac sodium.
Side effects like (pruritis, urinary retention,
respiratory depression, post operative nausea and vomiting etc) were
recorded for 24 hours.
Statistical analysis
Data analysis was done with the help of computer
using SPSS statistical package- Version 17. Using this software,
measures of central tendency, measures of dispersion, 't' value, chi
square and 'p' values was calculated. 't' test was used to test the
significance of difference between quantitative variables and Yate's and
Fisher's chi square tests for qualitative variables. A 'p' value less
than 0.05 will denote significant relationship. Demographic
characteristics of cases studied, outcome variables and the significance
of the relationship between the outcomes variables of the two groups
was analyzed using the above tests.
Results
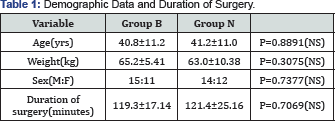
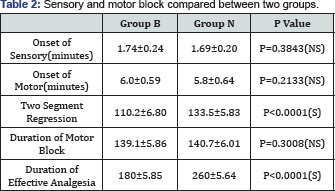
Both groups were compared on various variables like
age, weight, sex ratio and duration of surgery. There was no significant
difference found in various haemodynamic vital parameters intra
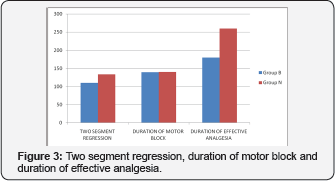
operatively between the two groups (Table 1,2) (Figure 1-3).
Summary of Results
The mean time of onset of sensory blockade and motor
blockade between the two groups is comparable with p value of (0.3843)
and (p=0.2133) which is not statistically significant. Two segment
regression of sensory blockade is significantly prolonged by addition of
intrathecalnalbuphine as seen in group N. The duration of analgesia is
significantly prolonged with addition of nalbuphine compared with
bupivacaine alone.
Discussion
Subarachnoid block is the first choice for lower
abdominal and lower extremity surgeries. Sub arachnoid block with
bupivacaine alone has short period of post operative analgesia. Many
adjuvants like fentanyl,morphine,clonidine has been used to prolong post
operative analgesia. Spinal opioids can provide profound post operative
analgesia with fewer central and systemic adverse effects than with
opioids administered systematically [6].
Most commonly used opioids are usually µ agonist drugs, which has
excellent analgesic effect with various µ related side effects.
Eventually it was found that significant analgesia can be obtained by
action on kappa binding sites also by bypassing p related side effects [7,8]. As there was less studies on opioids like Nalbuphine as an adjuvant in spinal anaesthesia. We have conducted this study
Nalbuphine hydrochloride is a kappa agonist/partial µ antagonist analgesic [8,9].
Whennalbuphine binds to µ receptor,it serves only to competitively
displace other µ agonists from the receptor without itself displacing
any agonist activity similar to those of nalaxone. It binds to kappa
receptor; it has agonist effect, so nalbuphine has mixed
agonist-antagonistic effect. These affects inhibit release of
neurotransmitter that mediates pain such as substance p and in addition
to this it also inhibits post synaptic interneuron and outer neuron of
spinothalamic tract which transports nociceptive information.
Local anesthetic bupivacaine acts mainly by blockade
of voltage gated sodium channels in the axonal membranes, and also by
further effect on presynaptic inhibition of calcium channels [10]. A combination of these affects may explain the observed synergism between bupivacaine and nalbuphine in our study.
The principle finding of this study is that addition
of 1mg of intrathecalnalbuphine to spinal anaesthesia in patients
undergoing lower limbsurgery with hyperbaric 0.5% bupivacaine
intensifies the sensory blockade and increases the duration of sensory
blockade without µ related side effects. Two segment regression, time of
sensory blockade and duration of analgesia were maximally prolonged
with nalbuphine 1mg with minimum effects over haemodynamic and
respiratory parameters [11].
Previous studies have demonstrated that visceral
analgesia is mediated by both µ and kappa receptors and that
intrathecalnalbuphine suppresses response to visceral pain [12].
In our study 2 segment regression of sensory block was prolonged with
addition of nalbuphine to bupivacaine which correlated with that of
tiwari et al whoalso found that with addition of 0.8mg of nalbuphine to
0.5% bupivacaine for subarachnoid block provides excellent analgesia
with longer duration of action compared with 1.6 and 2.4mg of nalbuphine
[13].
Large number of animal studies has been undertaken to
prove that intrathecalnalbuphine was not neurotoxic. Rawal et al showed
in sheep model usinghistopathological methods that,
intrathecalnalbuphine even at large doses 15-24mg were not associated
with histopathological changes of the spinal cord [9].
From our study we can also conclude that use of
nalbuphine in dosage of 1mg along with bupivacaine 0.5% H,does not cause
any gross haemodynamic disturbances. Similar findings are seen in study
conducted by culebras et al5,tiwari et al [13], mortafa et al [14].
In our study none of the patients had respiratory
depression since nalbuphine is µ antagonist,respiratory depression is
predominantly µ mediated. Respiratory depression effect is expected to
be attenuated by nalbuphine, so nalbuphine exhibits ceiling effect for
respiratory depression[RR<30cpm,spo2<90%] this is proved in
studies done by romagnoli and keats [15].
Our study also concludes that addition of nalbuphine
had significantly longer duration of first request of analgesia,
compared to patients who received bupivacaine alone and it also prolongs
duration of analgesia which correlates to result of studies done by lin
[16]
found that intrathecal nalbuphine at dosage of 0.8-1.6mg improved
quality of intraoperative analgesia during cesarean section with good
visceral analgesia,our study showed excellent analgesia at dosage of 1mg
as an adjuvant to intrathecal bupivacaine [5]. Adverse effects like nausea,vomiting, urinary retention and shivering were statistically insignificant.
Conclusion
On the basis ofthis study,in conclusion, addition of
nalbuphine hydrochloride in dosage of 1mg to intrathecal bupivacaine
0.5% H prolongs the duration of sensory blockprovides excellent and
longer duration of post operativeanalgesia,prolongs the 2 segment
regression with maintaining stable haemodynamics without any significant
side effects in patients undergoing lower limb orthopaedic surgeries.
Thus we conclude that intrathecalnalbuphine at dosage
of 1mg can be used as an effective adjuvant along with intrathecal
hyperbaric bupivacaine 0.5% to have a good post operative analgesia.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment