A Rare Case of Varicella Pneumonia with Acute Coronary Syndrome and Lower Limb Arterial Thrombosis-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Unlike in children, where chickenpox is generally a
non-complicated disease, adult chickenpox (varicella) can have serious
complications. Thrombotic complications of the varicella zoster are
rarely observed. There is one case report of varicella complicated by
myocardial infarction.We present a case of adult varicella who developed
complications of peripheral artery thrombosis as well as acute coronary
syndrome, requiring angioplasty.
Introduction
Chickenpox (Varicella) is a benign illness caused by
VaricellaZoster virus and primarily manifests in childhood and is quite
infrequent in adults. Most complications and serious cases are observed
in adults [1].
These include pneumonia, encephalitis, cardiac arrhythmias, seizures,
rare neurological sequelae including optic neuritis and transverse
myelitis [2]. Thrombotic complications of the varicella zoster are rare [3,4].
A variety of hematological complications including thrombocytopenia,
purpurafulminans and disseminated intravascular coagulopathy have also
been reported in children with varicella [2-4].
Case Report
A 38 years old nonsmoker male was admitted with a
vesicular rash over the face, chest and abdomen since 3 days. There was
associated low grade fever (100 F) and dyspnea at rest. He had a blood
pressure of 120/60mm Hg, pulse at 118/min, respiratory rate of 32 and
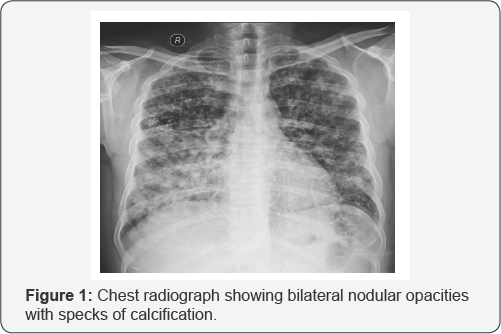
Saturation (SpO2) of 88% on 6 litres oxygen via face mask. His ABG revealed hypoxemia with a pH of 7.45, pO2 of 58.1 mmHg, pCO2 of 36mmHg. Chest radiograph revealed bilateral nodular opacities with specks of calcification (Figure 1).
His past and family history was unremarkable. His Complete blood count
revealed leucocytosis, kidney and liver function tests, Lipid and
thyroid profile were within normal limits.
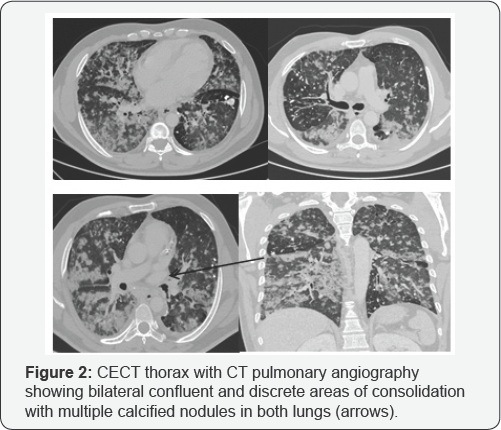
Contrast CT thorax with CT pulmonary angiography was suggestive of bilateral pneumonia (Figure 2).
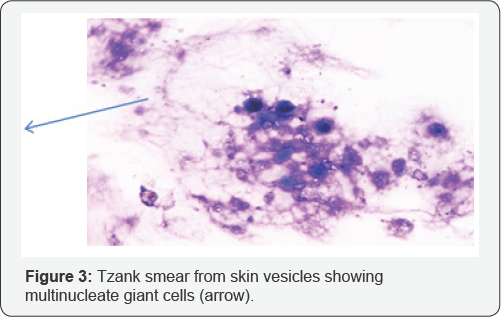
Patient was treated as varicella pneumonia and initiated on acyclovir
along with non-invasive ventilation and supportive intensive care. Tzank
smear from vesicles revealed multinucleate giant cells (Figure 3). Blood and urine cultures were sterile
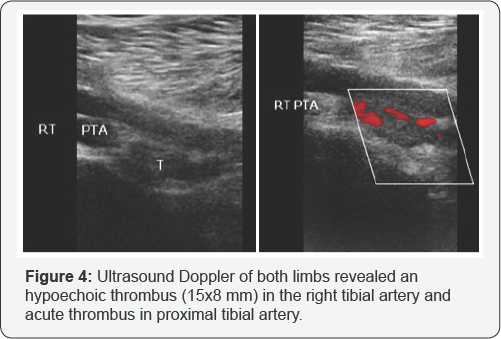
On the second day of hospitalization, patient's right
lower limb became pale with signs of ischemia. Ultrasound Doppler of
both limbs revealed a thrombus in right tibial artery and proximal
tibial artery (Figure 4). CT lower limb peripheral angiography confirmed intraluminal thrombosis in right tibio-peroneal trunk (Figure 5).
The same day our patient also developed acute left sided chest pain.
Electrocardiogram was consistent with ST elevation myocardial infarction
(STEMI) (Figure 6)
and cardiac biomarkers like Creatinine phosphokinase-MB, troponin I and
Pro BNP were elevated. 2D Echo showed regional wall motion abnormality
in anterior wall of left ventricle.

Patient was initiated on intravenous heparin infusion
with APTT monitoring. A coronary angiography was also performed which
revealed double vessel disease having long segment stenosis (90%) in mid
portion in Left anterior descending(LAD) and right coronary artery (70%
stenosis). Percutaneous transluminalangioplasty (PTCA) to LAD was done.
Thrombophilia profile (Protein C, S and Antithrombin III) and Lupus
anticoagulant antibody were within normal range. Vasculitis markers like
Anti-nuclear antibody (ANA), Antinuclear Cytoplasmic antibodies (cANCA,
pANCA) were negative. Gradually his limb perfusion improved and cardiac
status stabilized. A Review Transthoracic Echo-Doppler post PTCA done
on the 8th day showed no regional wall motion abnormality and normal
cardiac ejection fraction. Follow-up Doppler of Lower limbs showed no
evidence of thrombosis. The patient was stable and discharged after 10
days of hospitalization.
Discussion
Chickenpox is an extremely common illness, with about 90% of the population seropositive by the age of 15 [2]. It is uncommon, but more severe in adults with an increasing number of deaths being reported hospitals [5,6]. Pneumonia occurs only in about 6% of infected adults [7].
Our patient had associated pneumonia. Treatment options vary from
lotions plus antipyretic treatment or immunoglobulin and acyclovir for
serious manifestations. Acyclovir does not significantly reduce the
complications associated with the varicella zoster virus (VZV) infection
[8].
Thrombotic complication is a rare occurrence in VZV infection [8-11].
VZV is known to have tropism for vascular endothelium of cerebral
arteries. VZV is one of the commonest cause of ischemic stroke in
children, other complications being cerebral aneurysm and subarachnoid
hemorrhage. Unlike children, however, VZV in adults shows preference for
lower limb arteries. Our PubMed search for VZV and thrombotic
complications, showed only 5 reported cases of peripheral thrombosis,
all involving lower limb arteries. All the five cases were males, three
out of four being smokers with no past history of peripheral vascular
disease. Our patient was a nonsmoker with no previous history of
peripheral vascular disease. The origin of thrombotic complications of
VZV remains unknown. One study suggests that thrombosis was associated
with free protein S deficiency with the presence of anti phospholipid
antibodies [3,4]. The presence of lupus anticoagulant was also found in one of the case reports [3].
Another study suggested thrombosis was mediated by autoantibodies
induced by VZV infection and directed against the proteins involved in
the coagulation cascade [11].
Acute coronary syndrome (ACS) may also occur in
patients with varicella zoster virus infection after the primary
infection caused by varicella infection has been resolved [12].
Interestingly, our patient developed acute coronary thrombosis and
lower limb arterial thrombosis during varicella zoster virus infection
and not as a delayed complication. To the best of our knowledge, a
person developing ACS and lower limb arterial thrombosis during VZV
Pneumonia has not been reported before [8-12].
Conclusion
Chickenpox in adults, even in those who are
previously healthy, is a life-threatening infectious disease and may be
associated with acquired hypercoagulable state manifested by acute limb
ischemia, stroke or ACS depending upon the vessel involved. Clinicians
should be well aware of these serious complications for early
recognition and prompt therapeutic management. Above case is also
important with respect to timing of complications. Thrombotic
complications are usually delayed, but can occur in acute phase also.
For more articles in Academic Journal of
Pediatrics & Neonatology please click on:
https://juniperpublishers.com/ajpn/index.php
https://juniperpublishers.com/ajpn/index.php
Comments
Post a Comment