Efficacy of Needle Thoracostomy following Iatrogenic Pneumothorax in Critically Ill Patients-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
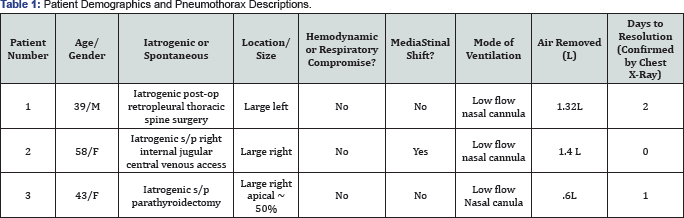
We report a series of 3 patients who experienced
iatrogenic pneumothoraces in the ICU: these were resolved with a single
needle thoracostomy and no patients experienced recurrence. The
following criteria were used to determine whether needle thoracostomy
was appropriate: all pneumothoraces were unilateral and greater than 30%
apical in location; patients did not have effusion, hemothorax,
purulence, or other drainage; coagulation and platelet parameters in
range; no history of surgeries on the hemithorax; and patient consent
was obtained prior to the procedure. A needle thoracostomy can be an
appropriate, less invasive alternative to chest tube insertion to
resolve post-operative pneumothoraces.
Keywords: Resolution of iatrogenic pneumothorax; Needle thoracostomy; Critical care medicineIntroduction
Due to increased invasive monitoring and treatment
modalities in critically ill patients, iatrogenic pneumothorax occurs
with an incidence rate of 4-15% [1], greater amongst teaching facilities [2]. Not accounting for asymptomatic or occult occurrences [3]
raises the expected overall incidence of pneumothorax. Traditional
treatment for spontaneous or iatrogenic pneumothorax is surgical
thoracostomy (chest) tube insertion. Despite being widely accepted, this
practice is not without complications and results in significant pain
as well as increased morbidity and mortality [4].
Herein we report 3 cases in which an iatrogenic pneumothorax in a
critically ill patient was resolved via a single bedside needle
thoracostomy. Each patient provided written consent to participate in
this research study and for the publication of their information as a
clinical case report.
There has recently been interest in treating
spontaneous pneumothorax with needle thoracostomy with success, however
this has not gained widespread favor amongst intensivists. Several
randomized controlled studies have demonstrated the efficacy of needle
aspiration as comparable to chest tube insertion for the treatment of
primary spontaneous pneumothorax [5-7].
Despite these reports, few literature accounts have described the
efficacy of needle aspiration for iatrogenic pneumothorax in critically
ill patients.
Case Report
This was a retrospective review of patients' medical
charts. The patients gave written informed consent for the procedure and
for release of information for educational purposes. The following
criteria were used to determine whether needle thoracostomy was the
appropriate intervention: unilateral and greater than or equal to 30%,
apical in location, and patients were not expected to have effusion,
hemothorax, purulence, or other drainage, and coagulation and platelet
parameters in adequate range, no history of surgeries on the hemithorax,
and signed informed consent for the procedure.
Procedure Description
All procedures were performed by a single
anesthesiologist at the bedside in the intensive care unit. Following
collection of informed consent for the procedure, patients were prepped
and draped in sterile fashion. Analgesia was achieved with 50-75 mcg of
IV fentanyl and local anesthesia was accomplished with Ropivacaine .5%
or lidocaine 1%. The rib inter space between the third and fourth ribs
were accessed by inserting a 16 or 18 gauge needle on the ipsilateral
side of the pneumothorax with gentle downward force until contact was
made with the third rib anteriorly, along the midclavicular line. The
angiocatheter was directed superiorly until located in the avascular
soft tissue of the inter costal space. The needle was then directed
downward an additional 2cm until air was aspirated. The catheter was
then threaded off and a thumb seal was made on the catheter hub. A
stopcock was attached immediately to prevent further air entry. A 60 cc
syringe was attached to the stopcock and air was slowly withdrawn by 60
cc aliquots (released into ambient air) and recorded (final volume in Table 1).
When resistance was felt and no further air could be withdrawn, the
catheter was withdrawn while the stopcock remained in the "off position
Immediately as the catheter was withdrawn, an
occlusive dressing (Tegaderm) was applied and reinforced until this was
seen to be airtight by the provider. Daily follow up chest x-rays were
obtained to confirm resolution of pneumothorax (Figure 1).
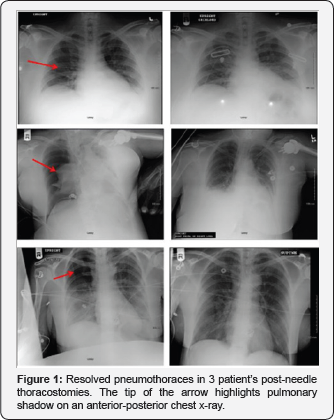
All pneumothoraces were iatrogenic in nature,
identified by plain chest x-ray and radio graphically resolved following
a single needle thoracostomy. No patients experienced recurrence,
complications, or required subsequent chest tube insertion. An average
of 1.11L of air was removed (range 0.6-1.4L). Average day to resolution
was 1 day with a range of 0-2 days. All three patients were on low flow
nasal cannula
Discussion
Chest tube insertion is currently the standard of care for mechanically ventilated patients [8].
In this case series we have demonstrated 3 patients that had iatrogenic
pneumothoraces resolved following a single needle thoracostomy. In this
small case series, we have demonstrated complete resolution of
pneumothorax without chest tube insertion. The decision not to place a
chest tube in mechanically ventilated patients is up to clinician
discretion and may have a high failure rate. Further investigations with
a larger sample size are required before conclusions can be made.
Idris and Hefny described needle thoracostomy in a 63
year old male with a >30% pneumothorax to his left hemithorax
following a fall to his chest [9].
In this case report, the patient deferred placement of a chest tube and
conservative treatment was provided. He was monitored with serial
imaging studies which revealed slight reduction in size of the
pneumothorax. He was discharged on hospital day 6 and a CT chest on 3
month follow up revealed complete resolution of the pneumothorax.
Kulvatunyou et al. described their experience with 14
French pigtail catheters for traumatic pneumothorax compared to chest
tube insertion [10].
A retrospective analysis revealed a comparable efficacy in comparison
to chest tubes. There was a greater occurrence of tube failure rate in
the pigtail catheter group compared to the chest tube group, however
statistical significance was not established.
A 2006 randomized controlled trial compared simple
aspiration vs. chest tube insertion for spontaneous pneumothorax in 137
patients [5].
Re-occurrences of pneumothorax in the aspiration group were greater,
however not statistically significant. Complications and analgesia
requirements were greater in the chest tube group, but also not
statistically significant. Overall, efficacy was comparable between the
methods. The authors concluded that needle aspiration is an alternative
method to chest tube insertion as the initial treatment for the first
episode of primary spontaneous pneumothorax.
Our experience suggests that needle thoracostomies
are an appropriate alternative to tube thoracostomy to resolve apical
uncomplicated iatrogenic pneumothoraces. We believe current guideline
for routine tube thoracostomies may need to be revised however clinical
judgment, experience and patient stability will guide treatment modality
in all cases. We continue to recommend chest tube insertion for
patients with tension pneumothorax resulting in hemodynamic instability.
This case series attempts to expand indications of needle thoracostomy
to iatrogenic etiology and patients on mechanical ventilation. A
randomized controlled study with outcomes focused on ICU stay, days to
resolution, cost and complications are required to confirm the
widespread use of this technique.
Author Roles
CS contributed to data collection, data analysis, and
manuscript writing. FD contributed to data collection, data analysis,
and manuscript revisions. PD contributed to maintaining regulatory
documentation, data analysis, and manuscript writing. DM was involved
with data analysis and manuscript revisions. EC was involved in data
collection, data analysis, regulatory documentation, and manuscript
writing
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment