Thoracic Epidural Analgesia Lessens Inflammatory Response to Coronary Artery Bypass Grafting Surgery -Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Objectives: To evaluate the effects of
preoperative thoracic epidural analgesia (TEA) on inflammatory response
of patients undergoing on- pump coronary artery bypass graft (CABG)
surgery under general anesthesia (GA).
Patients & Methods: Eighty-eight patients
were divided into two groups; Group TEA received TEA and GA and Group GA
received GA alone. Blood samples were collected preoperatively (T0), 4-hr (TJ, and one (T2) and two (T3)
days after surgery for ELISA estimation of serum interleukin (IL)-1β,
IL-6, IL-10 and tumor necrosis factor (TNF)-α. Intraoperative (IO) and
postoperative (PO) data were collected.
Results: Patients of group E had significantly
lower IO hemodynamic measures, shorter time for hemostasis and wound
closure and less IO blood loss than patients of group G. Amount of 1st
PO day wound drainage was significantly less, and durations of
mechanical ventilation (MV), ICU stay and PO hospital stay were
significantly shorter in group TEA. Patients of group E had
significantly lower individual and collective pain scores. All patients
showed significantly higher levels of estimated cytokines compared to
preoperative levels. Patients of group E showed significantly lower
serum IL-1β, IL-6 and TNF-α with significantly lower serum IL-10 levels
compared to patients of group GA.
Conclusion: TEA provided significantly better
control on inflammatory response during on-pump CABG in favor of
anti-inflammatory arm. Continuous epidural analgesia during ICU stay
significantly shortened duration of MV and ICU stay with reduction of
need for opioid. Pain control provided by TEA allowed PO early
ambulation, rehabilitation and short hospital stay.
Keywords: Thoracic epidural analgesia; Inflammatory response; CABG Introduction
Coronary artery bypass grafting (CABG) surgery
remains the preferred treatment in patients with complex coronary artery
disease [1].
However, CABG has inherent impacts on multiple organ systems that could
be attributed to altered inflammatory system functions [2]. Cardiopulmonary bypass (CPB) procedures are thought to activate systemic inflammatory reaction syndrome [3] and comparative studies found off-pump surgery could attenuate the CABG-associated inflammatory response [4,5].
Various drugs administered during anesthetic
procedure were tried to reduce inflammatory response during on-pump
CABG. Desflurane anesthesia induced lower concentrations of interleukin
(IL)-8 and IL-6 [6], methyl-prednisolone [7] and dexamethasone [8] decrease levels of IL-6 and increase antiinflammatory activity through IL-10 [7].
Also, dexmedetomidine reduced circulating IL-1, IL-6, tumor necrosis
factor-α (TNF-α), and interferon-γ levels after mini-CPB [9].
Epidural anesthesia is a central neuraxial block
technique with many applications. It is a versatile anesthetic technique
that can be used as an anesthetic, as an analgesic adjuvant to general
anesthesia, and for postoperative analgesia [10].
The current prospective comparative study aimed to
evaluate the effects of preoperative thoracic epidural analgesia (TEA)
on inflammatory response of patients undergoing CABG surgery under
general anesthesia (GA).
Patients & Methods
The current prospective study was conducted at
Departments of Anesthesia and Cardiovascular Surgery at Nasser
Institute. The study protocol was approved by Local Ethical Committee.
Patients signed fully informed written consent were randomly; using
sealed envelopes prepared by blinded assistant and chosen by patients,
allocated into two equal groups: Group TEA included patients will
receive TEA as adjuvant to inhalational GA and Group GA included
patients will receive inhalational GA alone.
Anesthetic Technique
All patients were taken into the operating room
unpremedicated and after standard non-invasive monitoring, Lactated
Ringer's solution was started. In Group E epidural catheter was inserted
before induction of anesthesia using the loss of resistance technique. A
20 gauge epidural catheter (Prefix 401, B. Braun, Melsungen AG) was
inserted through an 18-gauge Tuohy needle that was placed at the T1-2
interspace and advanced 3 to 5 cm into the epidural space. An initial
bolus of 10ml ropivacaine 0.75% was injected and followed by continuous
infusion of ropivacaine 2% at rate of 10ml/hr. Sensory block was
ascertained by sensory loss to needle prick.
For both groups, general anesthesia was induced with
midazolam (0.05mg/kg) as a pre-anaesthetic medication, propofol
(1-2mg/kg), fentanyl (1-2μg/kg), and atracurium (0.5mg/kg). After
tracheal intubation, lungs were ventilated with 100% O2 using a
semi-closed circle system, with a tidal volume of 6-8ml/kg, and the
ventilatory rate was adjusted to maintain end tidal CO2 between
35-40mmHg. Anesthesia was maintained by sevoflurane 2% and atracurium
injection was adapted to the patient's physiological reaction to
surgical stimuli. Heart rate (HR), systolic, diastolic, mean arterial
blood pressure (MAP) and oxygen saturation were invasively monitored
throughout the surgery. Patients of group GA received fentanyl infusion
(2μg/ kg/hr) as intraoperative analgesia. Postoperative (PO) pain was
evaluated using the visual analogue score (1-10 points) and rescue
analgesia for both groups was given at VAS of ≥4 as intramuscular
mepridine (50-100mg).
Collected operative data included number of grafted
vessels, aortic cross clamping (CCT), cardiopulmonary bypass (CPB) and
total operative times. Duration of ICU stay, amount of chest tube
drainage, and the frequency of PO events were recorded.
Laboratory Investigations
Blood samples were collected from preoperatively
(T0), 4-hr (T1), one (T2) and two (T3) days after surgery. Separated
serum was stored at -80°C until assayed for ELISA estimation of serum
IL-1β (Quantikine ELISA kit from R & D Systems, Inc., Minneapolis,
MN, USA) [11], IL-10 (Milenia®, DPC Biermann, Bad Nauheim; Germany) [12], IL-6 [13] and TNF- α (Pelikine™ Inc., Concord, USA) [14].
Statistical Analysis
Sample size was calculated using the standard nomogram proposed by Kraemer & Thiemann [15]
and a sample size of >40 patients was determined to be sufficient to
detect a difference at the 5% significance level and give the trial 80%
power (16). Obtained data were analyzed using One-way ANOVA with post-
hoc Tukey HSD Test and Chi-square test (X2 test) using the SPSS (Version
15, 2006) for Windows statistical package. P value <0.05 was
considered statistically significant.
Result
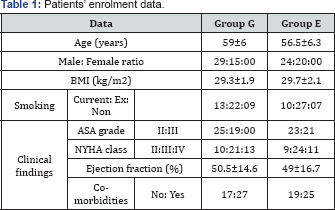
BMI: Body Mass Index; ASA grade: American Society of Anesthesiology; NYHA: New York Heart Association
The study included 88 patients assigned for isolated CABG (Table 1).
Intraoperative hemodynamic measures were nonsignificantly (p>0.05)
lower in group TEA till 30-min after induction of GA; then the
difference became significantly (p<0.05) lower in group TEA till the
end of surgery (Table 2 & Figure 1).
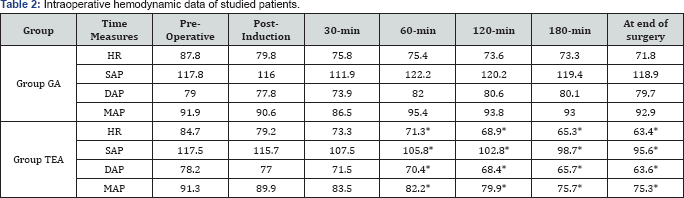
Data are presented as mean±SD; HR: Heart Rrate; SAP:
Systolic Arterial Pressure; DAP: Diastolic Arterial Pressure; MAP: Mean
Arterial Pressure; *: Significance Versus Control Levels
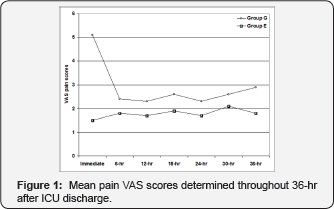
Operative data showed non-significant difference
between both groups. Patients of group TEA showed significantly lower
amount of 1st PO day wound drainage, and durations of mechanical
ventilation and ICU stay. Pain scores, determined throughout 1st 36-hr
afterward transfer, were significantly lower in patients of TEA group
than those of group GA (Fig. 1)
with significantly lower collective 36-hr pain score. Mean total
duration of hospital stay was significantly shorter in group TEA
compared to group GA (Table 3).
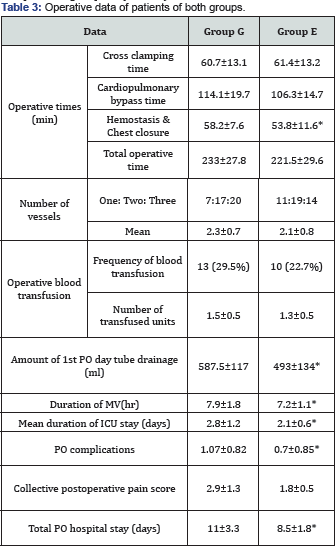
Data are presented as mean±SD, ratios & numbers; percentages are in parenthesis; *: significant difference versus group GA
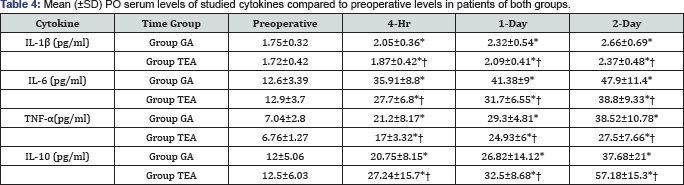
Preoperative serum cytokine levels showed
non-significant (p>0.05) difference between studied patients. All
patients showed significantly (p<0.05) higher PO cytokines levels
compared to preoperative levels with significantly higher serum IL-1β,
IL-6 and TNF-α and significantly lower serum IL-10 levels in patients of
group G compared to patients of group E. This significant difference
persisted till 2-day PO (Table 4).
Postoperative serum levels of inflammatory cytokines
were significantly higher, while levels of anti-inflammatory cytokine
were with significantly lower compared to preoperative levels; a finding
that illustrates the stress imposed by CABG surgery on immune system
and supported that previously reported in literature [17-21].
However, thoracic epidural analgesia (TEA) significantly lessened this
effect compared to general anesthesia (GA) alone. These findings
illustrated the beneficial effects of epidural analgesia on
surgery-induced activation of immune system and supported that
previously reported by Bach et al.[22] and Palomero Rodriguez et al. [23]
who reported that TEA as a part of a combined anesthesia attenuated the
inflammatory response to cardiac surgery with CPB. Moreover, Caputo et
al. [24]
detected significantly lower IL-6 and IL-8 levels with significantly
higher levels of IL-10 with combined GA and ETA than in GA alone in
patients underwent off-pump CABG. Also, Zawar et al. [10]
found combined TEA with GA decreased IL-6 at day 2, TNF-α at day 2 and 5
and concluded that TEA decreases inflammatory response to CABG.
Patients received TEA showed significantly lower pain
score and rescue analgesia consumption for 36-hr after extubation. This
allowed early ambulation and favorable outcome. Such outcome supported
that previously documented that TEA provided better analgesia with
significantly reduced pain intensity and analgesic consumption in early
PO period after CABG (El-Morsy & El-Deeb [25], Gurses et al. [26], Onan et al. [27] and Porizka et al. [28].
Patients received TEA enjoyed significantly better PO
course with significantly shorter duration of MV and ICU stay. This
could be attributed to the better control on inflammatory response in
favor of anti-inflammatory direction and the perfect control of pain
that allowed freer chest movement with subsequent better lung
ventilation, thus reducing postoperative MV-induced complications.
Additionally, TEA minimized the need for opioid with its sedative and
possible respiratory inhibition effects thus allowed earlier weaning of
MV and ICU discharge.
These data go in hand with El-Morsy & El-Deeb [25]
who reported that in elderly CABG patients, TEA reduced severity of PO
pulmonary dysfunction with faster restoration of normal function and
significantly higher PaO2, lower PaCO2, thus resulting in earlier
extubation and awakening. Moreover, Gurses et al. [26]
found PO need for vasodilator, transfusion; analgesics, extubation time
and duration of stay in ICU were significantly lower in TEA group of
CABG patients compared to GA group. Also, Neskovic et al. [29]
reported that combination of GA with TEA appears to be good choice
during synchronous carotid endarterectomy and OPCAB due to advantages of
early extubation and early neurological assessment. Recently, in 2016;
Porizka et al. [28] and Barbosa et al. [30] reported significantly shorter time to extubation and lower ICU stay of CABG patients received TEA.
Furthermore, patients had combined GA and TEA showed
significantly lower amount of mediastinal drainage on 1st PO day; mostly
due to better intraoperative hemodynamic control secondary to
significantly lower blood pressure so minimizing bleeding and
subsequently decreased PO oozing and collection. Similarly, Gurses et
al. [26]
reported significantly lower intraoperative MAP, need for transfusion,
whereas cardiac output and index, hematocrit values were significantly
higher; and postoperative MAP, HR, hypertension development were
significantly lower with TEA compared to GA.
In addition, patients received TEA showed
non-significantly lower frequency of PO events, but had significantly
shorter duration of hospital stay. In line with such outcome, Zawar et
al. [10], Gurses et al. [26] and Porizka et al. [28] reported significantly shorter duration of hospital stay in TEA group compared to GA group. Also, Barbosa et al. [30], found combined TEA and GA showed lower incidence of arrhythmias and lower ICU and hospital stay and Stenger et al. [31]
reported significantly lower frequency of PO dialysis and myocardial
infarction and 6-m mortality rate of cardiac surgery patients received
supplemental TEA to GA.
In line with outcomes of the current study and in
support of the efficacy of TEA for patients undergoing CABG, multiple
studies approved efficacy of combined TEA and GA for cardiac surgery in
obese patients [32], chronic obstructive pulmonary disease patients [33] elderly cardiac surgery patients [34] and even in high risk cardiac surgery patients [35].
Multiple experimental studies tried to evaluate the beneficial effects of TEA for patients undergoing CABG; Bedirli et al. [36]
using a rat model of mesenteric ischemia/reperfusion found TEA
significantly decreased cytokine, malondialdehyde, and myeloperoxidase
levels and increased antioxidant enzyme levels with significantly
decreased intestinal injury score and percentage of apoptotic cells.
Onan et al. [37] using immunocytochemistry showed that TEA increased
internal thoracic artery free blood flow significantly via increased
vascular endothelial growth factor and inducible nitric oxide synthase
expressions and recommended the use of TEA as an adjunct to GA as an
alternative to vasoactive agents for increasing internal thoracic artery
blood flow during CABG surgery.
Conclusion
TEA provided significantly better control on
inflammatory response during on-pump CABG in favor of anti-inflammatory
arm. Continuous epidural analgesia during ICU stay significantly
shortened duration of MV and ICU stay with reduction of need for opioid.
Pain control provided by TEA allowed PO early ambulation,
rehabilitation and short hospital stay.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment