Nt-Probnp versus Echocardiography in the Etiologic Diagnosis of Acute Severe Dyspnea-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Introduction: Acute dyspnea is a common
presenting complaint to the emergency department (ED). Etiologic
diagnosis is often difficult in the context of emergency. N terminal
probrain natriuretic peptide (Nt-proBNP) and echocardiography are
actually fundamental tools in the management of patients with heart
failure in the ED. The goal of this study was to compare the accuracy of
Nt-Pro BNP assay with Doppler echocardiography in differentiating CHF
from other causes in patients consulting the ED for severe dyspnea.
Results: A total of 65 patients were enrolled
in the study. The diagnosis of congestive heart failure (CHF) was
retained in 44 cases. The initial diagnosis was wrong in 15 patients
(23%): CHF was missed in 10 (15.38%) patients and wrongly diagnosed in 5
(7.69%) patients. The mean Nt-ProBNP concentration was 9188±6338 pg/mL
in the CHF group, compared with 416±400 pg/mL in the non-CHF group
(p<0.0001).Left ventricular EF was significantly lower in patients
with CHF (40.93±12.2 versus 55.29±7.8, p<0.0001). Systolic left
ventricular dysfunction (EF<0.45) was found in 29 (65.9%) patients
with CHF and in 4 (19%) patients with other causes of dyspnea
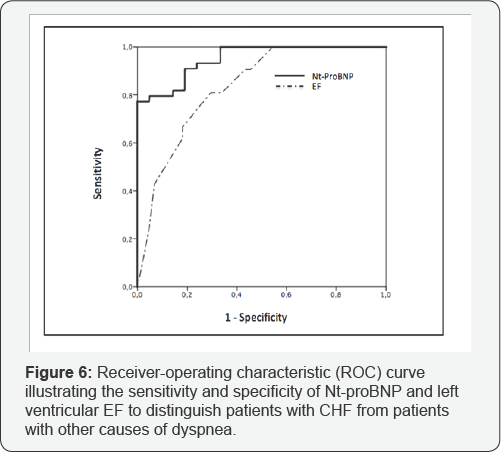
(p<0.0001). The area under the ROC curve was significantly higher for
Nt-ProBNP than for EF (0.95 versus 0.83, p<0.0001). The Nt-ProBNP
cutoff value of 500pg/mL had the highest sensitivity (97%) and negative
predictive value (93%) but a specificity of (66%). The cutoff value of
1100pg/mL had the highest specificity (93%) and accuracy (86%) but a
sensibility of (79%). Left ventricular EF had the lowest positive
predictive value (66%) and accuracy (70%).The best diagnostic
performance was found with the presence of ("impaired relaxation” and "
restrictive pattern”) with an accuracy of 92%.
Conclusion: The major contribution of the
Nt-ProBNP is the ability to rule out the diagnosis of CHF in the ED with
a cutoff of 500pg/mL, above this value, it is only a fair indicator of
the disease. Doppler echocardiography represent the « gold standard » in
the evaluation of patients with acute dyspnea by the ability to
evaluate diastolic and systolic function on one hand and to clarify the
etiological diagnosis on the other hand.
Keywords: Natriuretic peptides; Heart failure; Echocardiography Abbreviations: ANOVA: Analysis of Variance; Nt-ProBNP: N Terminal Probrain Natriuretic Peptide; CHF: Decompensated Congestive Left-Heart Failure; DT: Deceleration Time of the Mitral E-wave; ED: Emergency Department; LV: Left Ventricular; LVEF: Left Ventricular Ejection Fraction;OR: Odds Ratio; ROC: Receiver Operating Characteristic
Background
N terminal probrain natriuretic peptide (Nt-proBNP)
and echocardiography are actually fundamental tools in the management of
patients with heart failure in the ED. The goal of this study was to
compare the accuracy of Nt-Pro BNP assay with Doppler echocardiography
in differentiating CHF from other causes in patients consulting the ED
for severe dyspnea.
Introduction
Acute dyspnea is a common presenting complaint to the emergency department (ED) [1,2].
Often, it is caused by decompensated congestive left-heart failure
(CHF); which requires rapid diagnosis for prompt and appropriate
treatment.
However, this is often difficult in the context of emergency, especially
in elderly [3] or obese patients [4] or those with underlying chronic lung disease [5].
The symptoms may be nonspecific, and physical findings are not
sensitive enough to make the diagnosis which can have detrimental
effects for the patient with the corresponding risks for under- and
overtreatment [6-8].
N terminal probrain natriuretic peptide (Nt- proBNP) has been described
as an important biomarker able to assess diagnosis and severity of
heart failure (HF) as well as predict outcome and potentially guide
therapy even in the emergency setting [9]. It has been recommended in international guidelines for the diagnosis and management of HF [10].
The use of Nt-pro BNP at the rule-out threshold
recommended by The 2012 European Society of Cardiology guidelines on HF
provides excellent ability to exclude acute heart failure with high
specificity and sensitivity [11,12].
Despite the evidence that Nt-pro BNP is secreted in ventricular
overload states, there is an individual and inter-individual variation
(age, gender, race, obesity, renal function), which makes the
interpretation of Nt- pro BNP levels difficult [13].
So, a careful clinical examination associated with an echocardiography
examination should be complementary to Nt-pro BNP analysis for
diagnostic strategy and treatment implementation [14]. Echocardiography is a fundamental tool in the management of patients with heart failure [12].
Unfortunately, it is not routinely available in the ED. The role of
Echocardiography in emergency medicine as a diagnostic and a guide to
therapy tool is expanding rapidly, but its value for the etiologic
diagnosis of dyspnea has not been adequately studied in the emergency
setting [15].
The goal of this study was to compare the accuracy of Nt-Pro BNP assay
with Doppler echocardiography in differentiating CHF from other causes
in patients consulting the ED for severe dyspnea.
Patients and Methods
Study design
This was a prospective cohort study of a convenience
sample of patients presenting to the ED with acute dyspnea. The local
ethics committee approved this study.
Study setting and population
This prospective study was performed in the emergency
and intensive care department in the regional hospital of Zaghouan in
TUNISIA. The patients were recruited during 7 months, from June 2015 to
December 2015. All adult patients presenting to the ED for acute severe
dyspnea as their main symptomwere included. As exclusion criteria we
retained myocardial infarction, recent surgery, pneumothorax and chest
trauma. Patients were also excluded if they had received intravenous
(IV) therapy in the ED before echocardiography and NT-proBNP were
performed and also if emergency echocardiography was not feasible (poor
echogenicity, tachycardia, permanent pacing, or mitral prosthesis).
Study protocol
On admission, patients underwent a complete physical
examination, 12-lead electrocardiogram, chest X-ray, arterial blood gas
analysis, and routine blood tests. The senior physicians were asked to
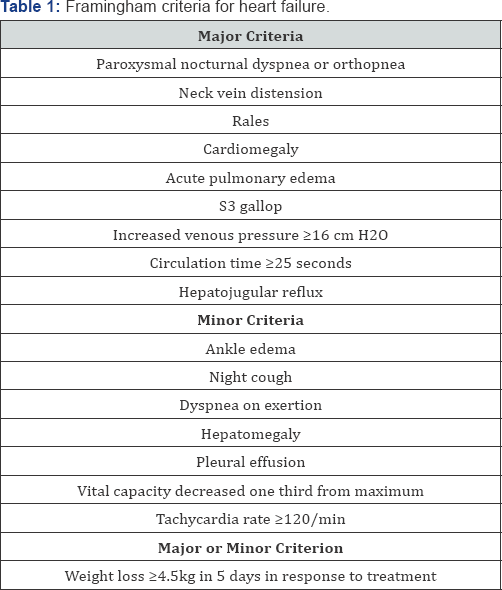
complete the Framingham criteria for heat failure [16].
The diagnosis of heart failure was retained at the presence of tow
major criteria or one major criterion plus to minor criteria Table 1.
Within 30 minutes of inclusion in the study and before initiation of
therapy, blood samples for NT-proBNP assay were collected and at the
same time echocardiography were performed. The treating physician was
blinded to NT-proBNP and echocardiography results.
Nt-ProBNP analysis: 5-mL blood sample was
immediately collected into a tube containing potassium ethylenediamine-
tetraacetic acid (1mg/ml blood), centrifuged and stored at 80 °C.
NT-proBNP analysis was per- formed with a commercially available
immunoassay (Elecsys pro-BNP, Roche Diagnostics, Indianapolis, IN) on an
Elecsys 1010 analyzer. The coefficient of variation for inter- and
intraassay precision was <4%.
Echocardiographic data: Doppler
echocardiograms were obtained at the bedside by cardiologists
experienced in echocardiography. The left ventricular ejection fraction
(LVEF) was estimated mainly by visual inspection. Diastolic indices
included: the early (E) and late (A) diastolic filling velocities, the
E/A ratio, and the early deceleration time (DT). Diastolic function was
initially classified as:
1. Impaired relaxation: When E/A ratio < 1 with DT > 220 ms, suggesting no increase in LV filling pressures;
2. Restrictive: when the E/A ratio > 2 or E/A
between 1 and 2 and DT< 150 ms, or DT < 150 ms alone in case of
atrial fibrillation, suggesting an increase in LV filling pressures;
3. Normal or pseudonormal: when E/A between 1 and 2 and DT > 150 ms;
Outcome measures
A medical staff including cardiologist, pneumologist
and intensivist, who were blinded to the results of Nt-ProBNP assay and
Doppler echocardiography obtained on admission, established the etiology
of dyspnea. They had access to ED records, clinical notes, and any
additional information that became available during hospital stay. The
Confirmation of CHF was based on the Framingham criteria, response to
treatments (diuretics, vasodilators, inotropic agents), hemodynamic
monitoring and pulmonary functional tests. Patients were finally
classified as CHF or non-CHF.
Statistical analysis
Categorical data are presented as numbers (percent),
and continuous data as means SD. The Students t test and the Fisher
exact test were used as indicated. Group comparisons of Nt-ProBNP values
were made using analysis of variance (ANOVA) with the Newman- Keuls
post hoc test; p values 0.05 were considered significant. The
sensitivity, specificity, accuracy, negative and positive predictive
values of Nt-ProBNP assay and Doppler echocardiography for CHF were
compared. We also computed receiver operating characteristic (ROC)
curves to determine optimal Nt-ProBNP cutoffs. We calculated the
diagnostic performance of the Framingham criteria, of Nt-proBNP, of the
LVEF and of the diastolic dysfunction. The analyses were performed using
SPSS 20 software.
Results
Characteristics of study patients
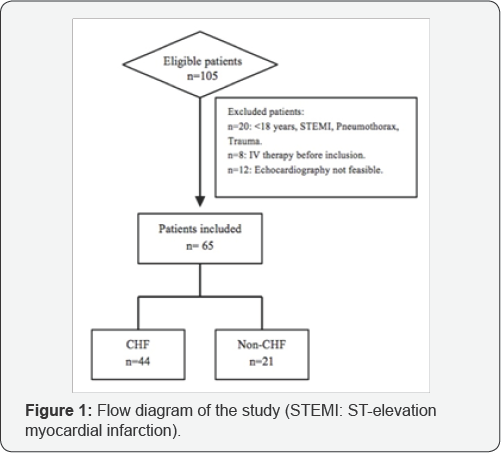
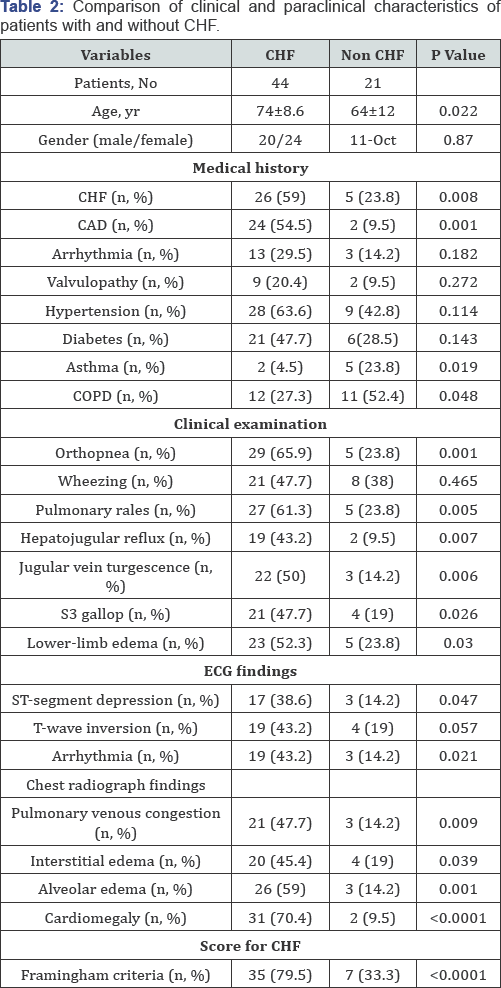
A total of 105 patients were eligible for the study, of whom 40 met exclusion criteria Figure 1. A total of 65 patients were enrolled in the study. The clinical and demographic characteristics of patients are presented in Table 2,
according to the final diagnosis. Among these patients, 39 (60%) had
severity signs and were admitted to the intensive care unit, mechanical
ventilation was indicated in 10% of these (n=4). Of the remaining 26, 20
(30%) were admitted to a general medical ward, and 6 (10%) were
observed in the ED. During hospitalization 6 patients (9%) died.
The mean time between the onset of acute dyspnea and
inclusion in the study was 6,2 ± 3,8 hours. The diagnosis of CHF was
retained in 44 cases. CHF was due to coronary artery disease (n=20),
hypertension (n=14), arrhythmia (n=8), and valve disease (n=2). Non-CHF,
21 cases, was due to pneumonia (n=9), decompensated chronic obstructive
pulmonary disease (n=8), severe asthma (n=3) or pulmonary embolism
(n=1). The patients with CHF were older than those with dyspnea from
other causes (74 years versus 64 years, p<0.05). They had more
history of cardiovascular diseases such as chronic heart failure
(p=0.008) and coronary artery diseases (CAD) (p=0.001). The patients
with no-CHF were more likely to have a history of respiratory diseases
such as asthma (p=0.019) and
COPD (p=0.048). On clinical examination, patients with CHF had more
symptoms (orthopnea), pulmonary rales, Hepatojugular reflux, jugular
vein turgescence, third heart sound and lower- limb edema. They also had
a higher incidence of abnormal ECG findings (ST-segment depression,
Arrhythmia), cardiomegaly and interstitial or alveolar edema. The
proportion of patients satisfying the Framingham criteria for CHF was
significantly higher in patients with CHF (79.5% versus 33.3%,
p<0.0001). The initial diagnosis was wrong in 15 patients (23%): CHF
was missed in 10 (15.38%) patients and wrongly diagnosed in 5(7.69%)
patients.
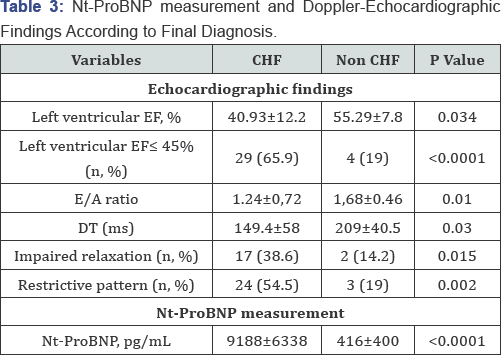
Nt-ProBNP and echocardiographic findings: The Nt-ProBNP measurement and Doppler-Echocardiographic findings were resumed on Table 3.
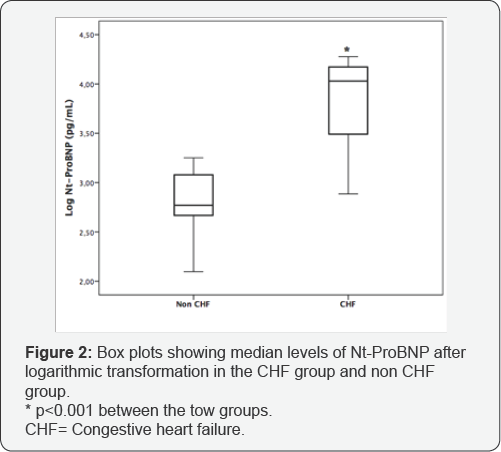
The mean Nt-ProBNP concentration was 9188±6338pg/mL in the CHF group,
compared with 416±400pg/mL in the non-CHF group (p<0.0001). Figure 2
shows box plots of log Nt-ProBNP values in each final diagnostic group.
Left ventricular EF was significantly lower in patients with CHF
(40.93±12.2 versus 55.29±7.8, p<0.0001). Systolic left ventricular
dysfunction (EF<0.45) was found in 29 (65.9%) patients with CHF and
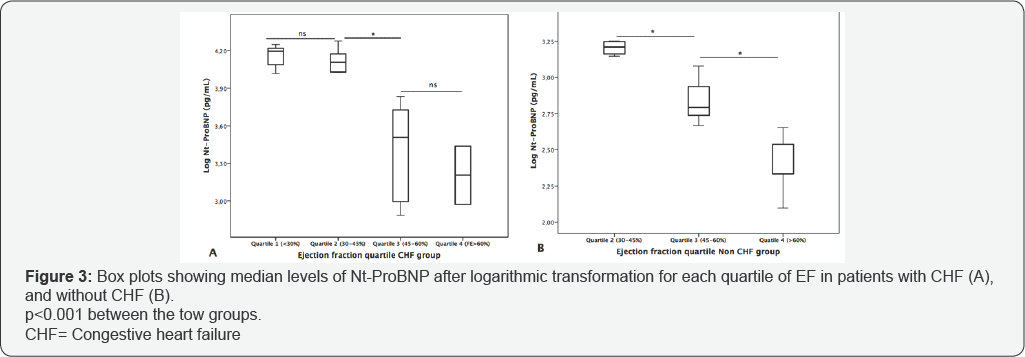
in 4 (19%) patients with other causes of dyspnea (p<0.0001). The log
Nt-ProBNP values for each quartile of EF are presented in Figure 3A for patients with CHF and in Figure 3B
for patients without CHF. Nt-ProBNP concentrations were significantly
higher in patients with abnormal systolic function in the two groups;
and they increased with the decrease in EF. The E/A ratio and DT were
significantly lower in patients with CHF, (1.24±0.72 versus 1,68±0.46,
p=0.001) and (149.4±58 versus 209±40.5, p=0.03) respectively. Diastolic
dysfunction was more pronounced in patients with CHF, "impaired
relaxation" and "restrictive pattern" was found respectively in 17
(38.6%) and 24 (54.5%) of the patients with CHF and in only 2 (14.2%)
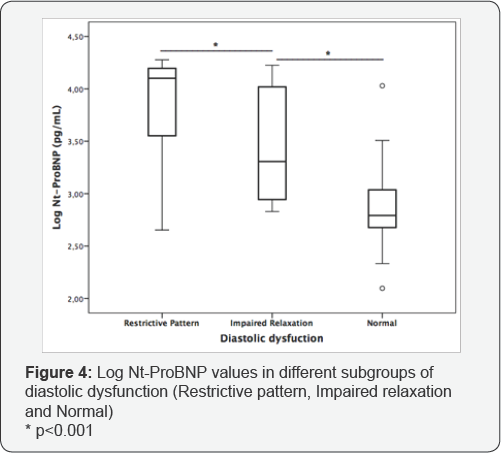
and 3 (19%) of the patients with other etiologic diagnoses. Patients
with abnormal diastolic function (n=18) had a concentration of
2250±1980pg/mL, whereas the normal subjects (n=16) had a mean Nt-ProBNP
concentration of 596±345pg/mL (p<0.0001). Figure 4
shows box plots of log Nt-ProBNP values in each subgroups of diastolic
dysfunction. Patients with "restrictive Pattern" had significantly
higher Nt-ProBNP levels than patients with "impaired relaxation"
(10323±6072pg/mL versus 5807±6140 pg/mL, p<0.001). The mean Nt-ProBNP
concentrations was significantly higher in patients with systolic
dysfunction than in those with diastolic dysfunction, and highest in
those with both systolic and diastolic dysfunction, as it shown in Figure 5.

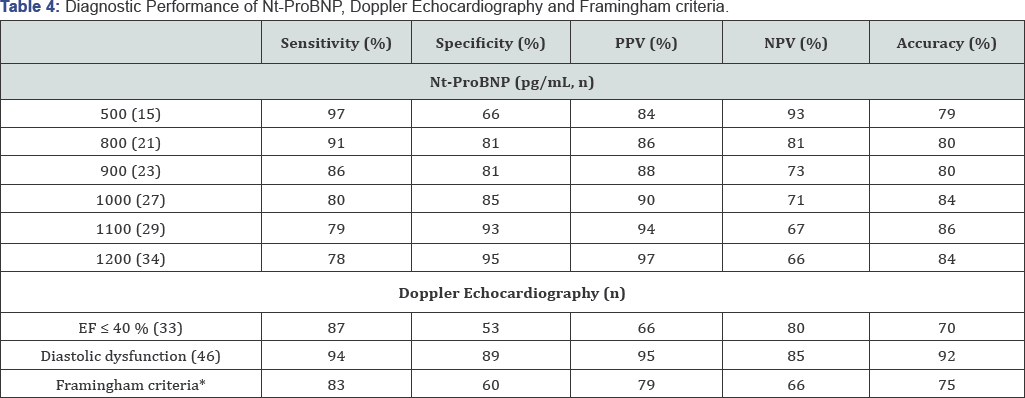
Etiologic diagnosis performance of nt-probnp and echocardiography:
Both, Nt-ProBNP and left ventricular EF were used to differentiate CHF
from other causes of dyspnea; the area under the ROC curve was
significantly higher for Nt- ProBNP than for EF (0.95 versus 0.83,
p<0.0001) Figure 6. The diagnosis performance of Nt-ProBNP, left ventricular EF, diastolic dysfunction and Framingham criteria was summarized in Table 4.
The Nt-ProBNP cutoff value of 500pg/mL had the highest sensitivity
(97%) and negative predictive value (93%) but a specificity of (66%).
The cutoff value of 1100 pg/mL had the highest specificity (93%) and
accuracy (86%) but a sensibility of (79%). Left ventricular EF had the
lowest positive predictive value (66%) and accuracy (70%). The best
diagnostic performance was found with the presence of ("impaired
relaxation" and "restrictive pattern") with an accuracy of 92%. Between
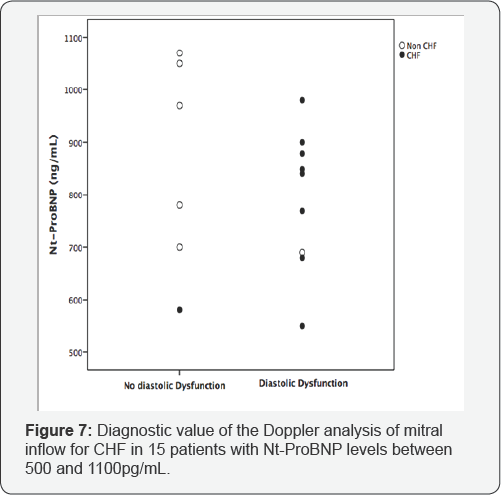
500 and 1100pg/mL, Nt-ProBNP had a poor predictive value of the final
diagnosis of CHF (OR 1.16, 95% CI [0.7 to 1.8], p=0.43). Fifteen (23%)
patients belonged to this interval, among them 10 patients were
misdiagnosed at admission. Nt-ProBNP cutoff values of 600, 800 and
1000pg/mL correctly identified 7, 5 and 2 patients respectively. The
presence of diastolic dysfunction on Doppler analysis of mitral inflow
correctly classified 13 of these patients and correct 8 of the 10
clinical misdiagnoses Figure 7.
Discussion
The etiologic diagnosis of acute dyspnea in the ED is
difficult because of the non-specificity of the symptoms and
non-sensitivity of physical, electrocardiogram and chest x-rays
findings, which constitute a source of misdiagnosis [2].
In our study, 23% of patients consulting for acute dyspnea were
misdiagnosed; this rate is close to that found in some studies [17,18].
According to the latest guidelines, natriuretic peptides and Doppler
Echocardiography are now considered to be part of the standard workup of
patients presenting with acute dyspnea to the ED [10,12].
Our results show that Nt ProBNP and Doppler Echocardiography have an
important contribution to the etiologic diagnosis of acute dyspnea in
the ED. Many studies have validated the high diagnostic accuracy of
Nt-ProBNP in the ED [19,20].
The 2012 European Society of Cardiology guidelines for heart failure
endorsed specific age independent decision cutoffs for plasma Nt-ProBNP
<300pg/mL, for the exclusion of acute heart failure based on
consensus of expert opinion [12].
The PRIDE (N-Terminal Pro- BNP Investigation of Dyspnea in the
Emergency Department) study demonstrated that Nt-ProBNP level ≤300pg/ml
was optimal for ruling out acute CHF [20]. Other studies demonstrated equal value of NT-proBNP [21].
In our study, we found that Nt-ProBNP cutoff of 500pg/mL had a high
negative predictive value (93%) with acceptable sensitivity and
specificity. This difference in cutoff values of Nt-ProBNP was mainly
due differences in study populations. A major part of our population had
a high mean age with comorbidities such us renal failure and was
admitted to the intensive care unit for severe dyspnea, in contrast to
the other studies [20,21].
In the other hand, a strong positive predictive value (94%), and a
highest accuracy (86%) were obtained with a cutoff of 1100pg/ mL. The
diagnostic value of the Nt-ProBNP was poor at values between 500 and
1100 pg/mL (23% of our patients). 40% of these patients had a final
diagnosis of Non-CHF due to severe pneumonia, decompensated chronic
obstructive pulmonary disease, or pulmonary embolism. Indeed, several
pathologies including infectious diseases, renal failure, critical
illness, cirrhosis of liver, intracranial pathologies, may be the cause
of high values of Nt-ProBNP even in the absence of depressed cardiac
function [22].
Secondly, our work has demonstrated the superiority
of Nt- ProBNP compared to the left ventricular ejection fraction (LVEF)
in the etiologic diagnosis of acute dyspnea. The calculated area under
the ROC curve was 0.95 for Nt-ProBNP, compared with 0.83 for LVEF. In
addition, LVEF had a poor positive predictive value (66%) and accuracy
(70%). Indeed, it is now accepted that a high proportion of patients
with CHF have normal left ventricular systolic function and this was the
case in 33% of our patients [23].
That is why we can no longer rely solely on the LVFE for the diagnosis
of CHF. Given that Nt-ProBNP is useful for the diagnosis of CHF both in
patients with and without systolic dysfunction [24,25].
Combining tow-dimensional imaging and Doppler, provides more data then
LVEF accurate in distinguishing between acute dyspnea due to CHF and
forms due to other causes. Tissue Doppler has recently become a gold
standard for diagnosing diastolic heart failure, but it requires
expertise, and it is not often used or applicable in an emergency
setting, especially in patients with dyspnea [24,26].
In our study, we are based on the measurement of the E/A ratio, and the
early deceleration time (DT) to evaluate diastolic function. They are
easy to have values in the emergency context and do not require
significant expertise. Several studies have shown a correlation between
the early (E) and late (A) diastolic filling velocities, the E/A ratio,
the early deceleration time (DT), mitral inflow pattern with left
ventricular end diastolic pressure, and pulmonary capillary wedge
pressure at rest [15,17].
Nazerian et al. demonstrated that emergency Doppler echocardiography,
particularly pulsed Doppler analysis of mitral inflow, is a rapid and
accurate diagnostic tool in the evaluation of patients with acute
dyspnea [15].
In our study, the presence of echocardiographic signs of diastolic
dysfunction (impaired relaxation, normal or normalized pattern and
restrictive pattern) showed a better sensitivity (94%), specificity
(89%), positive predictive value (95%), negative predictive value (85%)
and accuracy (92%) for the diagnosis of CHF compared with reduced LVEF
and Framingham criteria. In addition, the importance of echocardiography
findings is especially confirmed in the gray area of the Nt-ProBNP
values largely limiting its clinical usefulness [15,17,27].
In this study, the presence of diastolic dysfunction on Doppler
analysis of mitral inflow correctly classified 87% of patients belonging
to that area and corrects 80% of clinical misdiagnoses.
Thirdly, Our study has revealed that Nt-ProBNP
concentrations vary according to the type of heart failure. In fact,
several studies have shown that the mean Nt-ProBNP concentrations was
significantly higher in patients with systolic dysfunction than in those
with diastolic dysfunction, and highest in those with both systolic and
diastolic dysfunction [28,29].
On the other hand, we have shown that Nt-ProBNP concentrations were
different in subgroups of diastolic dysfunction but all subgroups had
higher Nt-ProBNP levels than patients with no-CHF. We can conclude that
Nt-ProBNP concentrations increase according to the stage of diastolic
dysfunction. In the first stage of diastolic dysfunction (impaired
relaxation), Nt-ProBNP levels mildly increase; in a second stage
(pseudonormalized filling pattern) these levels moderately increase; and
in an advanced stage of diastolic 11dysfunction (restrictive filling
pattern) Nt-ProBNP concentrations are markedly increased and our study
supports these findings [30,31]. Therefore, Nt-ProBNP measurements can play a crucial role in the diagnosis of diastolic dysfunction. Tschope, et al. [32]
concluded that Nt-proBNP reliably detects diastolic dysfunction in
patients with filling abnormalities and preserved LV systolic function.
The consensus statement on the diagnosis of heart failure with normal
left ventricular ejection fraction by the Heart Failure and
Echocardiography Associations of the European Society incorporated the
Nt-ProBNP in to the algorithm for the diagnosis of heart failure [26].
The optimal cutoff value for a diastolic dysfunction diagnosis is still
unclear and we need further investigation with echocardiography to
verify the diagnosis of abnormal cardiac function.
Conclusion
Nt ProBNP and Doppler Echocardiography have an
important contribution to the etiologic diagnosis of acute dyspnea in
the ED. In the present study, the major contribution of the Nt-ProBNP is
the ability to rule out the diagnosis of CHF in the ED with a cutoff of
500pg/mL, whereas above this value and especially in the gray area, it
is only a fair indicator of the disease. Thereby, Doppler
echocardiography represent the « gold standard » in the evaluation of
patients with acute dyspnea by the ability to evaluate diastolic and
systolic function on one hand and to clarify the etiological diagnosis
on the other hand. Certainly, Nt- ProBNP measurements can play a crucial
role in the diagnosis of diastolic dysfunction but its interpretation
should consider the echocardiography findings.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment