Pulmonary Hypertension in Children with Esophageal Varices: Frequency and Relation to N-Terminal Pro B-Type Naturetic Peptide-Juniper Publishers
Juniper Publishers-Journal of Pediatrics
Abstract
Classical homocystinuria (CHU) due to Cystathionine
Beta-Synthase (CBS) deficiency is rare autosomal recessive inborn error
of amino acids metabolism causing accumulation of methionine and
homocysteine. The clinical manifestations of CHU may include
neurological deficits mostly due to thromboembolic event so the most
common brain radiological findings are secondary to stroke. The
management is based on pharmacological treatment and dietary restriction
of methionine. We present four patients with pyridoxine non-responsive
CHU, who were found to have white matter changes on brain MRI, with a
review of their clinical characteristics and neurological outcome. All
patients had an underlying homozygous mutation of c.1006C>T (p.R336C)
in the CBS gene, hypermethioninemia due to poor adherence to diet
restriction, and were diagnosed before the implementation of the
National Metabolic Newborn Screening Program in Qatar. Dramatic
reductions in methionine levels because of better compliance were
associated with reversibility of the brain white matter lesions in two
patients.
Introduction
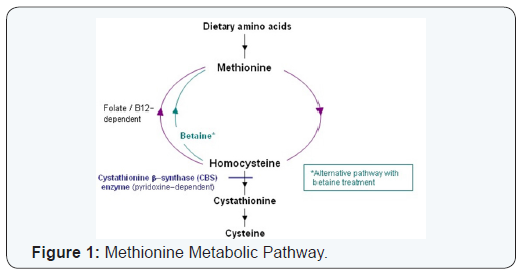
Classical homocystinuria (CHU) due to Cystathionine
Beta-Synthase (CBS) deficiency (OMIM 236200) is a rare autosomal
recessive in born error of amino acids metabolism [1]. Degradation of
dietary methionine produces an intermediate compound known as homo
cytosine that is mostly re-methylated to methionine. Homocysteine is
also converted to cystathionine by the action of CBS which requires
pyridoxine (Vitamin B6). Cystathionine Beta-Synthase
deficiency due to CBS gene mutation leads to accumulation of both
methionine and homocysteine, (Figure 1) [2]. The estimated prevalence of
Classical homocystinuria is between 1/20,000 and 344,000. However, in
Qatar it is approximately 1/1,800 births, the highest in the world
[3-5]. Untreated patients may present with multisystem manifestations,
such as vision problems due to myopia and ectopia lentis, osteoporosis,
skeletal deformities mimicking Marfan syndrome, intellectual disability,
and thromboembolic events. Neurological presentations may include
seizures, extra pyramidal signs, psychiatric disturbance and focal
neurological deficit due to infarction [5-7].
Neuro-imaging is not routinely done for patients with
classical homocystinuria unless clinically indicated. The most common
brain radiological findings are secondary to stroke: infarction,
atrophy, and venous occlusion [7]. Classical homocystinuria is
classified into pyridoxine responsive and none responsive types,
homozygous mutation of c.1006C>T (p.R336C) in the CBS gene was
attributed for most of pyridoxine non-responsive homocystinuria among
Qatari patients [4].
Protein (Methionine) restricted diet and pharmacological treatment with pyridoxine (Vitamin B6), Betaine, hydroxy-cobalamine (Vitamin B12),
and folic acid, are the corner stone in managing patients with
classical homocystinuria. The aim is to control biochemical
abnormalities and prevent complications.
Newborn screening is essential to improve clinical outcomes
and patient’s quality of life by allowing early diagnosis and
management. Poor compliance to diet restriction and medical
treatment leads to hypermethioninemia and serious complications
[8,9].
Case Series
Case 1
An 18 year old, male was diagnosed with classical
homocystinuria by the age of 7 years. He was born at term after
uncomplicated pregnancy and a smooth antenatal history. He was
hospitalized at age of 5 months for acute bronchiolitis and at 10
months with intussusceptions that was reduced by barium enema.
At 7 years of age, he presented with history of limited
vision and poor school performance. Physical examination
showed, tall stature, slender body constitution with height
falling at the 90th percentile and weight falling just below 50th
centile, long face, long tibial bones, but no scoliosis or kyphosis.
Ophthalmological assessment revealed bilateral lens subluxation
so homocystinuria was suspected and later on confirmed after
serum amino acids tests: homocysteine blood level 153.8umol/L,
(normal 4-12mol/L) and methionine serum level 495umol/L
(normal 43-223umol/L). The patient was started on treatment
immediately: Betaine (Tri-methyl glycine) 5 gm/day orally, Folic
acid 5mg/day orally, vitamin B6 (pyridoxine) 300 mg/day orally,
Vitamin B12 (Hydroxy-cobalamine) 1000ug/week IM injection and
restricted protein diet, but he had poor compliance mainly to diet.
Later the diagnosis of CHU pyridoxine non-responsive type was
confirmed by genetic study that confirmed homozygous mutation
of c.1006C>T (p.R336C) in CBS gene.
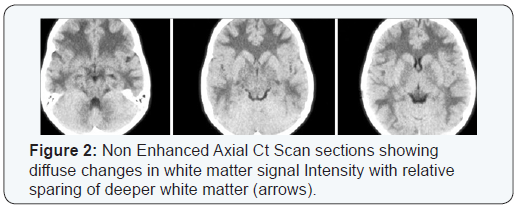
At the age of 9, he was found to have increased muscle tone
with exaggerated deep tendon reflexes in both lower limbs. A brain
CT scan showed diffuse reduced attenuation of the white matter
noted all over the brain parenchyma including the cerebellar
white matter sparing of the overlying cortex and basal ganglia
(Figure 2). A brain MRI was requested to confirm the findings but
patient traveled abroad for bilateral lens implantation. The patient
was evaluated again at the age of 13 years. At that time he was
a full time student, with learning problems, speech and language
difficulties.
He was able to walk, run, and go up & down stairs
independently, and was independent in activities of daily living.
IQ test revealed the following: verbal reasoning 37 (Average),
visual abstract reasoning 36 (average), quantitative reasoning 31 (average), short term memory 25 (average) and overall IQ
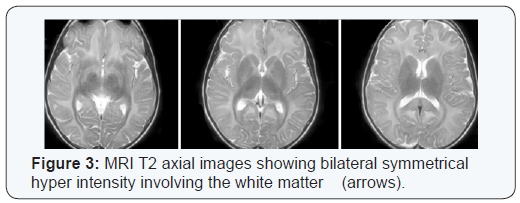
59 (mental retardation-mild). Brain MRI at that period showed
diffuse increased signal intensity on T2 and FLAIR of the cerebral
per ventricular white matter bilaterally in a symmetrical pattern,
there was also increased signal intensity of the cerebral white
matter bilaterally on diffusion weighted images. No evidence of
intracranial hemorrhage identified. The ventricles and extra axial
CSF spaces appeared unremarkable. There was a focal area of
cystic changes noted in the right cerebral per ventricular white
matter keeping with an old insult (Figure 3).The MRA of the
cerebral vessels showed no radiological evidence of vasculitis. The
tortuosity of the optic nerves noted bilaterally.
Case 2
A 17 year old girl was diagnosed with classical homocystinuria
at the age of 6 years. The diagnosis was suspected for the first
time due to incidental finding of bilateral lens dislocation.
Homocysteine level at diagnosis was 173.1umol/L and methionine
level was 622umol/L. Later CHU pyridoxine non-responsive type
was confirmed by isolation of c.1006C>T (p.R336C) CBS gene
mutation. Family history reported no parental consanguinity.
The patient had normal neonatal, infantile, and early childhood
stages. On examination (age 6 years), she had arachenodactyly,
limited cognitive function, speech was normal, and no abnormal
neurological findings were detected .I.Q test was refused by parents.
Soon after the diagnosis, she was started on medication: Betaine,
Vitamin B6 (pyridoxine), folate, vitamin B12sub> (hydroxycobalamin) IM
injections, and restricted diet but the patient was not compliant.
Hearing assessment was reported as normal and she was followed
up by ophthalmology for abnormal vision.
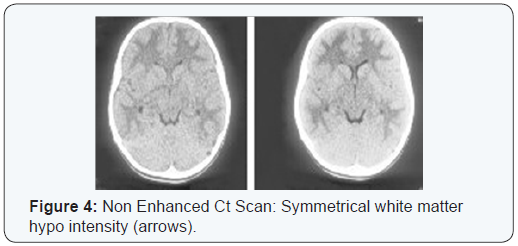
At the age of 7 years, the patient was admitted to the pediatric
ward with one month history of intermittent, generalized,
compressing type headache that was not associated with
vomiting or nausea. A brain CT reported as exaggerated white
matter hypo density of the supra tutorial brain symmetrically involved both hemispheres with no focal areas of infarction or
hemorrhage (Figure 4). A Brain MRI done in the same period also
revealed bilateral symmetrical diffuse white matter abnormality
characterized by poor myelination. Electromyography and Nerve
Conduction Study were normal. Echocardiogram was requested
showed mild mitral valve prolapse with no hemodynamic
consequences. Patient was discharged on oral aspirin with follow
up in neurology and metabolic clinics.
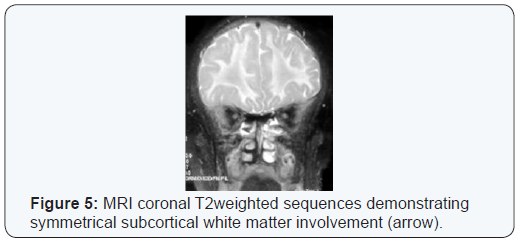
Two years later a follow up evaluation in the neurology
clinic, the patient continued to complain of infrequent bouts of
headaches that were relieved by Aspirin. Neurological exam was
normal at that time. So a follow up MRI head was requested, it
showed stationary course with no newly developed lesion (Figure
5). Echocardiogram showed mild mitral valve prolapse with mild
mitral regurgitation.
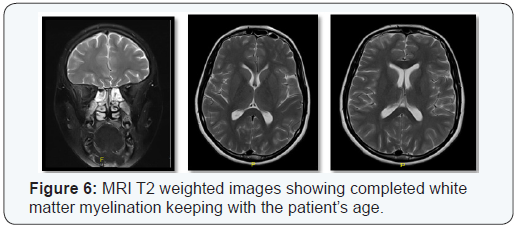
In 2008, sleep and a wake EEG was normal. A repeated MRI
head in 2009 was reported as no new changes from previous study.
Latest MRI brain done at age of 15 years showed no significant
white matter abnormality visualized, no evidence of significant
brain atrophy and with resolution of the previously reported
white matter changes (Figure 6).
Case 3
A 15 years old girl was diagnosed at age of 3 years and 10
months as a case of classical homocystinuria due to Cystathionine
Beta-synthase deficiency in early childhood, based on blood and
genetic work up. Later the diagnosis of CHU pyridoxine nonresponsive
type was confirmed by genetic test that identified
c.1006C>T (p.R336C) CBS gene mutation. Family history revel no
parental consanguinity. She was started on medication (Betaine
powder 4gm Po twice daily, folic acid 5mg Po twice daily, vitamin
B6 100mg Po twice daily, vitamin B12 injection 1mg IV once every 2
weeks, Aspirin 100mg Po once daily) and diet restriction, but had
poor compliance. EEG was done routinely and showed abnormal
bioccipital foci of spikes without clinically evident seizures.
Further EEG studies at age 6 and 8 years showed no changes.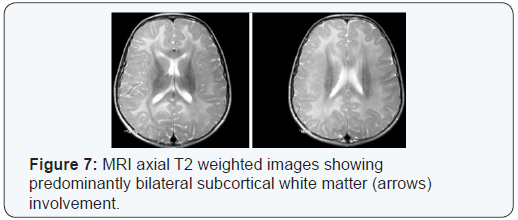
MRI brain at the age of 5 years and reported as normal. At
age of 8 years, a follow up brain MRI was reported abnormal and
showed diffuse white matter abnormality with predominant per
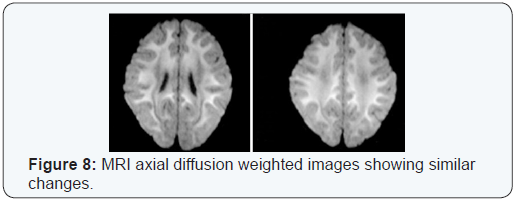
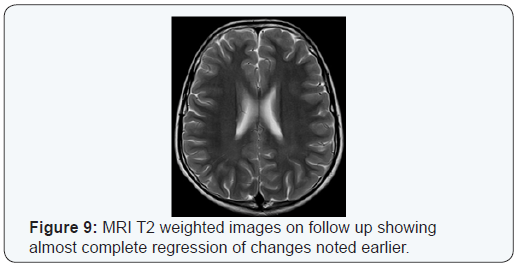
ventricular distribution (Figure 7). One year later, a repeated
brain MRI showed bilateral symmetrical white matter hyperintense
signals in T2 sequences mainly involving the subcortical
white matter and Centrum semi vale region (Figure 8). A follow
up brain MRI at 13 years of age revealed subtle high T2 signal
noted bilaterally in the frontal and parietal white matter there
were no gross white matter changes seen, there was no evidence
of cerebral or cerebellar atrophy (Figure 9).
The patient also had regular follow up with ophthalmologist
for myopia and was prescribed glasses. She was followed up by
orthopedics for thoracolumbar scoliosis. Hearing assessment was
normal. Cognitive assessment (I.Q) test score was 82, which is in
the low average level.
At the age of 14 years, the patient had a visit to Accident and
Emergency complaining of recurrent morning headache; however,
her neurological examination was reported normal as well as the
rest of her systemic evaluation.
Case 3
A 32 year old male, diagnosed with classical
homocystinuria
at the age of 10 years. He was born by vaginal delivery after uneventful
pregnancy with a birth weight of 3.5 Kg. The patient had history of
failure to thrive, and developmental delay mainly
in speech and language skills. At 4 years of age his weight was
below the 5th percentile for age and sex. There was also a history
of bilateral inguinal hernias that were surgically corrected.
At the age of 6 years he presented with severe left eye pain,
vomiting, and poor vision. Examination of the left eye showed
dislocated lens in the anterior chamber, small pupils, high
intraocular pressure >40 mmHg as well as dislocated lens of the
right eye. Based on clinical findings of long face, high arched plate
pectus carinatum and skin abnormalities he was diagnosed as:
Marfa syndrome with recurrent attacks of bilateral dislocation of
the lenses of both eyes and severe secondary left eye glaucoma
leading to vomiting.
At the age of 10 years the patient traveled to USA for further
ophthalmological assessment and management, where the
diagnosis of classical homocystinuria was made based on a
positive Cyanide Nitroprusside Test and serum amino acids
test. Initially he was started on low protein diet and pyridoxine
supplement. As he had pyridoxine non-responsive CHU, folic acid,
Vitamin B12 injections, and Betaine were added, but he had poor
compliance. In 2003, at the age of 20 years, c. 1006C>T (p.R336C)
CBS gene mutation was identified.
The patient attended schools for children with special needs
and he required educational support. When he was 16 years old, he
underwent bilateral lens implantation, surgical correction of large
left testicular hydrocele. He was also suffering from joint stiffness
and kyphoscoliosis. The patient did not have previous MRI images
as part of his diagnostic evaluation, however, at the age of 22
years, he was involved in a road traffic accident where he was a
pedestrian. The collision resulted in head injury, chest trauma,
right femoral shaft fracture complicated by fat embolism which
required open reduction and internal fixation with three weeks
of mechanical ventilation. During his hospitalization head MRI
showed scattered white matter disease in a linear fashion along
the distribution between the anterior and the middle cerebral
arteries and scattered foci in the basal ganglia, the frontal white
matter and few peripheral areas in the gray-white matter junction.
The appearance is not specific. The history and the conspicuity of
lesions on the diffusion-weighted images raised the possibility of
fat embolism; the differential diagnosis includes ischemic white
matter changes secondary to either homocystinuria or even as a
complication of hypoxic injury.
The patient was discharged ambulating in good general
condition, and Aspirin was added to his medications. He had a
cardiology team follow up for trivial mitral regurgitation and mild
aortic insufficiency. Laparoscopic cholecystectomy for gallstones
and acute cholecystitis was done at 25 years old.
Discussion
In this report, cerebral white matter changes were detected by
brain MRI in all the four patients with pyridoxine non-responsive classical homocystinuria whom had poor compliance to treatment
and diet restriction. In case
- The brain MRI was requested after he showed signs of upper motor neuron lesion.
- In case had MRI due to frequent bouts of headaches.
- MRI brain was requested as a follow up for abnormal EEG findings.
- It was done to investigate the complications of a road traffic accident. The follow up MRIs images for case (2) and (3) showed resolution of the white matter changes.
Although brain white matter lesions unrelated to
thromboembolic events are not classical manifestations of CHU,
there is increasing evidence supporting that the presence of
cerebral white matter changes might actually be part of the natural
history of this rare disease. A 10 years Iranian experience of 20
patients with homocystinuria, neuro-imaging data showed that
13 (65%) patients had white matter involvement [10]. In 2002
Yaghmai et al. [11] reported massive cerebral edema without
evidence of thrombosis occurred in a patient with pyridoxine
non-responsive classical homocystinuria who was on Betaine
treatment, the patient had poor compliance to diet restriction and
very high methionine levels reached 3000umol/L [11]. Another
study in 2004 described white matter edema after 4-6 weeks of
Betaine treatment in a child with cystathionine beta-syntheses
deficiency [12]. Reversible white matter changes were also
reported by Vatanavicharn and Brenton et al. [7,13]. Regular MRI
follow up in a 21 years old male with pyridoxine-nonresponsive
CBS deficiency was used to document reversible cerebral white
matter lesions in correlation to methionine levels [14].
The underlying cause of cerebral white matter changes in
patients with classical homocystinuria is still not well understood
whether it is a complication of the condition or as a side effect
of the medications. Even though Betaine therapy was claimed to
be the culprit by some authors [11,12,15], white matter changes
were reported in a 4 year old boy just prior to the diagnosis of
classical homocystinuria and starting treatment. His MRI changes
were normalized a year after starting treatment including Betain
[13]. In addition hypermethioninemia with levels as high as
1000umol/L or higher was a consistent finding in all reported
cerebral white matter changes in patients with CHU [7,11-14]
regardless of Betaine use. As Betaine acts on conversion of
homocysteine to methionine through an alternative pathway
(Figure 1), it will worsen the hyper methioninemia especially
in poorly compliant patients to methionine dietary restriction.
Another controversy is whether the underlying pathophysiology
of the white matter changes is due to demyelination process [7] or
intramyelinic edema [14,15].
Leukodystrophies have been documented in different
amino
acids disorders and those are due to many different mutations. An
in-depth analysis of the mutations involved in previous and future case
studies of white matter changes related to homocystinuria
could shed light on another way where neurological deficits in
CHU patients can be predicted and perhaps prevented. Linking
different CBS gene mutations and the degree of pyridoxine
responsiveness to the severity and the prevalence of cerebral
white matter changes can be worthwhile.
Summary
In summary, our report confirms the finding of cerebral
white matter changes in poorly controlled patients with classical
homocystinuria that is most likely due to hypermethioninemia.
Additionally we speculated that such complication is more likely
to occur in patients with the Pyridoxine non-responsive type,
supported by previously reported cases [7,11,12,14]. Unlike
other leukodystrophies white matter changes in most classical
homocystinuria cases are reversible, so early detection is essential
as it may prevent serious complications such as brain edema.
Conclusion
Our report supports the hypothesis of hypermethioninemia
rather than Betaine treatment as the cause of the white matter
changes. Hypermethioninemia was documented in all our
patients with levels ranging between 600->1000umol/L. The
high methionine levels are most likely due poor compliance with
treatment, especially the diet. We observed in two of our patients
that when blood methionine levels dropped because of better
compliance, previously seen brain white matter changes were
reversible.
Our study opens the door for further research for better
understanding of the natural disease progression and the longterm
sequel (e.g. cognitive and learning abilities) of white matter
involvement especially in non-treated or missed cases. Moreover,
studies should be conducted to determine if methionine levels
correspond to the appearance of cerebral white matter changes,
their progression and resolution./p>
We stress on the importance of family/patient education
to improve compliance with medications and follow the dietary
restriction. Clinicians should consider performing brain MRI
images at diagnosis and follow up studies for patients with classical
homocystinuria who have poor adherence to diet restriction with
rising methionine levels even in the absence of new neurological
findings.
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment