Supraorbital/Supratrochlear Nerve blocks: Clinical Significance of the Superior and Anterior Approaches-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Introduction
Hair restoration is one of the commonest cosmetic surgery procedure in men [1].
The procedure is performed under local anaesthesia. Many of the
patients are anxious about the degree of pain to be expected during and
after the surgery. The pain of the local anaesthetic agent is dependent
on various factors like needle gauge, composition, temperature, pH,
speed of injection, anatomical structure/area etc. Various maneuvers are
used to decrease the pain during the administration of local
anaesthesia like vibration anaesthesia Cryotherapy etc [2-4]. With the introduction of newer drugs for local anaesthesia, the safety is increased.
Peripheral nerve blocks constitute a major tool in
the armamentarium in the office-based cosmetic surgery procedures.
Supraorbital (SO) and supratrochlear (ST) nerve are the terminal
branches of the frontal nerve [5].
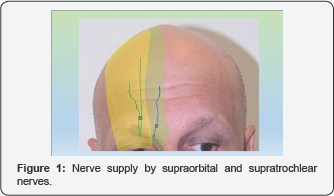
These nerves supply mainly the skin of the forehead. These nerve blocks
are beneficial in many procedures. The SO/ST nerve block during hair
transplant surgery decreases the severity of the pain for recipient site
injections. Their blockage is beneficial in treating disorders like
trigeminal neuralgia, migraine etc [6,7]. These nerve blocks also result in significant decrease in the need of additional analgesics and opioids [8]. The SO/ST nerves collectively provide sensory innervation to the forehead and frontal scalp as well as to the vertex (Figure 1). The anatomical details and variations of these nerves is very essential for a proper anaesthesia.
The supraorbital (SO) nerve emerges from the
supraorbital foramen or notch. The foramen or notch is located about 27
mm lateral to the glabellar midline. However, the distance varies if
different races [9,10].
The nerve divides into medial and lateral branches. Similarly
supratrochlear (ST) nerve emerges through supraorbital notch about 17mm
from glabellar midline. It follows one of the four courses i.e., Ia (ST
nerve emerges independently from SO nerve as a single nerve through
Corrugator Supercilli muscle), Ib (ST emerges independently from SO
nerve and bifurcates into 2 branches prior to entering the Corrugator
Supercilli muscle), IIa (ST nerve emerges from SO notch with SO nerve
and passes through Corrugator Supercillimuscle as a single nerve), and
IIb (ST emerges from SO notch with SO nerve and bifurcates into 2
branches prior to entering the Corrugator Supercillimuscle) [11].
There are two techniques to accomplish SO/ST nerve
block, i.e., anterior and superior. In superior approach, the needle is
inserted from the cephalic side in such a way that the tip of the needle
is felt at SO foramen by the palpating finger of the physician's other
hand. Whereas in the anterior approach, the physician stands on the side
of the patient and the needle is directed towards the midline. The
following study was undertaken to compare the pain levels of anterior
and superior approaches.
Materials and Methods
The study was conducted in 30 patients undergoing SO/ST nerve clock for hair restoration surgery. The patients undergoing 1st
session were included. The informed consent was taken. All the
injections were administered by the surgeon. A 3ml syringe with 30 oG
needle was used containing 1% Xylocaine with adrenaline is 1;100,000
dilution. Separate needle was used for each side.
Superior Approach
The needle was introduced about 2cm above the SO
foramen palpated. About 0.5ml of the anaesthetic solution was injected.
The needle was advanced caudally till the tip was felt at the foramen
and 0.5ml was injected here. The needle was withdrawn slightly and
directed laterally injecting about 1.0ml in a 'fanning out' way. The
needle was again withdrawn and directed medially injecting about 1.0ml.
This technique encompassed all the possible branches of the SO/ST nerves
(Figure 2).

Anterior Approach
The SO foramen was palpated and the needle was
inserted from the front side of the patient. Care was taken not to
puncture the SO nerve. About 1.0ml was injected here. The needle was
withdrawn and 1.0ml was injected on medical and 1.0ml on lateral side (Figure 3). At the end of the procedure, the patients were asked to rate the pain according to the Wong Baker Faces Pain Scale [12] (Figure 4).
The patients were also asked to give their feedback on the choice of
technique for the next time. The data was analyzed statistically by
Mann-Whitney's U-test (using the Easy Statistics Calculator©, version
1.2.0, Saitama, Japan, copyright 2016).


Results
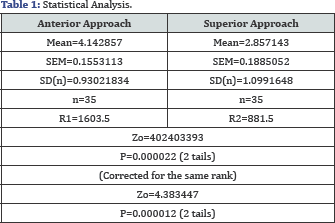
A total of 35 patients were included in the study.
The mean age was 33.4 years (range; 18 to 56). The mean pain score was
4.14 in anterior approach whereas 2.85 in superior approach (Table 1).
About 31.4% of the patients were smokers. The pain score in smokers vs
non-smokers was 4.09 vs 2.82 in anterior approach respectively. Where as
in superior approach, the mean score was 4.27 vs 2.86 in smokers and
non-smokers respectively. About 20% patients were anxious about the
anterior approach that the needle may hit the eyeball. About 71.4% of
the patients voted for superior approach on both sides for the next
time.
Discussion
The role of SO/ST nerve block is well established in
plastic surgery. It is routinely performed for the management of
different kinds of headaches like tension headache, chronic headaches,
migraine etc [6,7]. It is also the mainstay of regional anaesthesia in office-based cosmetic surgery procedures like hair restoration procedure [13].
To carry out a successful SO/ ST nerve block, the relevant anatomy is
of utmost importance which helps to locate the nerves and block them.
The sensory innervation of the face is supplied by
trigeminal nerve which has five branches4. The frontal nerve enters the
orbit via superior orbital fissure and passes anteriorly beneath the
periosteum of roof of the orbit. The frontal nerve gives off a larger
lateral branch, the supraorbital nerve, and a smaller medial,
supratrochlear nerve. The SO nerve exits the SO foramen or notch along
the superior rim of orbit, accompanied by the artery and vein. In the
notch or foramen, SO nerve gives off branches which supply mucosal
membrane of frontal sinus and filaments which supply upper eyelid. Above
the rim, SO nerve divides into superficial and deep branches.
The medical (superficial) branch passes over the
frontalis muscle and divides into multiple smaller branches with
cephalic distribution towards the hairline. It provides sensory
innervation to the forehead skin and anterior scalp as far as the
vertex. The deep branch (laterla0 runs deep in the frontalis across
lateral forehead between galeaapo neuroticanad pericranium. It provides
sensory innervation to underlying periosteum and frontal parietal scalp.
The ST nerve is the branch of the frontal nerve and supplies sensory
innervation to the bridge of the nose, medical part of upper eyelid and
medial forehead. Usually ST nerve is located about 17mm from midline and
SO nerve at 27 mm from midline.
The two approaches for SO/ST nerve block are well-
established. The current study is first of its kind to compare the
differences in terms of pain and patients' anxiety. The superior
approach was found to be clinically/statistically significant
(p<0.5). There are many factors which influence the experience of
pain perceived by patient but the technique of SO/ST nerve block
remained one of the significant factors. The visualization of watching
the injection near the eyeball probably resulted in high level of
anxiety in anterior approach.
The study by Chang et al described the pain of SO/ST
nerve block to be between 1 and 2 (out of 10) whereas in the present
study, the average pain score was 4.4 (out of 10) [14].
In another study, the average pain score was 3.9 (out of 10) and 6.8 9
out of 10) in SO/ST nerve block with and without the use of topical
anaesthetic cream [15]. In another study, the mean score also remained 3.86 [16].
In these two studies, the anterior approach was used for administering
SO/ST nerve block. In the present study, the pain score was found to be
doubled in anterior approach as compared to the superior approach. The
pain of superior approach remained 2.85.
Distraction during the administration of local anaesthesia injection plays a very important role [4,17].
In the present study, all the injections were administered by the
surgeon. The needle gauge, room temperature and environment were kept
the same in all the patients. The speed of the injection was kept slow
and maintained by the surgeon to a very slow in all the patients. The
Wong Baker Faces pain scale was used for rating as the scale gives the
opportunity to the patients to express how they feel as it has a well
established reliability and validity even in children [18,19].
Conclusion
The superior approach for administration of
supraorbital/ supratrochlear nerve block proved to be better approach as
far as the patient's anxiety about the injections is concerned. It also
proved to be less painful.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment