Pulmonary Aspiration during Induction of General Anesthesia in a Patient with Chronic Inflammatory Demyelinating Polyneuropathy-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Chronic inflammatory demyelinating polyneuropathy
(CIDPJ-a rare immune-mediated disorder affecting the peripheral nervous
system-is the most common treatable neuropathy. Its clinical features
include progressive or relapsing muscle weakness and decreased motor
ability and or sensation in the extremities. Patients with CIDP are not
encountered frequently in the operating room; thus, there is
insufficient knowledge regarding their anesthetic management. Here, we
report a case of pulmonary aspiration during induction of general
anesthesia in a 64-year-old man with CIDP undergoing emergency surgery
for gastric ulcer perforation.
Keywords: Piriformospora indica; Pulmonary aspiration; Chronic inflammatory demyelinating polyneuropathy; General anesthesiaAbbreviations: CIDP: Chronic Inflammatory Demyelinating Polyneuropathy; MNGIE: Mitochondrial Neurogastrointestinal Encephalomyopathy; Fio2: Fraction of Inspired Oxygen; Hb: Hemoglobin; Paco2: Partial Pressure of Carbon Dioxide; Pao2: Partial Pressure of Oxygen; Spo2: Oxygen Saturation; POD: Post-Operation Day
Introduction
Chronic inflammatory demyelinating polyneuropathy
(CIDP) is a rare neurologic disorder of the peripheral nervous system.
Clinically, it presents with gradual muscle weakness that is typically
symmetric and characteristically involves the proximal and distal
muscles. It usually develops over more than 2 months with relapse [1].
There are only a few articles regarding anesthetic management of
patients with CIDP and there are no reports on the possible
complications during induction of anesthesia in such patients. Here, we
report a case of pulmonary aspiration during induction of general
anesthesia in a patient with CIDP.
Case Report
A 64-year-old man (weight, 50kg) was hospitalized in
the neurology department with a headache. His medical history included
CIDP, chronic obstructive pulmonary disease, chronic hepatitis C,
diabetes mellitus, and hypertension. He also had undergone subtotal
gastrectomy (Billroth I) for gastric cancer approximately 4 years prior.
On the fourth day of hospitalization, the patient complained of sudden
abdominal pain. The air- fluid level was confirmed on chest radiography.
Gastric ulcer perforation was suspected, and emergency surgery was
scheduled.
The patient was not premedicated prior to induction
of anesthesia, and he had fasted for over 14 hours. He received 100%
oxygen for 3 minutes with spontaneous ventilation. Anesthesia was
induced with 50mg propofol and 2mg/hr remifentanil intravenously,
followed by 20mg cisatracurium. Immediately after administration of
anesthetic drugs, the patient began projectile vomiting. Abundant
blackish material was removed from the oral cavity and tracheal
intubation was performed. After intubation, his oxygen saturation
decreased to 55% and his right lung sounds also decreased. Suction
through the endotracheal tube was performed quickly. Mechanical
ventilation with 100% oxygen improved his oxygen saturation to 90%, but
his blood pressure decreased to 70/40mmHg. Norepinephrine was
administered, and his vital signs stabilized. Intraoperative anesthesia
was maintained with 100% oxygen (2 L/min), sevoflurane (1.5-2 vol%),
remifentanil (1-2mg/hr), and cisatracurium. Wedge resection of the
stomach with feeding jejunostomy was performed successfully.
After surgery, the patient was transferred to the
surgical intensive care unit. He was diagnosed as having aspiration
pneumonia, and treatment with antibiotics, inotropic agents, mechanical
ventilation, and supportive care was initiated. Arterial blood gas
analysis was performed daily (Table 1).Despite
this treatment, his aspiration pneumonia did not improve. On the second
postoperative day, bronchoalveolar lavage via bronchoscopy was
performed. Subsequently, pulmonary infiltrates tended to wax and wane,
and his other vital signs and respiratory parameters remained stable. On
the tenth postoperative day, chest radiography showed increased
haziness over both lung fields (Figure 1). The patient's condition worsened, and he died the following day.
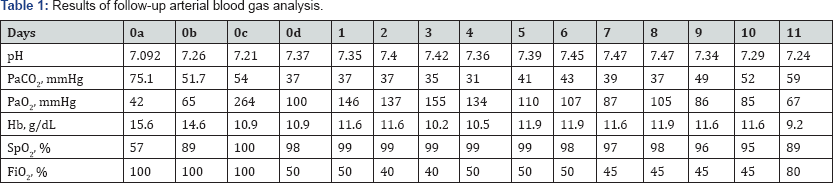
Postoperative days: 0a: immediately after
pulmonary aspiration; 0b: 1 hour after pulmonary aspiration; 0c:
immediately after intensive care unit arrival; 0d: 10 hours after
intensive care unit arrival.
Abbreviations: Fio2: Fraction of Inspired
Oxygen; Hb: Hemoglobin; Paco2: Partial Pressure of Carbon Dioxide; Pao2:
Partial Pressure of Oxygen; Spo2: Oxygen Saturation

Discussion
Pulmonary aspiration is a well-known severe
complication of anesthesia. Aspiration of gastric contents has been
associated with acute lung injury characterized by pulmonary edema,
severe diminished gas exchange, and progression to acute respiratory
distress syndrome. In a recent review, prevalence of pulmonary
aspiration was reported to be 1 in 8,600 anesthetic procedures [2].
Most cases occur during induction of anesthesia, or, less frequently,
during extubation and recovery. The clinical manifestations of pulmonary
aspiration depend on the nature, quantity, and distribution of the
material aspirated, as well as the relative impact of the acidic,
bacterial, and particulate content, and other patient-related factors.
Major risk factors for pulmonary aspiration include pregnancy after the
first trimester and acute gastrointestinal disease, particularly
esophageal or gastric disease, decreased esophageal or gastric motility,
small bowel obstruction, and ileus. Other risk factors for
gastrointestinal stasis include trauma, diabetes, obesity, and
administration of drugs that inhibit gastrointestinal function.
Preoperative fasting for at least 6 hours after consumption of a light
meal or nonhuman milk and 2 hours after clear liquids (e.g., water,
clear tea, black coffee) is also important. If the patient is determined
to have a high potential for pulmonary aspiration, nasogastric tube
placement is useful for reducing aspiration during induction of
anesthesia.
Our patient had fasted sufficiently (>14 hours),
and a nasogastric tube was maintained. Despite these conditions, he
aspirated gastric contents during induction of general anesthesia. Kim
et al. reported that Billroth I reconstruction after subtotal
gastrectomy was associated with delayed gastric emptying (12 of 378
patients (3.2%)) [3]. However, gastric motility returned in 3 to 6 weeks in most patients [4].
Our patient had undergone Billroth I surgery 4 years prior, which
should have been sufficient time to improve delayed gastric emptying.
Patients with CIDP rarely exhibit decreased
gastrointestinal motility. Progressive forms of CIDP carry a poorer
prognosis than relapsing forms. For example, difficulty swallowing is a
common symptom in progressive forms [5].
In the present case, the patient had progressive upper and lower limb
weakness and difficulty swallowing for over 3 months prior to admission.
He had been diagnosed as having CIDP based on his clinical forms [5].
In the present case, the patient had progressive upper and lower limb
weakness and difficulty swallowing for over 3 months prior to admission.
He had been diagnosed as having CIDP based on his clinical history and
electrophysiologic studies. According to his history, he had difficulty
swallowing, dysphagia, and occasionally aspirated food when eating.
Therefore, we suggest that CIDP is a risk factor for pulmonary
aspiration during induction of anesthesia.
There have been several reports of cranial nerve involvement in CIDP. Teramoto et al. [6] reported relapse with dysphagia in a patient with CIDP with involvement of the glossopharyngeal and/or vagus nerve [6].
They also showed that intravenous immunoglobulin was effective for CIDP
with dysphagia. Our patient complained of dysphagia, difficulty
swallowing, slurred speech, ptosis, and diplopia, which indicated
cranial nerve involvement, but electrophysiologic studies showed normal
values. Intravenous immunoglobulin may be effective for CIDP with
dysphagia that does not resolve with steroid therapy; however, in our
patient, we did not have the opportunity to administer this treatment.
Differential diagnosis of CIDP should include mitochondrial neurogastrointestinal encephalomyopathy (MNGIE) [7]. Incidence of mitochondrial disease (1 in 500) is more frequent than that of CIDP (1.6 in 100,000) [8,9].
Gastrointestinal and neurologic symptoms are the most common findings
in MNGIE. Pathology outside the peripheral nervous system and elevated
serum lactate level are what differentiates MNGIE from CIDP Our patient
had gastrointestinal symptoms, but he did not have an elevated serum
lactate level. Although there is insufficient knowledge regarding
anesthetic management of patients with CIDP, MNGIE is known to be
associated with respiratory failure, cardiac depression, conduction
defects, and dysphagia.
The manifestations of pulmonary aspiration include
acute onset of dyspnea, tachypnea, bronchospasm, cyanosis, pulmonary
edema, hypotension, and hypoxemia, which may progress rapidly to severe
acute respiratory distress syndrome and death. These manifestations vary
depending on the volume and nature of the material aspirated. Our
patient had received treatment with antibiotics, inotropic agents,
mechanical ventilation, bronchoalveolar lavage, and supportive care.
Pulmonary infiltrates tended to wax and wane, but his aspiration
pneumonia did not improve clearly. We had planned on weaning him from
mechanical ventilation after tracheostomy. However, on the 11th
postoperative day, his vital signs were unstable, his respiratory
parameters worsened, and he eventually died. There is no clear reason
for the clinical deterioration of this patient. We suggest that his
aspiration pneumonia may have led to severe septic shock.
Currently, there are no anesthetic guidelines for patients with CIDP. There are only several case reports to use as guidance [10,11].
According to these case reports, regional anesthesia can be
administered safely, and the effect of rocuronium can be prolonged in
general anesthesia. However, ours is the first report of pulmonary
aspiration during induction of anesthesia in a patient with CIDP. For
safe anesthetic management of patients with CIDP, more research is
required.
Conclusion
In conclusion, pulmonary aspiration may occur during
induction of anesthesia in patients with CIDP. Recently, increased
monitoring of anesthetic care outside the operating room has been
suggested. Anesthesiologists and physicians should keep in mind the
possibility of aspiration in patients with decreased gastrointestinal
motility.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment