Postoperative Discomfort due to Peripheral Residual Nerve Blocks in Outpatients who had Carpal Tunnel Surgery-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Introduction: The purpose of this study was to compare the discomfort due to residual blocks between distal and proximal blocks.
Methods: The study was conducted on a pool of
ambulatory patients who had undergone open surgery for carpal tunnel
release under peripheral blocks. Patients returned home 2-3hours after
surgery. On the third postoperative day. They were called, and asked to
determine the discomfort caused by residual obstruction after discharge
from the hospital, on a verbal scale (absent, minor, slight, very
important and very important). According to the degree of discomfort, we
separated the patients into two groups that were compared with Fisher
exact tests and Student's t-test.
Results: Between November 2006 and January
2008, 185 patients were contacted on Day 3 and analyzed (105 distal BP
and 80 proximal BP).The age, sex, body mass index, the dominant side and
the operated side, smoking, postoperative pain scores did not differ
between groups. The muscolocutaneous nerve was blocked in 24 (22.9%)
patients who had a distal peripheral nerve block (distal BP) and in 63
(78.8%) of those who have had a proximal block (proximal BP) (p
<0.001). Overall, the distal BP induced less discomfort than promixal
BP (P = 0.041).
Discussion: This difference could be due to
the larger territory of the proximal BP. But the clinical impact of this
malaise seems limited since in both groups, 70 to 80% of patients
reported no discomfort or minor discomfort.
Keywords: Peripheral blocks; Carpal tunnel syndrome; Postoperative discomfort; Surveillance; Monitoring Summary
Introduction: The aim of our study was to
assess the discomfort due to residual distal and proximal blocks in
outpatients operated for carpal tunnel release.
Methods: The study was conducted on a cohort
of ambulatory patients having undergone open surgery for carpal tunnel
release in peripheral blocks. Patients went home 2-3hours after surgery.
On the third postoperative day. They were called, and were asked to
determine the discomfort caused by residual obstruction after discharge
from the hospital on a verbal scale (absent, minor, slight, very
important and very important). According to the degrees of discomfort,
we separated the patients into two groups and compared the two using the
Fisher exact test and Student's t-test.
Results: Between November 2006 and January
2008, 185 patients were contacted three days after their release and
analyzed (105 distal PNBs and 80 proximal PNBs). Age, gender, body mass
index, ASA score, postoperative pain scores were not different between
groups. The musculocutaneous nerve was blocked in 23% of distal PNBs and
in 81% of proximal ones (p<0.001). Overall, distal PNBs induced less
discomfort than proximal PNBs (p=0.041). Nevertheless, 20% of patients
with distal PNBs express mild to very important discomfort, versus 30%
of patients with proximal PNBs (p=0.124).
Discussion: Despite dramatic differences in
anaesthetised and paralysed territories between the two groups, wrist
PNBs induce only slightly less postoperative discomfort due to residual
block than proximal PNBs. Therefore, the clinical impact of this
discomfort seems limited since in both groups, 70 to 80% of patients
reported no or minor discomfort.
Introduction
Hand Surgery and particularly carpal tunnel is very common [1].
Peripheral nerve blocks were the techniques anesthetics frequently
used. They provide good surgical conditions and a better risk-benefit.
Two types were first disclosed for this surgery. This would be the nerve
block at the wrist [2] and nerve blocks at the brachial plexus or the humeral canal or axilla [3].
The choice of technique depends on the operators and indications but
they are comparable to anesthesia level. The main nerves to block in
carpal tunnel release surgery, are the median, ulnar and often the
musculocutaneous. There is talk of proximal peripheral block (PPB) when
the nerves are blocked at the axilla and distal peripheral block when
they are located at the elbow and wrist.
Whatever the technique, blocks allow street aptitude before the total lift of the block [4]. Nearly all patients go home with the residual effects of anesthesia [5].
We did not find any similar study on the blocks at the wrist. In
addition, the discomfort of residual blocks at the brachial channel have
not been compared with those of the blocks at the wrist.
The aim of our study was to evaluate discomfort from
distal and proximal residual blocks in ambulatory patients undergoing
carpal tunnel release surgery.
Methods
Patients
The study was conducted in the outpatient surgery
unit of a university hospital. This is a prospective observational study
which was conducted from January 2007 to June 2008. It did not require
application files to be submitted to the committee for the protection of
local people because it does not create a change the usual care of
patients. We have included all adult patients ASA 1-3 operated for
carpal tunnel syndrome in outpatient under loco-regional anesthetic
(LRA). Criteria for non-inclusion were: the refusal or inability to use
simple digital scales.
Intraoperative support
Wrist and brachial canal blocks were then explained
to patients after the agreement for intervention under LRA obtained
during the pre-anesthetic consultation. There was no oral premedication
but in the preanesthesic room, after standard monitoring, intravenous
sedation (1mg midazolam and sufentanil 5mcg) plus oxygen therapy (6L
/min) via a face mask was offered to patients before performing a LRA.
Blocks were performed either via ultrasound or neuro stimulator with the
same needle mark (Nanoline™, Pajunk™, Geisingen, Germany) 25mm for
blocks wrist and 50mm for brachial canal blocks. Mepivacaine 1.5%
(Carbocaine®AstraZeneca, Rueil- Malmaison, France) was used for all
patients. The LRA technique to the wrist was that described by maicaire
and for the brachial plexus blocks the Gaertner technique [6].
Before making the incision, the surgeon was tested the incision site
with the tip of the scalpel or pinching the area with dissection
forceps. When necessary, they completed the LRA by intraoperative local
infiltration of lidocaine 1%.
Post operative
During their stay in a post anesthesia care unit
(PACU), one of six members of the paramedical team, which did not
intervene in the prior management of the patient, asked them to self-
assess pain experienced during the LRA (related to the injection, to
electrical stimulation, injection of mepivacaine) at the withers and
during surgery. Patients then returned to their room or were started on
analgesics (paracetamol 1g*4/day and vitamin C-1g/j) (Afar). They were
then invited to eat and then get up. They left home two hours after the
end of the intervention.
Gathering information
Each subject was contacted by telephone 3days after
hospital discharge in accordance with outpatient protocol. After the
basic checks, the only additional check was «Having an anesthetized limb
bothered you: very much, a lot, some, a little, not at all» (Likert)
Statistics
Quantitative values are given as mean and standard
deviations and analyzed with a Student test. The distribution of scores
for discomfort is not Gaussian, and for more clinical relevance, these
scores from 0 to 10 were analyzed as a percentage of patients with a
score greater than 3/10, to take into account only moderate to severe
discomfort. The discomfort was assessed according to the anesthetic
technique, age, history. Qualitative values are given in absolute
numbers and as a percentage of the population studied. Statistics were
performed using the PASW Statistics 18 (SPSS Inc., Chicago, IL)
software. Values of p<0.05 were considered significant.
Results
Between November 2006 and January 2008, 185 patients
were included and analyzed at postoperative day 3- 105 BP distal and 80
BP proximal.
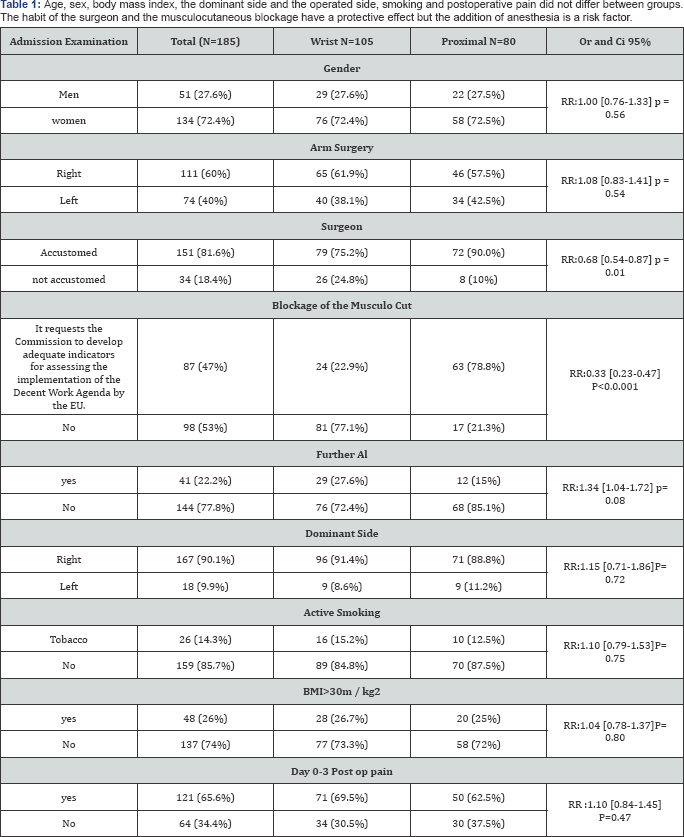
Board
The distribution of patients according to the type of
anesthesia. Our population was divided into 134 women and 51 men. Age,
sex, body mass index, the dominant side and the operated side, smoking
and postoperative pain did not differ between groups. The average age
was 55.85±12.26 years in the wrist group and 57.08±12.28 years in the
proximal group. The weight, height and BMI were respectively
75.39±18.18kg; 164.33±6.9cm; 27.87±6.21kg/m2 wrist and
71.15±15.64kg; 162.95±9.17cm; 26.76±5.51kg/m2 proximally. The average
doses of mepivacaine 1.5% to 17.86±23.14±3.24ml and 4.25ml in each
group.
The average duration of tourniquet was similar with 13.19±3.01mn for the wrist group and 12.96±2.98mn proximally. Table 1
summarizes the distribution of the population by type of anesthesia.
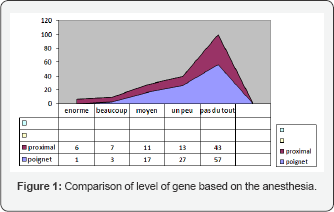
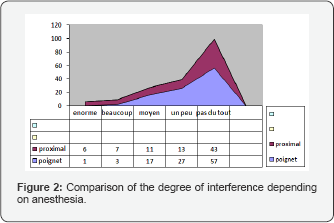
The peroneal nerve was significantly blocked proximally 63(78.8%)
against 24(22.9%) P<0.0.001. Figure 2 &1
showed that overall the LRA is well tolerated with 17(9.2%) of the
genes greater than 3. The proximal blocks gene was significantly higher
than the wrist blocks 4(3.9%) against 13(16.3%) p = 0.04?
Discussion
Wrist blocks induced less discomfort than brachial
canal blocks. But overall incidence was lower at around 9%. The peroneal
nerve was frequently blocked proximally. But this data is not reliable.
It could be blocked because of its proximity to the radial wrist. It is
extremely difficult to obtain reliable and consistent data on the
incidence of postoperative discomfort due to the residual effects of the
LRA. Retrospective studies estimated the incidence of discomfort to be
0.5-1.0%, but a prospective study suggests an incidence of 10-15%. In
view of all studies, the existence of discomfort directly attributed to
the nerve block in carpal tunnel surgery remains controversial and is
all clearly dependent on the definition of discomfort [7].
As many risk factors may be considered in the
occurrence of post operative discomfort. A study done in the US shows
that the incidence of postoperative complications of peripheral nerve
blocks was not modified by the use of ultrasonography [8]. Surgery could also cause discomfort. Uroš Ahčan [9]
showed in a comparative study between the conventional technique and by
macroscopic endoscopic visualization of the entire transverse carpal
ligament a significant reduction in post operative discomfort after
carpal tunnel surgery. This technique could avoid injuries subcutaneous
palmar nerve terminal branch of the musculocutaneous. He further asserts
that there are several individual anatomical variations which are
difficult to predict.
The density of skin nerve endings that criss-cross
from the hand to the trunk further increases the risk of injury. Another
explanation for the post-block discomfort is the etiology underlying
several pathologies with nerve damage may favor the occurrence of post
operative discomfort after LRA [10].
The most cited were tenosynovitis in rheumatoid arthritis, nonspecific
chronic tenosynovitis or fibrosis, radius fracture in the wrist, Colles'
fracture, carpal arthrosis, scaphoid nonunion, the wrist trauma,
diabetes mellitus, thyroid disease, pregnancy, birth control pills,
lymph nodes, muscle hernia or lipomas in the carpal tunnel. Anesthesia
consultation still does not diagnose preexisting nerve injuries. Even
when the diagnosis is made, there is no direct correlation between the
etiology and nerve damage.
Conclusion
Peripheral nerve blocks provide are significantly
beneficial. But could increase the risk of discomfort after surgery in
ambulatory patients. The density of skin nerve endings decreases from
the hand to the trunk; the individual anatomical variability; the
underlying pathologies make it difficult to complete exploration before
surgery. Distal blocks are preferred, first direct visualization of
nerves through ultrasound and prefer new surgical techniques is to be
encouraged. Though a minor surgery, carpal tunnel can hide a nervous
pathology that could compromise the contribution of the LRA. The
postoperative day 3 postoperative gene could be a warning sign for a
neurological follow up with the involvement of all participants.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment