The Effectiveness of Esmolol in Attenuating the Arousal Response (Heamodynamic Changes and Bis Index) to Endotracheal Intubation in Patients Undergoing Surgical Procedures-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Introduction
Measurement of anaesthetic depth is a challenging
task for the anaesthesiologist. Ever since the first modern anaesthetics
(ether, chloroform, and nitrous oxide) were used in the 1840, doctors
have been searching for a reliable method of measuring the depth of the
patient's unconsciousness. Research has indicated that patient's
attitude towards undergoing surgery is affected by the possibility of
awakening during the procedure. Post-traumatic stress disorder (PTSD) is
a common result of awareness episodes. [1,2].
There are several reasons for anesthesiologist’s difficulty in evaluating dosages of anesthetic agents:
- The lack of a universally accepted definition of "consciousness".
- The complex effects of anesthesia on the human organism.
- The increased use of combinations of anesthetic agents rather than single drug.
- Changes in the patient's response to anesthesia over the course of the operation.
- Age and sex related differences in responsiveness to specific anesthetics.
- Large differences among individuals apart from age or sex groupings in regard to sensitivity to anesthesia [3].
A variety of different physiological responses have
also been used in attempts to indirectly measure the depth of a
patient’s unconsciousness under anaesthesia. Most people use
haemodynamic responses- the patient's blood pressure and heart rate as
basic guidelines for adjusting the amount of anaesthetic agent delivered
to the patient during surgery. Other direct measurements have been
based on the movements of the patient's body during surgery, hormonal
responses, sweating, eye movement, and the reactivity of the eyes to
light [4,5].
In contrast, a technology that would permit
independent neurophysiologic monitoring of the central nervous system
would provide a direct measure of brain status during anesthesia and
sedation, allowing clinicians to finely tune perioperative management
and achieve the best possible outcome for each patient. Accurate
monitoring and targeting of brain effect, in combination with assessment
of clinical signs and traditional monitoring, would permit a more
complete approach to adjusting the dosing and mixture of anaesthetic,
sedative and analgesic agents.
Indirect methods that allow an observer to assess a
person's level of awareness have been used since the early 1970. The
earliest and most widely used instrument for evaluating impaired
consciousness is the Glasgow Coma One difficultly that has emerged from
these attempts at direct measurement is that that they are not good
predictors of the likelihood of awareness during surgery or recall of
the procedure after surgery.
Another measurement that researchers have explored in
their attempts to measure depth of anesthesia directly is the
electroencephalogram (EEG). The EEG is a complex recording of the
electrical activity of the nerve cells in the brain. In 1931 Berger
discovered that brain waves change in amplitude and frequency when a
person is asleep or anaesthetized; they slow down, shift to lower
frequencies, and become more closely synchronized with another.
Bispectral index
It is a numeric index that directly reflects the
activity of cerebral cortex and correlate with level of consciousness.
It is the latest system used in anesthesiology to measure the effects of
specific anaesthetic drug on the brain and to track changes in
patient's level of sedation and hypnosis. In technical terms, the
Bispectral index itself is a complex mathematical algorithm that allows a
computer inside an anesthesia monitor to analyze data from a patient’s
electroencephalogram during surgery. BIS was first developed in early
1990 and has been used since 1997, It is a type of automated direct
measurement of the patient's condition in comparison to the Glasgow coma
scale or similar scoring systems, which are indirect assessment of
sedation [6].
The Bispectral Index (BIS) is a measure of the
effects of anesthesia and sedation on the brain, a new "vital sign" that
allows clinicians to deliver anesthesia with more precision and to
assess and respond more appropriately to a patient’s changing condition
during surgery. It is a numeric index that directly reflects the
activity of cerebral cortex and correlates with the level of
consciousness.
BIS monitoring supports three key elements of anaesthesia are:
- Vigilance
- Diagnostic decision-making
- Therapeutic targeting
Therapeutic targeting is a clear benefit that results
from BIS monitoring. Using this new parameter, the clinician can manage
patients within the optimal plane of anesthesia effect, reducing the
unwanted occurrence of excessive or inadequate anesthetic effect.
Clinical investigations of BIS monitoring during anesthesia have
consistently demonstrated an average 25% reduction in intra operative
anesthetic use and a consistent reduction in the time for emergence from
general anesthesia.
The key EEG features identified from the database
analysis characterized the full spectrum of anaesthetic induced changes
and included:-
- Degree of beta or high frequency (14-30 Hz) activation,
- Amount of low frequency synchronization,
- Presence of nearly suppressed periods within the EEG
The BIS is an empiric, statistically derived
measurement. The key hypothesis underlying the development of BIS was
that some combination of EEG features (e.g. bispectral, power spectral
or other) could be identified and shown to be highly correlated with
sedation and hypnosis, regardless of the agent used to produce that
clinical state. The BIS was derived by analyzing a large database of
EEGs from subjects who had received one or more of the most commonly
used hypnotic agents [7,8].
The normal neural EEG activity of higher frequency
(alpha and beta rhythms) is converted to slower frequencies (delta and
theta rhythms) during deep anaesthesia, due to direct suppression of
cortical activity or by depression of pacemaker regulation. It further
increases the amplitude of EEG (synchronization) leading to 'burst
suppression'. On the other hand arousal characteristically decreases
amplitude (desynchronization).
BIS calculates three sub parameters.
1) Burst suppression with two separate algorithms
a. Burst Suppression Ratio (BSR)
b. QUAZI
2) Beta Ratio
3) Synch fast slow
The BSR is the proportion of the suppressed EEG
(isoelectric) in an epoch, the Beta ratio is the log ratio of the power
in the two empirically divided frequency bands (high and medium
frequency ranges) and Synch fast slow is the relative Bispectral power
in the 40-70 Hz frequency band. The Bispectral analysis examines the
relationship between the sinusoids at the two primary frequencies, f1
and f2, and a modulation component of the frequency f1+f2. The set of
these three frequency component is known as triplet.
After processing, a database is created describing
the EEG- derived sub parameters and the corresponding clinical state
(level of consciousness).
Each parameter has a particular stage of anesthesia
where it performs more accurately. The Beta ratio parameter reflects
light sedation; Synch fast slow detects surgical levels of anaesthesia,
and the burst suppression ratio (BSR) and QUAZI predominate during deep
levels of anaesthesia. Multi-variate, statistical models were used to
derive the optimum combination of the features, which then was
transformed into a linear dimensions scale from 0 to 100 [9].
Prospective clinical trials have demonstrated that
maintaining BIS Index values in the range of 40-60 ensures adequate
hypnotic effect during general aesthesia while improving the recovery
process. During sedation care, BIS Index values >70 may be observed
during adequate levels of sedation but may have a greater probability of
consciousness and potential for recall.
The BIS Index provides a direct measurement of brain
status, not the concentration of a particular drug. For example, BIS
Index values decrease during natural sleep as well as during
administration of an anaesthetic agent. The decrease produced during the
natural process of sleep, however, is not to the degree caused by high
doses of propofol, thiopental or volatile anaesthetics. The BIS Index
values reflect the reduced cerebral metabolic rate produced by most
hypnotics. Using positron emission tomography, a significant correlation
between BIS Index values and reduction in whole brain metabolic
activity was measured [10].
BIS Index monitoring can allow delivery of anesthesia
care that is safer, more precise and more pleasant for the patient. In
combination with assessment of clinical signs and traditional
monitoring, the BIS monitoring can facilitate balanced hypnotic and
analgesic administration with ensuring adequacy of anaesthesia. Various
measures to be taken during a sudden increase or decrease of BIS values
are as below:-
Responding to sudden BIS increase:
- Examine for the presence of artefacts (EMG, electrocautery or high frequency signals).
- Ensure that anaesthetic delivery systems are operating properly so that the intended dose of anaesthetic agent is reaching the patient.
- Ensure that the anaesthetic dose is sufficient.
- Assess the current level of surgical stimulation.
Responding to sudden BIS decrease:
- Assess for new pharmacologic changes.
- Assess the current level of surgical stimulation.
- Consider decrease as possible response to administration of muscle relaxants.
- Assess for other potential physiologic changes.
- Assess for emergence from anaesthesia [11].
BIS monitoring during endotracheal intubation
During endotracheal intubation, one general goal of
the anaesthesia provider is to minimize cardiovascular stimulation, thus
preventing resultant hypertension and tachycardia. Several strategies
are commonly used to blunt the blood pressure and heart rate response
including:
- Sufficient dosing of intravenous induction agent (e.g., propofol, thiopental)
- Opioid supplementation (e.g., fentanyl) [12]
- Administration of intravenous or tracheal lidocaine [13]
- Administration of antihypertensive (e.g., esmolol)
- Alternative intubation methods (e.g., fiberoptic intubation)
Several studies have examined the BIS responses
during endotracheal intubation to better understand the relationship
between cortical CNS and cardiovascular responses. Quite often, a
transient increase in BIS value (ΔBIS) can be observed following
tracheal intubation or other stimulation. Studies have demonstrated that
BIS responses do not directly correlate with the change in blood
pressure following laryngoscopy and intubation.
Laryngoscopy as well as tracheal intubation is one of
the most stressful times in the period of anesthesia for the patient.
It is associated with significant changes in the hemodynamics i.e.
increase in heart rate and blood pressure as well as an arousal response
as quantified by BIS.
Various agents have been used to attenuate these
reflexes and reduce hemodynamic changes these include opoids,
ɑ2-agonists like clonidine, local anesthetics like lidocaine, adrenergic
blocking agents like esmolol and vasodilating agents like sodium
nitroprusside and nitroglycerine [14,15].
Several studies have examined the BIS responses
during endotracheal intubation to better understand the relationship
between cortical CNS and cardiovascular responses. Quite often, a
transient increase in BIS value (Δ BIS) can be observed following
tracheal intubation or other stimulation. Studies have demonstrated that
BIS responses do not directly correlate with the change in blood
pressure following laryngoscopy and intubation.
Patients with controlled hypertension have
demonstrated an exaggerated blood pressure response, while their BIS
response was no different than normotensive individuals. BIS responses
to stimulation associated with laryngoscopy and intubation can be
markedly attenuated in a dose-dependent fashion.
Esmolol, a short-acting (β1-adrenoceptor
antagonist, produces dose-dependent attenuation of the adrenergic
response to laryngoscope and orotracheal intubation. However, previous
studies assessing the effectiveness of esmolol in blunting the
hemodynamic alterations induced by laryngoscope and orotracheal
intubation failed to monitor electrical activity of the brain. Only a
few studies have evaluated the effect of interaction between β1-adrenoceptor
antagonists and anesthetics on BIS. They raised the possibility that
esmolol administration may mask inadequate anesthesia.
Our purpose was therefore to determine whether
preventing hemodynamic responses with esmolol simultaneously ameliorates
arousal reactions as quantified by BIS monitoring during laryngoscope
and endotracheal intubation.
Materials and Methods
Materials Required
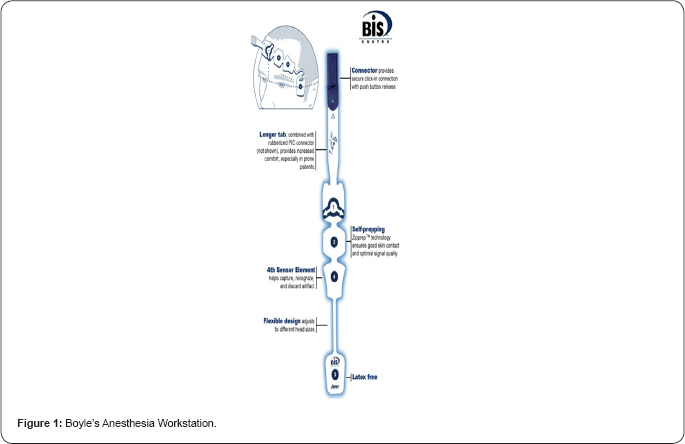
BIS System Components: The BIS system is comprised of five components
- BIS sensor-Capture raw EEG
- Patient interface cable (PIC)-Transmit raw EEG signal
- Digital signal converter (DSC)-Processes raw EEG and filter artefacts
- BIS engine-Analyzes EEG signal and calculate BIS index value
- Display monitor-Displays BIS index value and displays additional parameters including SQI, EMG, SR, EEG
BIS Sensor: The BIS sensor is a sophisticated
electrode system specifically designed to work with BIS systems. A
family of sensors tailored to different clinical applications or
different patient sizes are available. After minimal skin preparation,
the single-use sensor is placed on the forehead of the patient with a
specific orientation over either the left or right hemisphere. Due to
advanced electrode technology, it results in low impedance values,
allowing reliable capture of raw EEG data and increasing the fidelity of
the EEG signal. BIS systems routinely test sensor impedance to ensure
acceptable sensor performance during clinical monitoring.
Patient Interface Cable (PIC): The raw EEG is transmitted from the sensor through the patient interface cable to the digital signal converter.
Digital Signal Converter (DSC): The digital
signal converter receives, amplifies and digitizes the raw EEG signal
for subsequent processing and analysis. In addition, key filters and
signal processing steps occur in the DSC to identify and reject certain
types of electrical artefact (e.g., electrocautery filters in DSC-XP
systems). The digitized EEG data travels through the DSC cable to the
BIS engine.
BIS Engine: The BIS engine is heart of the BIS
system, contains the microprocessor, which is responsible for rapid
signal processing and computation of the BIS Index. Some of the steps
involved in the analysis of the EEG include multiple methods of artefact
detection and processing. Segments of the EEG that are compromised by
the presence of artefact are not included in the calculation of the BIS
Index. The BIS Index is made by combining selected EEG features, using
the BIS algorithm. All BIS values are updated every second but reflect a
smoothing function set at either 15 or 30 seconds to minimize excessive
fluctuations.
Display Monitor: All BIS systems are linked to
display monitors - either stand-alone BIS monitors or integrated
multiparameter monitors. These monitors have an ability to display BIS
value, BIS trends and important additional data including:
- Signal quality index (SQI)
- Electromyogram/High-frequency activity (EMG)
- Suppression ratio (SR)
- EEG waveforms
Signal quality index (SQI) and electromyogram/high-
frequency activity (EMG) may be displayed in graphic or digital mode.
Suppression ratio (SR) is also available. The display monitor also
coordinates a variety of communication alerts and alarms (Figure 1).
Boyle's Anesthesia Workstation.
- Bain's circuit / closed circuit with circle absorber
- Macintosh curved blade laryngoscope
Multi-para monitor having pulse oxymeter, NIBP, ECG and BIS
IV infusion set, blood transfusion set
IV Cannula: 18G; 20G, IV extension line
IV Fluids: crystalloids; colloids including normal saline
Disposable syringes: 5ml; 10ml; 50ml
- Infusion pump
- Suction machine, stethoscope, laryngoscope, ET tubes of different sizes, stop clock.
- BIS-QUATRO sensor
Drugs required
Anesthesia drugs
- Propofol
- Glycopyrolate
- Esmolol
- Atracurium
- Diclofenac sodium
- Ondensetron
- Neostigmine
Methodology
The study was conducted in the Department of
Anesthesiology, S.M.S Medical College and attached group of hospitals,
Jaipur with due permission from the institutional ethical committee and
review board and after taking written informed consent from the patient
Study design
Prospective Randomized Double blind Hospital based Interventionl study.
Sample size
Total 50 patients were selected and divided into 2 groups of 25 each via chit and box randomization technique.
Inclusion criteria/Exclusion criteria
Every patient was screened a day before surgery after applying inclusion and exclusion criteria
Inclusion criteria
o Patients with ASA grade 1 and 2
o Patients of age group 18 to 55 years of either sex undergoing elective surgery under general anesthesia
o Patients willing to give written and informed consent
Exclusion criteria
- Patients refusal
- Major organ dysfunction
- Patients on medications like hypnotics, narcotic analgesics, α2 agonists, calcium channel blockers, β blockers
- Patients with anticipated difficult intubation
- Patients incubated after more than 1 attempt or more than 20 seconds
- Patients with impaired LFT/RFT
- Patients with ASA grade 3,4,5
- Deaf and dumb patients
- Patients with respiratory, cardiac or neurological disease
- Patients having known allergy to anesthetic agents used in study
- Psychiatric patients
Groups
The patients were divided into two groups of 25 each according to drugs used
Randomization was done by chit and box method.
Pre-anesthetic check up
All patients were examined on the day before surgery
and explained about the anesthetic technique and peri-operative course.
Informed consent taken, each patient had a pre anesthetic checkup which
includes-
- Any significant present/past medical surgical history
- History of any previous surgery with significant anesthetic complication
- Physical examination
- Vital parameters like BP/Pulse/Respiratory rate
- Routine investigations like Hb, TLC, DLC, LFT, RFT, ECG,X-ray chest (PA view), FBS/RBS, Platelet count.
Technique
On arrival in the operation theatre, weight, fasting
status, consent and PAC was checked. Before anaesthetic induction,
electrodes for BIS (BISTM monitor 2000, Aspect Medical System, USA) were
placed on the forehead and the baseline BIS value was recorded. The
electrodes used were disposable BIS-QUATRO Sensor strips (Aspect Medical
System, USA). Baseline parameters [SpO2, Pulse rate (PR), Systolic
blood pressure (SBP), Diastolic blood pressure (DBP), baseline BIS were
recorded.
a) 2 IV lines with 18/20 G cannula were secured.
b) Ringer lactate drip started through one IV cannula
c) Premedication with Inj. Glycopyrolate (0.005 mg/kg) given 6 minutes before start of Induction of Anesthesia.
d) Inj Diclofenac 1.5 mg/kg infusion started after dilution in 100 ml saline.
e) Test drug Bolus: (Esmolol 1mg/kg or Normal saline)
was administered IV slowly over 1 minute in double blind fashion just
after premedication.
f) PR, SBP, DBP, SpO2, BIS were recorded after the test drug bolus.
g) Test Drug Infusion: (250μg/kg/min esmolol/normal saline) commenced in a double blind fashion after the test drug bolus.
Esmolol infusion prepared by taking 500mg of esmolol in 50ml syringe. The infusion rate adjusted as per the formula.
Rate (ml/min) = 0.25*body weight (kg)
The placebo group received normal saline infusion
over the same time period. The rate of infusion again calculated by the
same formula. The infusion rate was adjusted in infusion pump as per the
weight of the patient before starting the infusion.
The infusion continued for 14 minutes including the
time period for pharmacokinetic stabilization of drug levels in the
plasma (5min), the time taken for induction (3min) and intubation (1min)
and for 5 minutes after intubation.
PR, SBP, DBP, Spo2, BIS were recorded at
1st, 3rd and 5th minute after start of infusion. All the monitoring and
recording were made by yet another anesthesiologist who was blinded to
the groups. The patients were preoxygenated for 5min during this period.
Induction
Induction was done 5 minutes after start of test drug
infusion and with the ongoing infusion, using inj. propofol 2mg/kg
injected slowly over IV over 1 minute, and propofol infusion was started
at the rate of 6 mg/kg/hr after induction. After induction, pulse rate,
blood pressure, SpO2 and BIS was recorded. followed by inj.
Atracurium 0.5mg/kg . Hemodynamic parameters and BIS were recorded after
end of Propofol administration (6min from start of infusion). Patient
were ventilated with face mask with 100% oxygen for 2 minutes.
Hemodynamic measurements and BIS were recorded just before intubation (8
min from start of infusion).
Intubation
Intubation was done with endotracheal tube of
appropriate size after direct laryngoscopy. Tube position was confirmed
by ETCO2 and auscultation. Hemodynamic measurements and BIS were
recorded just after intubation (9 min from start of infusion) and 1, 3
and 5 min after intubation (10, 12, 14 min from start of infusion). The
test drug infusion was then stopped 5 min after intubation (14 min from
start of infusion).
Maintenance
Anesthesia was maintained with inj. Propofol infused
at the rate of 6mg/kg/hr and ventilation was done with 40% O2+ 60% N2O
by using Ventilator in Volume control mode with Vt at 8ml/kg and rate
adjusted to keep ETCO2 between 32-36. Muscle relaxation was maintained
with subsequent doses of atracurium (0.1mg/kg).
Intra operative monitoring
Intra operative monitoring continued and hemodynamic
measurements were recorded at 20min, 25min, 30min (from start of
infusion) and after every 10min thereafter. Inj. Ondensetron (0.1mg/kg)
was given intra operatively. Propofol infusion was stopped just after
the laproscope ports were taken out.
Reversal
Reversal was done with inj. Neostigmine (0.05mg/kg)
and inj. Glycopyrolate (0.01mg/kg). Hemodynamic measurements and BIS
were recorded after giving inj. Neostigmine and inj. Glycopyrolate
(Reversal was done after onset of spontaneous respiration).
Extubation
Extubation was done and hemodynamic parameters and
BIS were recorded immediately after extubation and 5min after
extubation. Any complication such as laryngospasm, bronchospasm or
desaturation was recorded and managed according to the standard
protocols. Any intra operative complication was recorded and managed
accordingly. Patients were shifted to recovery room and any immediate
post operative complication e.g. nausea, vomiting, shivering,
respiratory depression, sedation, restlessness, hypotention, bradycardia
etc. were recorded and managed.
Statistical analysis
Statistical analysis done after applying standard qualitative and quantitative tests (eg student-t-test and chi-square-test).
Review of Literature
Gibbs FA et al. [2]
illustrates that the electro-encephalograph records the essential
activity of the cortex of the brain, and the pattern of wave form is a
constitutional characteristic of the individual. Therefore,
abnormalities of rhythm may be of more fundamental significance than
clinical manifestations. The three main manifestations of epilepsy
(grand mal, petit mal and psychomotor epilepsy) are each accompanied by a
distinct pattern of dysrhythmia. The electro-encephalogram record
obtained in patients having psychomotor seizures is similar to that seen
in most patients diagnosed as having schizophrenia. These records,
furthermore, are closely similar to those obtained in the majority of
children with psychopathic personalities. On the basis of statistical,
therapeutic and electrical evidence, they believe that any relationship
between epilepsy and schizophrenia is positive rather than negative.
Sigl JC et al. [4]:
The goal of their study was to provide a simplified interpretation of
the electroencephalogram (EEG) for a variety of applications, including
the diagnosis of neurological disorders and the intra operative
monitoring of anaesthetic efficacy and cerebral ischemia. Power spectral
analysis, for example, quantifies only power distribution as a function
of frequency, ignoring phase information. It also makes the assumption
that the signal arises from a linear process, thereby ignoring potential
interaction between components of the signal that are manifested as
phase coupling, a common phenomenon in signals generated from nonlinear
sources such as the central nervous system. Bispectral analysis is a
method of signal processing that quantifies the degree of phase coupling
between the components of a signal.
Zaugg M, et al. [16]
found that peri operative betablockade improve long-term cardiac
outcome in non-cardiac surgical patients. A possible mechanism for the
reduced risk of peri operative myocardial infarction is the attenuation
of the excitotoxic effects of catecholamine surges by beta-blockade. It
was hypothesized that beta-blocker-induced alteration of the stress
response was responsible for the reported improvements in cardiovascular
outcome.
Mayer J, et al. [17]
showed the impact of Bispectral index (BlS)-guided general anesthesia
on recovery from general anesthesia in different patient population.
They designed this study to examine the value of BIS-guided anesthesia
in a fasttrack setting where the goal is rapid recovery. Forty-four
patients undergoing open colon resection were randomly assigned to
receive either BIS-guided (BIS group, n=22) or clinically guided
(standard care group, n=22) total IV anesthesia with propofol after
placing a thoracic epidural catheter. Duration of post anesthesia care
unit stay, time to tracheal extubation, direct drug cost, the incidence
of hemodynamic abnormalities, ability of ambulation on the day of
surgery, and patient satisfaction with anesthetic management were
assessed. They found that in the BIS-guided group, tracheal extubation
was achieved significantly earlier (7.6 vs. 15.4min, P<0.01) and the
post anesthesia care unit stay was significantly shorter (51 vs. 85min,
P<0.01). Total anesthetic drug cost was reduced by 23% and the
incidence of hypotension requiring treatment was significantly lower in
the BIS group. Early ambulation, patient satisfaction, and incidence of
adverse events were not significantly different between the groups. They
concluded that BIS-guided IV anesthesia in combination with thoracic
epidural analgesia facilitates rapid recovery and reduces the overall
cost of care in patients undergoing fast-track colon surgery.
Choi, Seung Ho [18]
studied that Activation of the peripheral nerve system by endotracheal
intubation is accompanied by an increase in bispectral index (BIS).
Esmolol produces a dose-dependent attenuation of the adrenergic response
to endotracheal intubation. In this double blind, randomized study,
after the induction of anesthesia, patients were mask-ventilated with
either sevoflurane or desflurane (end-tidal 1 minimum alveolar
concentration) and received normal saline or esmolol (0.5mg/kg) 1 minute
before intubation (sevoflurane-control, sevoflurane-esmolol,
desflurane-control, and desflurane- esmolol groups, n=20/group). BIS,
mean arterial pressure, and heart rate were measured before the
induction of anesthesia (awake), before esmolol injection (time point
1), immediately before intubation (time point 0), and every minute for 5
minutes after tracheal intubation (time point 1 to 5). Compared with
preintubation, esmolol attenuated the increase in BIS at 1 minute after
intubation during sevoflurane anesthesia (5.1% for esmolol and 31.7% for
control) but not during desflurane anesthesia (28.6% for esmolol and
30.8% for control). Mean arterial pressure and heart rate increased
after intubation in all groups but the changes were greater in the
control groups than the esmolol groups. In conclusion, a single dose of
esmolol blunted the increase in BIS to tracheal intubation during
sevoflurane but not desflurane anesthesia.
Zhong TD, et al. [19]
observed esmolol infusion as an adjunct to propofol can affect BIS
index, reduce anesthetic dose and decrease emergence time Sixty ASA I-II
patients, age 18-35, undergoing uterine dilatation and curettage
surgery were randomized into two groups. Before induction, patients in
esmolol group (Group E) were received 1 mg/kg esmolol intravenously and
followed by esmolol 150 microg x kg(-1) x min(-1) intravenous infusion;
patients in group C received normal saline instead of esmolol. Fentanyl
(1μg/kg) and propofol (2mg/kg) were used as induction drugs. The change
of BIS index, heart rate and MAP during operation; total amount of
propofol; time when patients opened eyes and time when patients reached
the standard for discharge from hospital were recorded. They observed
that BIS and heart rate of Group C at 1,2,3 minute after surgery
started, increased significantly compared with the time after induction
and those in Group E (P<0.05). The time patients reached the score of
discharging from hospital in Group C is longer than that in Group E
(P<0.05).
Esmolol combined with propofol administering in minor
ambulatory operations can control the increase of BIS index caused by
surgical nociceptive stimulus. Meanwhile the combination could reduce
the dose of sedatives and decrease anesthesia emergence time.
Observations
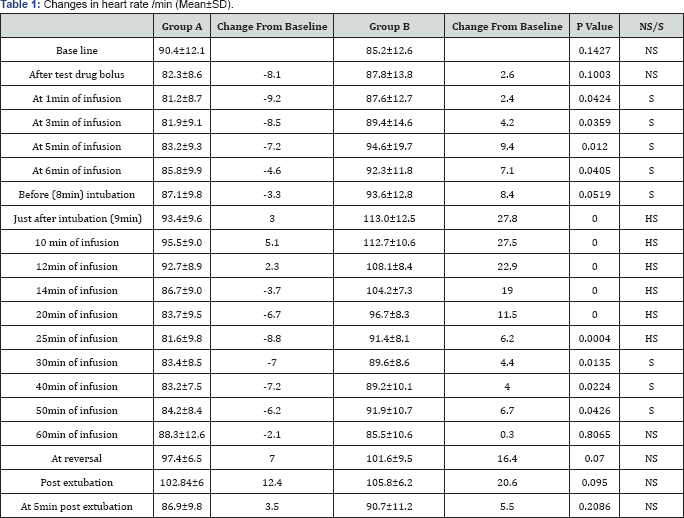
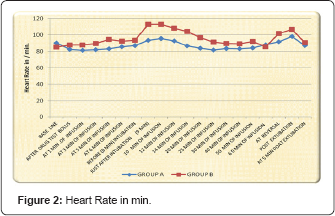
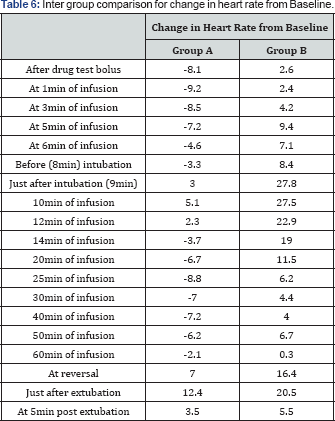
Table 1 shows the comparison of the two groups with regard to mean ± S.D. of Pulse Rate in both the groups at various time intervals.
Student's T- test (unpaired) was applied for
evaluation of changes in heart rate at different time intervals in each
group. Values at different time intervals were compared with baseline
value. There is no significant difference between the base line value of
the heart rate between the group A group B .In group A after test drug
bolus heart rate decreased from base line value 90.4±12.1 to 82.3±8.6
compared with group B in which heart rate increased from base line value
85.2±12.6 to 87.8±13.8. In group A, change compared to baseline value,
at 1, 3 and 5 minute after intubation, were +3.0, +5.1and 2.3
respectively, which was maximum change from base line after intubation.
At the same time in group B these changes were +27.8+27.5 and 22.9
respectively. On intergroup comparision of changes in heart rate from
base line at 1,3,5 minute after intubation statistically highly
significant difference was found (p value <0.000). At 14, 20, 25, 30,
40, 50min (from start of infusion) changes in heart rate from base line
was compared between group A and B a statistically significant
difference (p value<0.05) was found. At reversal and just after
extubation changes in heart rate from baseline in both group A and B was
compared and it was statistically not significant (p value >0.05) (Table 2) (Figure 2).
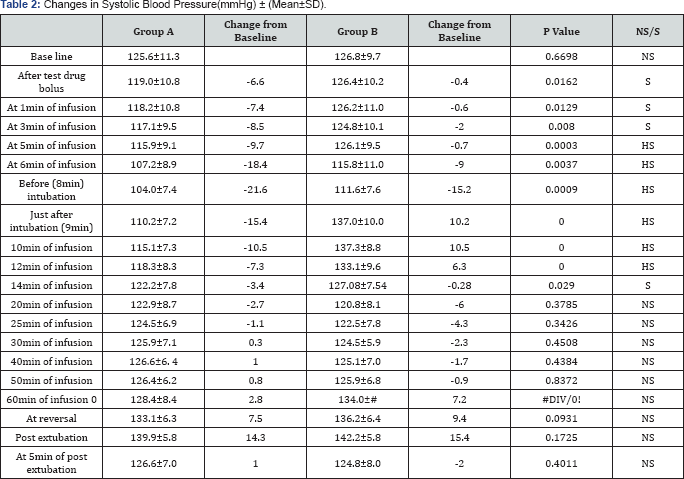
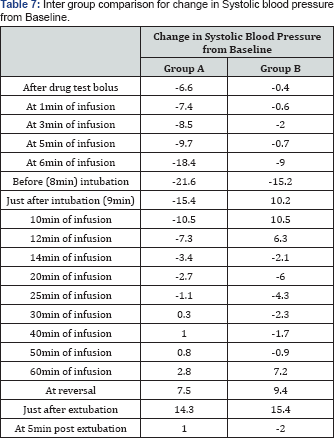
This table depicts the comparison of the two groups
with regard to mean ± S.D. of SBP (Systolic Blood Pressure) in both the
groups at various time intervals (Figure 3 & 4) (Table 3 & 4).

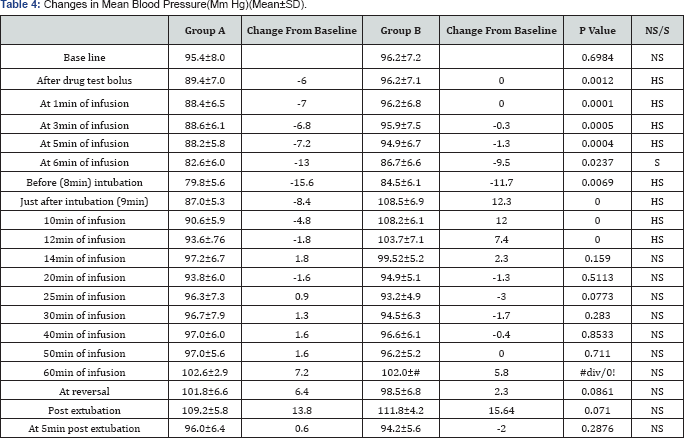
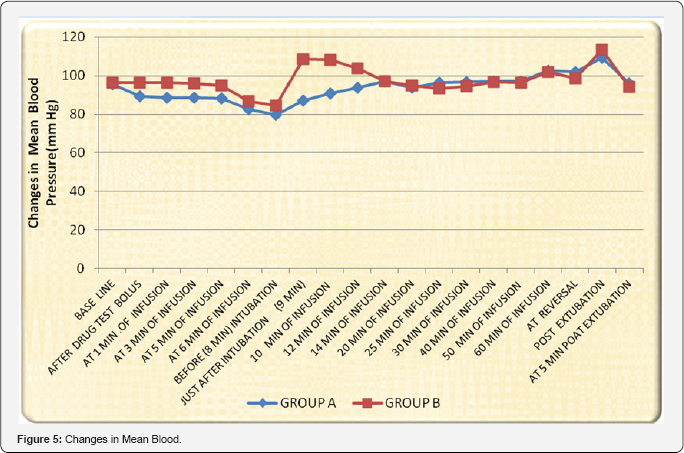
This Table shows the comparison of the two groups
with regard to mean change in mean blood pressure ± S.D. from baseline
value in both the groups at various time intervals. Student- t- test
(unpaired) was applied for evaluation of changes in mean blood pressure
at different time intervals in each group. There is no significant
difference between the base line values of the mean blood pressure
between group A group B (p value 698). Values at different time
intervals were compared with baseline value. After test drug bolus mean
arterial pressure decreases from base line in group A while in group B
it remained same.The change in Mean arterial pressure from base line at 1
,3, 5 6,and 8 min of infusion were compared and on intergroup
comparison statistically highly significant difference were found
between group A and B (p value<0.05).In group A change compared to
baseline value, at 1 ,3 and 5 minute after intubation, were -4.8,-1.8
and +1.8 respectively. At the same time in group B these changes were
+12.0,+7.4, +2.3 respectively. Changes in mean arterial pressure at
1,3and 5 minute of intubation were compared and statistically
significant difference was found in between group A and B (p value
<.05) (Figure 5 & 6) (Table 5).
Discussion
BIS index offers a direct and accurate method for
continuous brain status monitoring and provides a measurement of
hypnotic effect of anaesthetic agents. BIS monitoring is not a
substitute for clinical judgment. However, using BIS information as a
part of assessment we can make more informed decision about the dosing
and balance of anaesthetic agents.
Laryngoscopy as well as tracheal intubation is one of
the most stressful times in the period of anesthesia for the patient.
It is associated with significant changes in the hemodynamics i.e.
increase in heart rate and blood pressure as well as an arousal response
as quantified by BIS.
Various agents have been used to attenuate these
reflexes and reduce hemodynamic changes these include opoids, a2
agonists like clonidine, local anesthetics like lidocaine, adrenergic
blocking agents like esmolol and vasodilating agents like sodium
nitroprusside and nitroglycerine.
The hemodynamic responses to laryngoscopy and
tracheal intubation from reflex sympathetic discharge result from
epipharyngeal stimulation. It is logical to select an agent which would
prevent or minimize the laryngopharyngeal stimulation by the intubation
process or an agent which would block the sympathetic activity
associated with it.
Several studies have examined the BIS response during
laryngoscopy and endotracheal intubation to better understand the
relationship between cortical central nervous system and cardiovascular
response. With this background we conducted a prospective randomized
double blind study. Our purpose was to determine whether preventing
haemodynamic response with esmolol simultaneously ameliorates arousal
reaction as quantified by BIS monitoring during laryngosopy and
intubation.
Esmolol, a short-acting β1-adrenoceptor
antagonist, produces dose-dependent attenuation of the adrenergic
response to laryngoscopy and orotracheal intubation [20].
However, previous studies assessing the effectiveness of esmolol in
blunting the haemodynamic alterations induced by laryngoscopy and
orotracheal intubation failed to monitor electrical activity of the
brain. Only a few studies have evaluated the effect of interaction
between β1-adrenoceptor antagonists and anaesthetics on BIS. There was
no dropout recorded throughout the study. No adverse effects were
observed during or after the administration of study drugs.
Selection of patients
This study was carried out on 50 patients aged
between 18-55 yrs, of either sex belonging to ASA physical status I or
II, posted for a variety of surgical procedures. All the patients were
randomly divided into two groups of 25 patients each as below:-
Group A - Received Esmolol 1mg/kg bolus (10ml in volume) then 250μg/kg/min infusion for next 14 minute.
Group B - Received equal amount of saline (10ml in volume). Random sampling made the distribution of the patients in two groups.
To study effectiveness of esmolol in attenuation of
arousal response as quantified by Bispectral Index. These groups were
compared regarding the changes in and hemodynamic parameter to
endotracheal intubation. Any significant side effect of drug used.
Monitoring
Heart rate: The mean value of baseline heart
rate was almost similar in two groups (90.4±12.1 in group A and
85.2±12.6 in group B). Just after Test drug bolus the mean heart rate
decreased in group A but in contrast it showed an increase in group B.
This fall in pulse rate can be attributed to ßl- adrenoceptor blockade
effect of esmolol. After start of test drug infusion in group A mean
heart rate decreased as compared to baseline value. While in group B
heart rate showed an increase. At 1, 3 and 5 minute after intubation
heart rate increased in both group A and B but increase was
significantly greater in saline group (+27.8,+27.5,+19.9
respectively).While in group A 1, 3minute after intubation a rise +5.1,
+2.3 was observed. At 5 minute of intubation mean heart rate stabilized
and return below baseline value (86.7±9.0) in group A compared to group
B(104.2+7.3 and remained stabilized throughout the surgery. It means
that in group A esmolol is more effective for attenuation of
tachycardia. And throughout the procedure pulse rate in group A remained
below the base line value. It is evident in our study that in esmolol
group mean heart rate showed a less rise after intubation and it
stabilized early (3 minute after intubation) and remained stable
throughout the surgery because of attenuation of adrenergic response to
laryngoscoy and intubation by direct cardiac effect of esmolol as noted
by Menigaux C et al. [21]. In contrast to group B mean heart rate remained above base line value throughout the study.
Our results are comparable to Menigaux C et al. [21] who noticed similar trends in pulse rate after intubation. Our study also validates the findings of JIANG Yong,_et al. [22] who reported that a single dose of esmolol 1mg/Kg better attenuate heart rate than 0.5 mg/kg given before intubation.
There is a dose-dependent risk of hypotension and
bradycardia before laryngoscopy when esmolol is combined with anesthesia
induction agents [20].
However, the dose regimen used in our study did not result in any
adverse haemodynamic effects. Previous studies of Figueredo [20] and Miller DR, et al. [23] demonstrated decrease in heart rate before laryngosopy .This could be because of use of opioids. We did not use opioids (Table 6)
Systolic Blood pressure: The mean value of
baseline systolic blood pressure was almost similar in both groups
(125.6±11.3 in group A and 126.8±9.7 in group B). Just after
administration of study drug bolus systolic blood pressure decreased in A
group while in group B it remained almost same. But the changes were
statistically significant between group A and B (p value 0.01). In
Esmolol group at 1, 3 and 5 minute of intubation although mean systolic
blood pressure increased as compared to preintubation value but it was
still lower than baseline value(115.1±7.3, 118.3±8.3, 122.2±7.8
respectively). While in saline group at 1 and 3 minute after intubation
mean increase in systolic blood pressure was +10.5 and +6.3
respectively. Which was statistically greater (p value<0.005). At 5
minute of intubation systolic blood pressure stabilized and became
almost same as base line value. The rise in systolic blood pressure
after intubation was compared between the groups statistically highly
significant difference was found (P value<0.005). In our study was
effective in controlling pressure response to laryngoscopy as it is
evident from above observations .and inubation. Esmolol attenuates
hypertensive to intubation as it is evident from above observation.
These results are consistent with the findings of Menigaux C, et al. [21]
who observed a significant fall in systolic blood pressure at the same
time in their study. The hypotensive effect of esmolol results from a
gradual decrease in rennin release [24].
Similar trends were observed by JIANG Yong, et al. [22]
who reported that a single dose of esmolol 1mg/Kg better attenuate
systolic blood pressure than 0.5 mg/kg given before intubation. Shin H
Y, et al. [25] observed that there were significant differences in the mean arterial pressure between control group and other groups (Table 7).
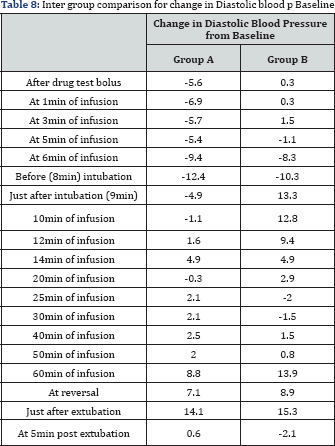
Diastolic blood pressure
As systolic blood pressure, there was no significant
difference in baseline value of mean diastolic blood pressure in both
groups (79.8±7.6 in group A and 80.9±9.2 in group B). Just after
administration of study drug bolus diastolic blood pressure decreased in
A group while in group B it increased from base line value. But the
change was statistically highly significant between group A and B (p
value 0.001). In group A at 1 minute of intubation mean diastolic blood
pressure (78.7±6.1) increased as compared to preintubation value but it
was still lower than baseline value. While in group B at 1 minute after
intubation mean increase in diastolic blood pressure was +12.8. In group
A at 3 and 5 minute of intubation mean diastolic blood pressure
increased as compared to preintubation value (81.4±8.0 and 84.7±8.4
respectively). While in group B at 3 and 5 minute after intubation mean
increase in diastolic blood pressure was +9.4 and +16.4 respectively was
observed. Just After intubation diastolic blood pressure increased in
both the groups but maximum increase was found in group B than group A.
Which was statistically significant (p value 0.000). From the above
observation it is evident that esmolol effectively attenuates
hypertensive response to laryngoscopy and intubation.
Similar trends were observed by Menigaux C, et al. [21] signifying the advantage of using esmolol in anesthetic regimen.
The observations are consistent with the findings of by Jiang Yong, et al. [22]
who reported that a single dose of esmolol 1mg/ Kg better attenuate
diastolic blood pressure than 0.5 mg/kg given before intubation. Shin,
et al. [25] also noted a significant fall in mean diastolic blood pressure compared to baseline values at all the measurement times (Table 8).
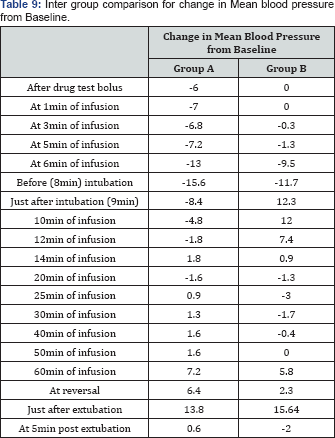
Mean blood pressure
Baseline value of mean blood pressure was similar in
both the groups (95.4±8.0 in group A and 96.2±7.2 in group B). Just
after administration of study drug bolus mean blood pressure decreased
in A group while in group B it remained almost same. But the changes was
statistically significant between group A and B (p value 0.001). Then
mean blood pressure was recorded till at 1,3,5,6 and 8 minutes of
infusion. In esmolol group it remained below base line value while in
group B mean blood pressure decreased after induction of anesthesia with
propofol (6 minute of infusion). The changes was statistically
significant between group A and B. At 1, 3 and 5 minute of intubation
mean blood pressure increased in B group from base line
value(.+12.0,+7.4.and +2.3 respectively) While in Esmolol group at 1 and
3 minute of intubation mean blood pressure decreased from base line
value(-4.8 and-1.8 respectively). The rise in mean blood pressure at 1
and 3 after intubation was compared between the groups statistically
highly significant difference was found (P value <0.000). These
results were similar to the results of Menigaux C, et al. [21].
The observations are consistent with the findings of by JIANG Yong, et al. [22]
who reported that a single dose of esmolol 1mg/ Kg better attenuate
hypertensive response to intubation than 0.5 mg/kg. Another study
conducted by PF White , et al. [26] use of esmolol alone in combination with nicardipine decreases mean arterial pressure in response to intubation (Table 9).
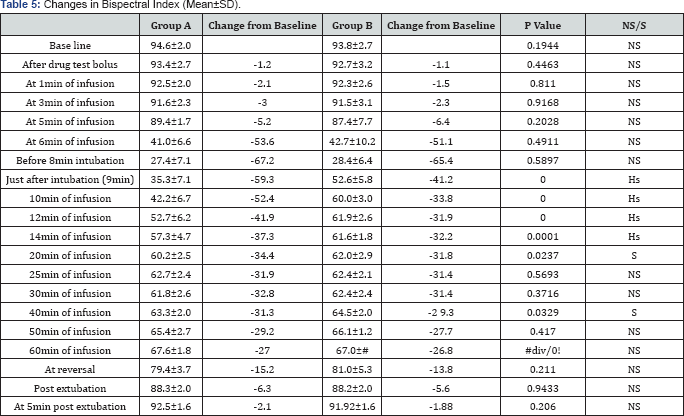
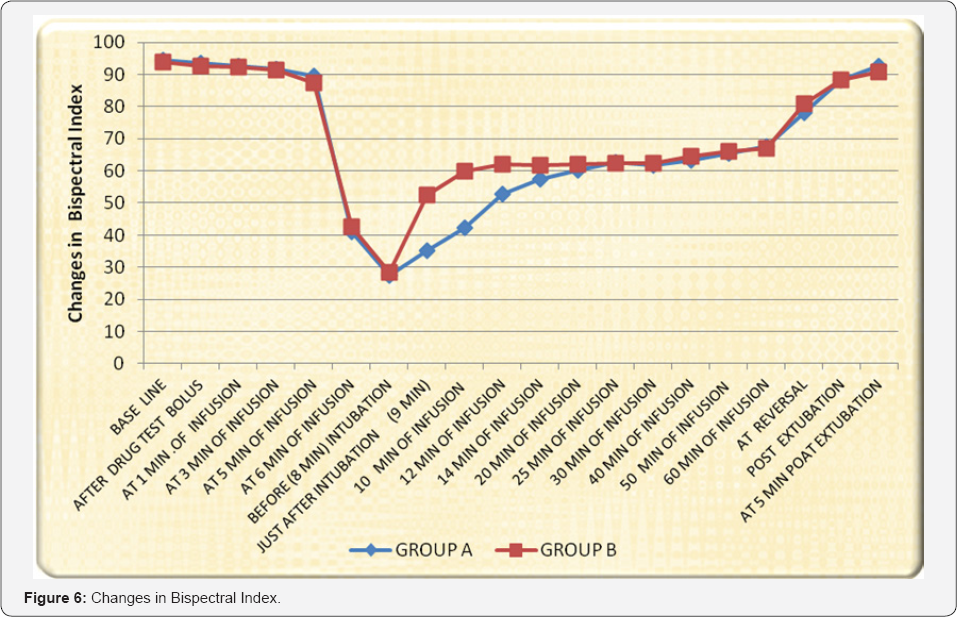
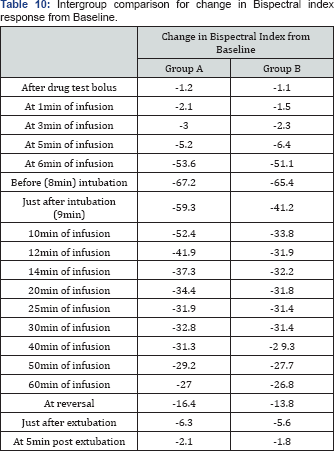
BIS value
Baseline value of Bispectral index value was almost
similar in both groups (94.6±2 in group A and 93.8±2.7 in group B).
After induction with propofol (2mg/kg) we started the propofol infusion
at dose of 6mg/kg/hr. After 5 minute of induction and start of infusion,
BIS value decreased up to range of 25-50 in our study.
The mean BIS value just before intubation was
27.4±7.1 and 28.4±6.4 in group A and group B respectively. The
difference between group A and B was statistically not significant.
Addition of esmolol to general anesthesia with propofol did not affect
BIS value before laryngoscopy. This observation suggests that esmolol
does not modify BIS during general anesthesia when substantial
sympathetic activation is unlikely. Just after intubation, there was
increase in BIS value in both esmolol & saline group but increase in
BIS value was greater in group B to (52.6±5.8) than group A (35.3±7.1)
On inter group comparison it was statistically highly significant (P
value 0.0001). At 1, 3 and 5 min after intubation BIS value increased as
compared to preintubation value in both groups. This rise was
significantly more in group B. These results indicate that esmolol does
not have anaesthetic effect per se and it mainly acts via beta
adrenergic blockade, thus it is effective only during period of
sympathetic activation as occours during laryngoscopy and intubation.
Our results are consistent with a study which reports that esmolol does
not alter the propofol blood concentration preventing response to
command. The noxious stimulation of layngosopy and inubation increases
central catecholamine concentration and esmolol prevents this response
by blocking β1 adrenoceptor within the reticular formation.
Our results and previous studies indicate that β1-
adrenoceptor antagonist not only block cardiovascular stress response
after noxious stimulation(laryngoscopy & intubation) but also
increase the anti-nociceptive component of anesthesia as reported by
Menigaux C, et al. [22]. In a study conducted by Johanson JW, et al. [27]
BIS value significantly suppressed in esmolol group compared to placebo
group using similar doses of esmolol . We found that at end of 9 minute
of intubation there was statistically significant difference in value
of BIS between both the groups.
The observations are consistent with the findings of by Oda Y manner, et al. [28]
using esmolol and landiolol. BIS was significantly greater in the
placebo group compared to esmolol and landiolol group. However, they use
sevoflurane for induction and maintenance instead of using propofol.
Autoradiographic studies in the rat hippocampus have reported both β1 and β2
adrenergic receptor expression in the rat hippocampus. Esmolol is a
moderate lipophilic drug with ( receptor activity and could be involved
in the modulation of central adrenergic activity, although some data
seem to dispute whether it crosses the blood-brain barrier [29].
Davidson et al. [30]
reported that β adrenergic blocking drug possess analgesic-like
properties and was able to attenuate the bispectral index responses to
noxious stimuli. However, our results are consistent with two other
studies, each of which demonstrated that esmolol can be used as
analternative to opioids for maintaining haemodynamic and BIS stability
during general anaesthesia. Dose of esmolol was selected in accordance
with previous reports in which concomitant use of esmolol with propofol
showed a significant reduction of the required dose for anesthesia and a
favorable inhibition of the BIS response to tracheal intubation [22,28]. The exact mechanism of this response requires further study.
Esmolol has been shown to control intraoperative
nociceptive responses during desfurane anesthesiain a similar way to a
compatirative group that received desfurane and an opioid in the
anaesthetic regimen obseved by Coloma, et al. [31].
In another study, patients β-blocked with atenolol required less
fentanyl and isofurane than unblocked control patients to produce
similar BIS values.
Another explanation may be an alteration of the
pharmacokinetics of propofol by esmolol. Our finding that BIS values
before laryngoscopy were similar in the two groups does not support this
theory. Esmolol by attenuating the haemodynamic responses to
laryngoscopy and orotracheal intubation may have prevented the increase
in cardiac output that would normally lead to redistribution of blood
flow with a resultant fall in the effect site concentration of propofol
and an increase in BIS [28].
It can be concluded bolus dose of Esmolol then
continuous infusion of esmolol provides better control of Bispectral
Index responses after orotracheal intubation than a single bolus dose of
esmolol [29]. However no side effect like bradycardia, hypotension and bronchospasm observed with esmolol in our study (Table 10).
Summary
After approval of hospital's ethical committee and
written informed consent from the patients and attendants, the present
study was undertaken in 50 ASA status I and II, of either sex between
the age group 18-55 years, scheduled for various surgeries in the
department of Anaesthesiology at S.M.S. Medical College & Attached
Group of hospital, Jaipur. All patients were thoroughly examined
pre-anesthetically based on the history, physical examination, chest
x-ray and other laboratory investigations.
All the patients were randomly divided into two groups of 25 patients each as follows:-
Group A- Received Esmolol 1mg/kg (10 ml in volume) then 250μg/kg /min infusion for next 14 minute.
Group B - Received equal amount of saline (10ml in volume).
Random sampling made the distribution of the patients in all groups. Baseline pulse rate, blood pressure, SpO2
and BIS was recorded. After loss of consciousness, positive pressure
ventilation using bag-valve-mask apparatus and 100% oxygen was
performed. Study drug was administered as previously mentioned.
Laryngoscopy and tracheal intubation was performed after induction and
administration of study drug. The pulse rate, blood pressure, SpO2 and BIS was recorded at various time interval.
- There were no significant difference found in demographic data in both the groups as patients were between 36.6 to 39.96 years of age and 55.3 to 58.8kg of Weight of both sexes.
- Baseline pulse rate was almost similar in both groups. But after intubation, a significant increase was found in group B that was greater than group A and it was statistically significant . Pulse rate remained near baseline in esmolol group than Saline group after intubation at different time intervals.
- Baseline systolic, diastolic and mean blood pressure were almost similar in both groups. Significant increase was found in group B that was significantly greater than group A. The increase in blood pressure at different intervals after intubation was found lower in Esmolol group than Saline group but it was statistically significant. It suggests that Esmolol has more protective effect than Saline against haemodynamic responses to orotracheal intubation.
- Propofol provides BIS value in range of 40-60, after induction and on continuous intravenous infusion at 6mg/ kg/hr.After intubation, there was significant increase found in BIS value in group B than group A and 6 min after stoppage of esmolol infusion there was a statistically significant difference in BIS value in group A and B. It proves that bolus dose of Esmolol then continuous infusion of esmolol provides better control of Bispectral Index responses after orotracheal intubation than a single bolus dose of esmolol.
- Propofol intravenous infusion provides better control of Bispectral Index responses after orotracheal intubation.
- No significant difference in SpO2 was found in all groups.
Conclusion
From the above study and other mentioned previous
studies, it can be concluded that Esmolol provides more protective
effect against bispectral index and haemodynamic responses after
orotracheal intubation.
Previous studies mentioned that when Esmolol was
given in a single bolus dose followed by continuous intravenous
infusion, it provides better control on Bispectral index responses after
orotracheal intubation but a single bolus dose alone was not found so
much effective.
Esmolol effectively blunts the hemodynamic response
as well as arousal reaction as quantified by BIS to endotracheal
intubation in patients undergoing surgical procedures under general
anesthesia and can be safely used at induction of general anesthesia.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment