Remifentanil-Induced Respiratory Failure in PACU after a Brainstem Tumor Debulking: Acute Diagnostic Dilemma-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
A 66 year old man developed sudden apnea and
unresponsiveness after a large cerebellopontine angle tumor debulking.
Based on the findings of a focused neurologic exam, the patient was
emergently mask ventilated with subsequent return of spontaneous
ventilation minutes later and recovery without further complications.
Remifentanil bolus from residual infusion in an IV line was suspected
due to rapid return to baseline and acute neurologic findings. We review
remifentanil and highlight a challenging diagnostic dilemma in an
acutely apneic patient after major neurosurgery.
Keywords: Remifentanil; Neuroanesthesia; Post-op respiratory failure; Neurologic Emergencies Key Messages
a. A focused neurologic exam can affect emergent management.
b. A high index of suspicion and staff education are
necessary for those involved in the care of patients receiving
remifentanil.
Introduction
Remifentanil is a potent, ultra short-acting μ-opioid
receptor agonist with a rapid onset of action in 30-60 seconds, peak
analgesic and respiratory effects within 2.5 minutes (min), and rapid
clearance (T1/2 = 3 min) [1].
It is commonly used as part of a balanced anesthetic in many anesthesia
practices as well as in the intensive care unit. Its use is
particularly prominent in neuroanesthesia, where precise hemodynamic
control is as important as a crisp, quick emergence of anesthesia to
facilitate neurologic evaluation. Respiratory depression is a common
severe adverse effect of opioids that may be most prevalent with
remifentanil [2].
Case History
A 66 year old man with a large acoustic neuroma presented for cerebellopontine (CP) angle tumor resection (Figure 1).
Neuromonitoring of cranial nerves IX, X, XI, XII, somatosensory evoked
potentials and motor evoked potentials was used during the case, while
the patient received an intravenous anesthetic consisting of propofol
100mcg/kg/min and remifentanil at 0.3mcg/kg/min. Neuromuscular blockade
was not used for the case. The surgery progressed without complication,
and thepatient was stable throughout. The case lasted 7.5 hours, and
propofol and remifentanil were discontinued 60min and 15min prior to
conclusion of case, respectively. The patient was able to spontaneously
ventilate, protrude tongue, and demonstrate intact cranial nerves IX and
X with gag reflex prior to extubation.

In the PACU, the patient was awake and following
commands. Shortly after administration of flush through a secondary
peripheral IV, the patient acutely closed his eyes, becoming
unresponsive and apneic. Rapid physical exam to check for increased
intracranial pressure given the setting of recent intracranial surgery
demonstrated the patient's pupils were actually pinpoint. The patient
was then mask-ventilated until spontaneous ventilation returned several
minutes later. Pinpoint pupils and rapid recovery makes a remifentanil
bolus from residual infusion in the second IV line the most likely
etiology. Patient recovered without further difficulty and was
discharged home 3 days later.
Discussion
Remifentanil review
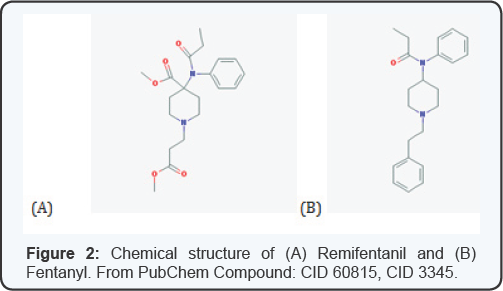
Remifentanil is a potent selective μ-opioid agonist.
Its major distinction from other fentanyl analogues is its rapid onset
and short duration of action with a terminal elimination half-life of
3-10 min, usually negating the need for Naloxone reversal [3].
The rapid onset of action is directly related to the rapid blood brain
equilibration time of 1-2 minutes, while the short duration of action is
a result of its unique structure of ester linkages making it
susceptible to hydrolysis by blood and non-specific esterases (Figure 2).
This rapid extra-hepatic metabolism makes its pharmacokinetics
reproducible and dependable. Time to spontaneous movement, following
commands, and extubation are all shorter than when compared with other
opioids such as fentanyl and morphine. These pharmacokinetic and
pharmacodynamic characteristics make remifentanil a nearly ideal
analgesic in the operating room. However, due to its short duration of
action, patients receiving remifentanil frequently require rescue
analgesia in the postoperative period for pain management [4].
Remifentanil is rapidly metabolized regardless of the
duration of infusion and is used commonly in clinical situations
requiring a rapid offset with the benefit of minimal side effects such
as respiratory depression [5].
While the risk for respiratory depression still exists, the ability to
rapidly titrate the drug based on response allows for an overall lower
rate when compared to most other opioids. In neuroanesthetic cases, it
is commonly used in conjunction with propofolas part of a total
intravenous anesthetic. It is easily titratable, facilitates stable
hemodynamics, and minimally affects neuro-monitoring. Perhaps most
importantly, this total intravenous anesthesia combination can allow for
rapid emergence and the ability to perform post-operative examination
for neurological status shortly after conclusion of the case [2].
Clinical experience
Rapid bolus of remifentanil can result in potentially
life threatening respiratory depression, hemodynamic changes, or muscle
rigidity. Respiratory depression has been documented in case reports
after bolus in laboring patients with patient controlled analgesia [6] as well as in non-obstetric patients receiving remifentanil [7].
This appears to be even more pronounced and observed at lower doses in
patients greater than 60 years old. Even infusions as low as
0.05mcg/kg/min have been reported to cause changes in ventilatory drive
in healthy volunteers. Muscle rigidity, likewise, is a concerning
complication of opioids that can lead to decreased ventilation and
compliance resulting in hypoxia and hypercapnia. It is suggested that
difficult ventilation may be primarily due to vocal cord closure.
Remifentanil, however, primarily affects respiratory drive by activating
opioid receptors on the respiratory neurons in the brainstem. By
depressing the respiratory drive, the arterial carbon dioxide not only
increases but increases in oxygen consumption and intracranial pressure
are to be expected [8]. Muscle rigidity however can be prevented with pretreatment or concurrent administration of neuromuscular blockade [9].
Apnea
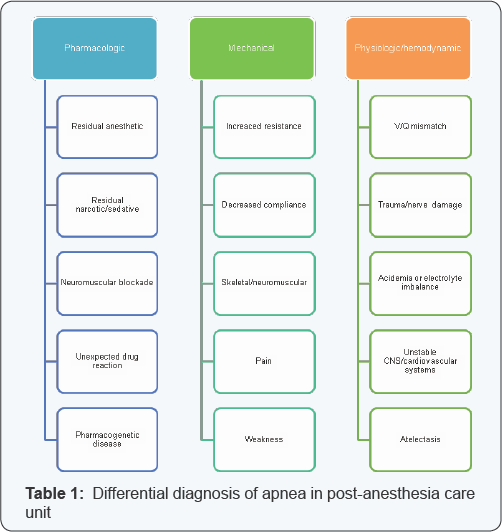
Our case brings up the challenge and importance of
differentiating causes of sudden apnea and mental status change in the
immediate post-operative period. The differential for postoperative
respiratory failure is large and includes pharmacologic, hemodynamic and
mechanical causes (Table 1).
In addition to those listed, the patient's comorbidities may be one of
the most fundamental things to consider. In the setting of recent
intracranial surgery, both opioid overdose and intracranial pathology
and dysfunction such as increasing intracranial pressure and seizures
are important considerations. Cerebellopontine angle procedures are
technically challenging and carry significant risk for postoperative
bleeding, increasing intracranial pressure, venous insufficiency and
cranial nerve palsy. Physical exam, including neurological exam, may be
the most useful and potentially life-saving in this case.
Prevention
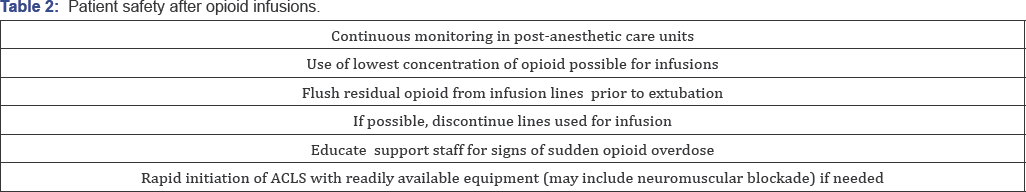
Prevention is a keystone of patient care, and the use
of more dilute concentrations of remifentanil and initiating rapid
resuscitation with possible muscle relaxation have been identified as
ways to decrease the chance of similar events from occurring (Table 2).
Remifentanil is a very useful opioid in a variety of settings for
controlling autonomic responses during procedures and allowing for rapid
recovery [2,5].
However, its dangers as a bolus should be known to healthcare providers
and ancillary staff so appropriate identification and supportive care
can be initiated as soon as a problem is identified.
Acknowledgement
Special thanks to Damian Pickering for assistance with
manuscript preparation.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment