Prognostic Factors of Pediatric Emergency Anesthesia at the University Hospital of Cocody-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Summary
FIn sub-Saharan Africa and singularly in Ivory Coast
the anesthesia of the children in urgen cyisa real Challenge because of
many risks to which it exposes. The lack of data at the University
Hospital of Cocody has motivated this study whose the aim was to search
the elements which can make it possible to predict the pediatric
mortality in case of anesthesia in urgency in order to anticipate their
occurred and in the worst case drawing up a protocol medical car for the
children.
Population and method: It was carried out over
one 05 years period going from July 2008 to June 2012. It concerned all
the children whose age lay between 0 and 15 years, which were taken
charges with the min urgency under anesthesia with the service with
anesthesia reanimation D "a Hospital and University D "Abidjan-Coast D"
Ivory.
Results and discussion: The factors forecast
raised in this study are: Digestive pathologies, the young age,
classification ASA, the absence of doctor anesthetist to the block,
interventions carried out the night.
Conclusion: The good practice of the pediatric
anesthesia in urgency would pass by staff training in anesthesia of the
children with blocks dedicated and equipped.
Keywords: Anesthesia; Pediatric; In urgency; Mortality; PreventionIntroduction
The basic principles of the anesthesia have always
been the same ones any where in the world. But their application would
require all the more important adaptations because of two main
constraints: the subject is young and disabilities are many [1].
This assertion is confirmed by most studies which
report that mortality and morbidity are strongly influenced by the age.
In developed countries, according to the register of perioperative
mortality, the incidence of the cardiac arrests due to the anesthesia
is: 1.4+0.45 per 10000 anesthesia, 55% concerned infant of less than one
year. The anesthesia in urgency accounted for 21% [2,3].
In Ivory Coast, a study carried out [4]
in 1996 on the intra operative cardiac arrest sand in the recovery
phase in a university hospital of reference, found an incidence of 01
per 250 anesthesia or 0.4%. Unfortunately, the children accounted for
67% of the cardiac arrests. 3103 anesthesia were recorded. Generally
practiced in emergency, the pediatric anesthesia could concern children
in precarious situation, either because of an extreme immaturity of the
major functions (high prematurity), or because of severe pathology
acquired or constitutional of ten genetically transmitted which can
engage the vital prognosis in the absence of an adequate support through
gestures of reanimations [3].
In sub-Saharan Africa and taking into account our
conditions of exercise, the practice of the anesthesia of the children
in case of urgency is a real challenge because of many risks to which it
exposes [5].
The absence of data in the highest reference hospital has motivated
this survey whose objective was to search the elements which can make it
possible to predict the pediatric mortality anesthesia in urgency in
order to anticipate their occurrence and in the worst case drawing up a
protocol of specific medical care for children.
Equipment and Method
It was about are prospective, descriptive and
analytical study conducted in the department of anesthesia and intensive
care of the largest hospital of reference in Ivory Coast over one 05
years period. All the children whose age was between 0 and 15 years and
who had a surgical operation in emergency were included. An index card
collection was the essential material support of our study. This card
included the following elements: Epidemiologic parameters, The
pre-anesthetic evaluation, anesthetic histories, classification ASA, the
anesthetic data (the type of anesthesia, the type of premedication, the
type of induction, the control of the air routes), the kind of
pathologies supported; the quality of the expert having realized
anesthetic induction, Anesthetic accidents and incidents.
Anesthetic accidentss
Any major complication occurring during surgery with consequences on the condition of the patient.
Incidents
Any minor complication occurring during surgery and
which is without consequence on the clinical state of the patient and
the post-anesthetic evolution of the children.
All these data have been recorded and processed with
the Software EPI Info version 6.04. The qualitative variables are
expressed in the forms of proportions and the quantitative variables are
expressed on average with their standard deviation. The graphs were
carried out starting from the software Microsoft Office Excel 2007. The
statistical test used for the comparison of the qualitative variables
was Khi2. The test was significant if p<0.05. The results will be
expressed in tables.
Results
General characteristics (Figure 1)

Neonatal anesthesia account for 5% of the work
force.The most represented age group is [07-12 years]. The mean age was
08.66±5.41 with a range of 0-15 years. 100% of the children were seen in
consultation. The predominant ASA (American society of anesthesiology) I
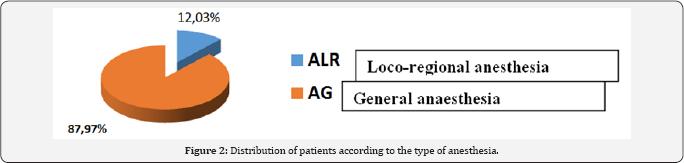
and II class with 78% of the work force (Figure 2).
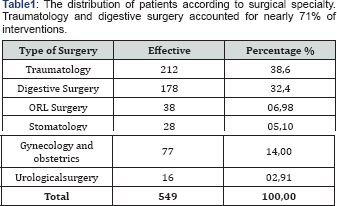
General anesthesia was the most practiced in 87.97%
of cases. 71.22% of inductions were performed intravenously. Intubation
of the trachea was performed in 73.09% of patients. 71.22% of children
had intravenous induction 63.75% of inductions performed in the absence
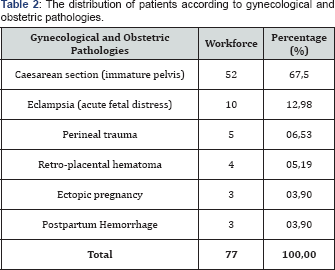
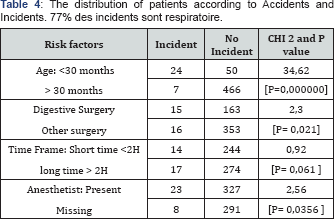
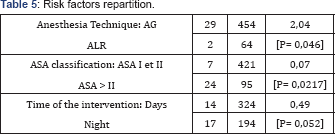
of a resuscitation anesthesiologist (Table 1-5).

Comments
The low number of neonatal anesthesia is explained by
the high number of deaths before transfer to a specialized structure.
These structures were insufficient number with a non-existent evacuation
system. This management of fewer frequent surgical children decreases
the experience of the personnel of these specialized structures with
equipment increasingly defective. The majority of Anesthesia
Consultations were performed by anesthetists in 90% of cases. General
anesthesia was performed in 88% of children. 71.22% of the inductions
were performed intravenously. During induction, propofol was the most
used with 41.6%. For muscle relaxation, vecuronium (Norcuron®) was the
most used curare in the operating room in 99.4%. Fentanyl is frequently
used as an analgesic in the operating room in about 91%. 63.75% of
inductions were performed in the absence of a resuscitation
anesthesiologist. Post-surgical care was provided by Surgeons in 80%
because our intensive care units are adults with one or two places for
children. As regards loco-regional anesthesia used in 12% of children,
it was essentially spinal anesthesia in 95% mainly in obstetrics and 4%
caudal and around 1% peripheral block. 20% of patients had complications
after surgery. These complications were mainly respiratory (77%) with
the incidence of cardiac arrest which was 128 per 10000 anesthesia. Most
studies made on the incidents and accidents in pediatric anesthesia in
sub-Saharan Africa had similar or higher results.
So in Benin, Zoumenou et al. [6]
general anesthesia was used in 94% of children. Regional anesthesia was
used in 1.7% of children at CNHU and 17% of children at Hôpital de la
Mèreet de l'Enfant Lagune. Inhalational induction was the commonest
technique used. Halothane was the only inhalational agent available for
induction. Seventy-two percent of children having general anesthesia
were intubated. Muscle relaxation was used in 48% of cases, only with
pancuronium. The available perioperative monitoring equipment was not
used regularly. All children having general anesthesia breathed
spontaneously with manual assistance. There were eight cardiac arrests
recorded, giving an incidence of 156 cardiac arrests per 10,000
anesthetics. Hypoxia was the commonest cause of cardiac arrest. The
mortality associated with cardiac arrest was very high (62%). There were
three prognostic factors that predicted a poor outcome: age <1 year,
emergency surgery and an ASA score of three or more.
In congo, Otiobanda et al. [7]
brought back a cardiac arrest perioperative for a sample of 180
children operated to the university hospital of Brazzaville (either 55
out of 10,000 anaesthesia) and a perioperative mortality estimated at
270 out of 10,000 anesthesia's. In burkina faso, Kaboré et al. [8]
reported a perioperative mortality rate of 624 out of 10,000
anesthesias in the service at the pediatric university hospital of
Ouagadougou. In gabon, Essol Aandal et al. [9] brought back a lower morbidity, estimated at 11 out of 10,000 anesthesias.
Methodologies of the sevarious studies are not always
comparable; in the same way, the partial or total responsibility of the
anesthesia was not explicitly studied there. Our values were higher
than that reported from Maghreb which was from 2.23 out of 10,000
anesthesias [10].
In the POCA Registry of 1994, 63 institutions
enrolled and submitted 289 cases of cardiac arrest. Of these, 150
arrests were judged to be related to anesthesia. Cardiac arrest related
to anesthesia had an incidence of 1.4 ± 0.45 (mean ± SD) per 10,000
instances of anesthesia and a mortality rate of 26%. Medication-related
(37%) and cardiovascular (32%) causes of cardiac arrest were most
common, together accounting for 69% of all arrests. Cardiovascular
depression from halothane, alone or in combination with other drugs, was
responsible for two thirds of all medication-related arrests.
Thirty-three percent of the patients were American Society of
Anesthesiologists physical status 1-2; in this group, 64% of arrests
were medication-related, compared with 23% in American Society of
Anesthesiologists physical status 3-5 patients (P<0.01). Infants
younger than 1 year of age accounted for 55% of all anesthesia-related
arrests. Multivariate analysis demonstrated two predictors of mortality:
American Society of Anesthesiologists physical status 3-5 (odds ratio,
12.99; 95% confidence interval, 2.9-57.7), and emergency status (odds
ratio, 3.88; 95% confidence interval, 1.6-9.6).
Digestive pathologies were found to be a prognostic
factor. The reasons given in our exercise conditions were: immature
organs, high sensitivity of children to hypovolemia, difficulties with
parenteral nutrition, anesthetic risks with halothane, and per-and
post-operative hypothermia [6].
Western studies found that 61.1% of anesthetized children for visceral
surgery were treated with CHG or CHU. They recommend an organization of
the management of pediatric anesthesia with protocols, reference
hospitals, specialized anesthesia of the remedies. In sub-Saharan
Africa, early diagnosis and pre-anesthesia assessment, accessible and
easy-to-use child-specific materials and medications [6].
All the publications which described the practice of
the pediatric anesthesia bring back a morbidity and excessively high and
unacceptable perioperative mortality in comparison with reference
levels in the developed countries [11].
We however realized in all these studies to show that the risk was all
the more high as the child is young, new-born child and the infants have
more raised rates of mortality [2,3].
These incidents with the disastrous consequences could complicate the
fate of sub- Saharan Africa which bases its hope son youth [4].
The doctor's anesthetist absence in the operating room was also found
like one of the independent factors forecasts in this study. In Africa
and every where in the world as shows in most studies, the absent or an
in experienced anesthetist was revealed like factor major forecast [1,3,11-13].
For these authors, When we take care of children, it
are necessary to satisfy certain specific conditions as a preliminary,
corresponding to the age group concerned, as well as regards staff as of
structures. In general-purpose hospitals it would be necessary to have a
space dedicated to the child and encourages the creation of pediatric
references hospital. Each work place where anesthetists will take care
of children should be equipped with pediatric equipment [4,2,14]
in spite of we did not find a direct link statistical, this study
pointed out a more significant number of deaths under general anesthesia
compared to loco regional anesthesia, in the surgeries practiced in the
night on children who were ASA class III and IV and which was operated
after a long period of waiting.
The significant number of incident during the general
anesthesia could explained by the fact that it was the technique more
practiced in pediatry during this time. About 80% of the ventilation
support incidents in this study could probably be related to the general
anesthesia. A significant number of authors face respiratory
complications in pediatric anesthesia. According to them, the problems
of air routes would be the most frequent cause of pediatric anesthesia
complications [11,15].
Thus, they recommended the use of probe of intubation with good-sized balloon with monitoring of the pressure [16,17]. Keenan RL [18]
in his studies on the factors forecasts of the brady cardiain pediatric
anesthesia had found: classification ASA, urgency, the time of
interventions higher than 4 hours and thein experienced supervisory
anesthetist [18]. But according to Draper and collar [19,20], the risks related to the loco regional anesthesia are not negligible when it is combined with the general anesthesia.
Conclusion
The children are not adults in miniature. The
incidents in pediatric anesthesia differ to a significant degree
compared to the incidents concerning the adults. These risks are all the
more high as the child is young and the surgery is urgent. The good
practice of the pediatric anesthesia in urgency would pass by a staff
training in anesthesia of the children with blocks dedicated and
equipped, by an initial training and the maintenance of knowledge of
staff. A great hope is also place don't he use of the new agents and
technical anesthetic.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment