A Prospective Cohort Study Comparing Medical Student Intubation on Cadaveric and Manikin Models Using the King Vision™ Videolaryngoscope and Direct Laryngoscopy-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Objective: Compare intubation by
medical students with direct laryngoscopy (DL) versus King Vision™
videolaryngoscope in training and cadaveric models.
Methods: 24 medical students
with no experience intubating humans were randomized into two groups: DL
first or King Vision™ videolaryngoscope first. Following a short
training, techniques were practiced ona manikin model. Intubation
success, ease of use, and one timed manikin intubation was recorded.
Students crossed, repeated training and trial with other technique.
Students then intubated 3 cadavers with their initial technique, crossed
over to intubate these same cadavers using their second technique.
Cormack-Lehane (C-L) view of the glottic opening, time to intubation,
intubation success, ease of use, and preferred technique were recorded.
Results: In manikin intubation,
success rate was not significantly different. Mean time to intubation
using DL was 19.67 seconds, 11.03 seconds with King Vision™. The median
“ease of use” for DL was 7; King Vision™ was 4 (0 easiest, 10 hardest).
In cadaver model, the median C-L view was 2 for DL, 1 for King Vision™.
Success rates were 82% for DL and 93% for King Vision™. The median “ease
of use” for DL was 5 and King Vision™ was 4.
Conclusion: The King Vision™
videolaryngoscope had statistically significant improved visualization
of the glottic opening, intubation success rate when compared to DL, and
was rated easier to use. Given the portable nature, low cost, ease of
use, and easy maintenance; the King Vision™ videolaryngoscope should be
considered an excellent device for intubation training orany emergent
setting where advanced airway management is required.
Keywords:
Videolaryngoscope; Laryngoscopy; Airway management; Cadaver study;
Manikin study; King Vision; King Vision; Endotracheal intubation;
Medical studentIntroduction
Orotracheal intubation is a critical skill required
to manage patients with airway compromise or respiratory failure.
Traditionally, direct laryngoscopy (DL) has been the standard method
used to intubate patients. DL can be complicated by many factors that
obstruct direct visualization such as pathology to the oropharynx (e.g.
tumor) and limited mobility of the cervical spine [1-5].
Videolaryngoscopes (VL), which provide an indirect view of the glottis
and vocal cords, have been in use as an adjunct to DL for over a decade
[2,6,7]. Due to its ability to see “around the corner” via indirect
visualization of the glottic opening, VL has been recommended for
intubation in patients with limited neck mobility, airway anatomy that
is difficult to visualize, and for training novice intubators in
laryngoscopy [1,2,4-6,8-11]. The King Vision™ VL is a relatively new,
single unit, indirect videolaryngoscope that is lightweight, has a self
contained high-resolution camera, is battery operated, and has a curved
blade with the option of a tube-guiding channel for easier intubation.
Unique to the King Vision™ setting it apart from other VL is its low
cost and portability relative to all other VL.
Objective
The purpose of this investigation was to compare
timing and intubation success of the King Vision™ VL to DL in a manikin
and cadaveric model by medical students with no prior intubation
experience on human beings. Secondary outcomes were ease of use of DL
and the King Vision™ VL in both the manikin and
cadaver model as well as the Cormack-Lehane (C-L) view in
cadaver model only as this is the model that best simulates real
life intubating conditions.
Material and Methods
This study was approved by the Institutional Review Board
at the University of Texas Southwestern. This was a randomized
cross-over simulation study design in which 24 first year
medical students with fewer than 5 manikin intubations, not
previously employed in healthcare, and no prior intubation
experience on human beings were randomized into two groups.
Group 1 was initially trained in the use of DL followed by testing
their ability to intubate with DL on a manikin model. Group 2
was initially trained in the use of the King Vision™ VL followed
by testing their ability to intubate with this device on a manikin
model. Then, each group crossed over to intubate with the other
technique using the same training and testing as detailed below.
All training was performed using an adult Laerdal® airway
management trainer (www.laerdal.com).
All participants were recruited by campus wide email
and received no compensation for participation other than
intubation skills training. Exclusion criteria were extensive
intubation experience, defined as 5 or more previous lifetime
attempts, or any prior human intubation experience. After
written informed consent was obtained, each participating
student was required to review an 11-minute DL intubation
video, read a 4-page tutorial on basic endotracheal intubation,
and attend a 10-minute orientation on the King Vision™
VL. Group 1practiced DL intubation using a Macintosh 4
laryngoscope on a manikin model and Group 2 practiced VL
intubation using the King Vision™ VL with a channeled blade
until each student demonstrated 3 successful intubations and
felt comfortable with their assigned technique. Students then
had a timed intubation on the same manikin that they practiced
their assigned technique. The time to intubation and success
rate was recorded. The time period started once the tip of the
laryngoscope passed the lip of the manikin and ended once the
student verbalized that the intubation was complete. A research
assistant confirmed endotracheal tube placement in the manikin
via direct visualization. After completing a timed intubation on
their assigned technique, each student completed a written
survey to assess their perceived ease of use for that intubation
technique using a 0-10 scale with 10 being “very difficult” and
0 being “easy.”The students then crossed over techniques and
repeated the intubation training, testing and survey.
Students were then assigned to 3 of 6 cadavers, each
intubating all 3 assigned cadavers with the first technique,
then crossing over to intubate these same 3 cadavers using the
other technique. Students were asked to assess the C-L view of
the cadaveric glottic opening for each timed intubation with
each technique. As described in 1984 by Drs. Cormack and Lehane, the C-L view was graded as follows: 1) Grade 1, most
of the glottis is visible, 2) Grade 2, only the posterior extremity
of the glottis is visible, 3) Grade 3, no part of the glottis (only
the epiglottisis visible), and 4) Grade 4, not even the epiglottis
can be exposed [12]. The following information was recorded
for the cadaver intubations: time to intubation as described
above with the manikins, C-L view of the glottic opening, and
proper endotracheal tube (ETT) placement. ETT placement was
confirmed by direct observation of the ETT in the trachea through
a window created in the cricothyroid membrane by investigators,
who were blinded to the study group of the participant during
the intubation procedure. The C-L view was verbalized to the
research assistant present at the time of each intubation. After
completing intubation on the assigned cadavers, each student
completed a written survey to assess their perceived ease of
use of each intubation techniqueas mentioned above with the
manikins. Study was limited to 24 participants due to time,
availability, and materials constraints.
Results
A total of 24 first-year medical students (10 (42%) male, 14
(58%) female) were consented to participate in the study. The
King Vision™ VL is abbreviated as VL in the results section for
the purpose of simplicity.
Manikin data
There were 48 measured intubations performed by the
students on manikins, 24 DL and 24 VL. The intubation success
rate was 92% (n = 22) for DL and 96% (n = 23) for VL, p-value
= 0.50 with Fisher’s exact test. The mean time to intubation was
19.67 seconds using the DL and 11.03 seconds using VL, p-value
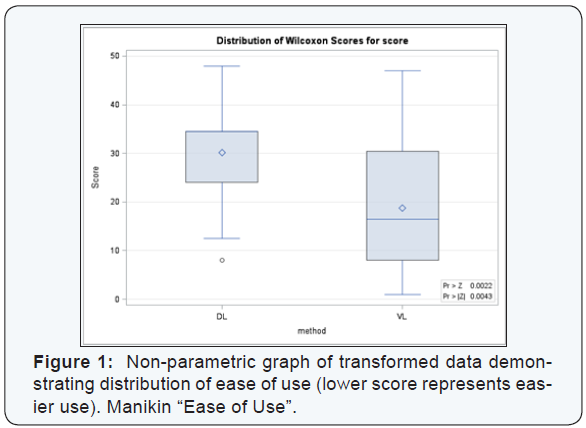
= 0.015 with Student’s t-test, Table 1. Utilizing Wilcoxon Rank
Sum test, the median ranking for “ease of use” was 7 for DL and
4 for VL on a 0 to 10 scale with 0 being the easiest to use and 10
being the most difficult, p-value = 0.003, indicating that students
thought the VL was easier to use, Figure 1 which has transformed
the 0 to 10 scale into a larger scale on the vertical axis to better
demonstrate the distribution of the data.
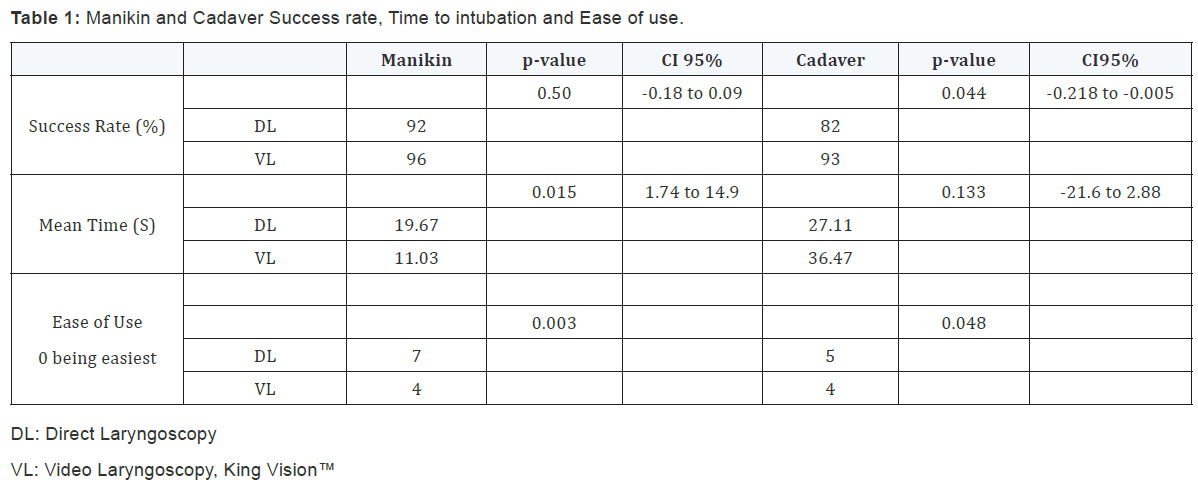
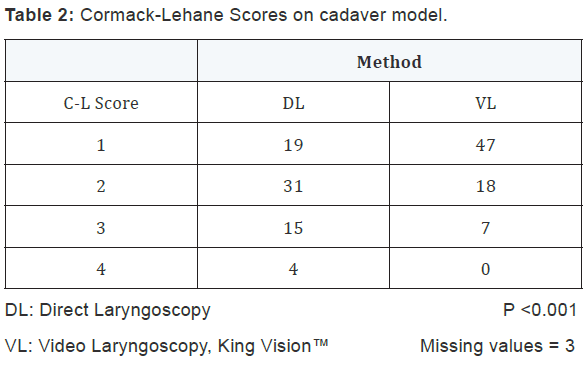
Cadaver data
There were 144 cadaveric intubation attempts (all 24
students intubated 3 different cadavers with each technique):
72 DL and 72 VL. The median C-L view grade was 2 for DL and
1 for VL, p-value < 0.001.Generalized Estimating Equations
were utilized for our ordinal values of the C-L grade, Table 2.
Eighteen of the intubation attempts were unsuccessful: 13 DL
and 5 VL. Success rates were 82% (59/72) for DL and 93%
(67/72) for VL, p–value = 0.044, Table 1. Generalized Estimating
Equations were used as successful intubation was a binomial
variable and confirmed that success rates were statistically
higher with the VL method. No statistical difference was seen
in the time to intubation for the method (DL vs. VL), Table 1.
Repeated Measures Analysis of Variance was used to determine
if the time to intubation varied between the DL and VL methods
of intubation for all participants. The intubation technique that
was used first by the student made no significant difference in
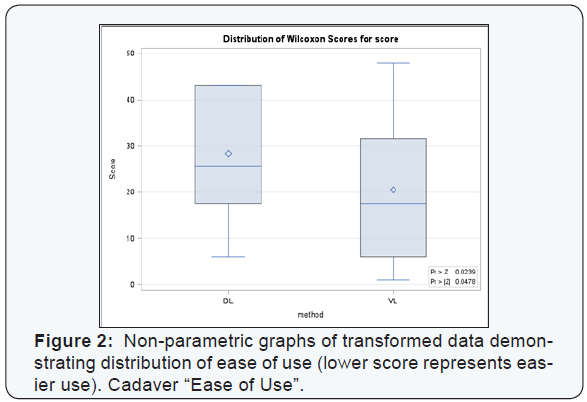
time to intubation or success. “Ease of use” for the cadaver model
utilizing the Wilcoxon Rank Sum test demonstrated that the VL
was also easier to use in the cadaver, p=0.048 Table 2 & Figure
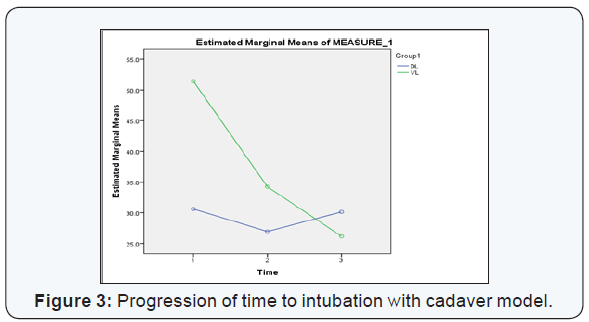
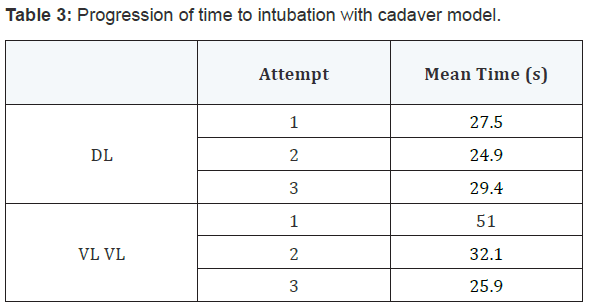
2. There was a positive trend in mean time from the first to third
intubation with VL from 51.0s to 25.9 s. DL had no improvement
with repeat intubation Table 3 & Figure 3.
Discussion
The results of the current investigation clearly demonstrate
that the King Vision™ VL has advantages compared to DL,
consistent with other VL performance in the current literature.
The King Vision™ was considered easier to use by participants,
had a higher success rate and better C-L scores. However, when
compared to other videolaryngoscopes, the King Vision™ VL is
less expensive, utilizes disposable blades, and is very portable.
The increased first pass success and C-L grade observed with
King Vision™ VL in this study are consistent with a 2014 study by
Murphy et al. using novice paramedic students in a cadaver model.
In this study, the King Vision™ VL had a higher success rate over
DL, faster time to intubation, and better C-L grades [10]. Although
our study showed insignificantly faster intubation times with DL
in the cadaver model, the time to intubate decreased by almost
50 percent with successive attempts using the King Vision™ VL,
indicating a rapid learning curve with the use of this device. In
the current investigation, both glottic opening visualization and
intubation success rates were significantly improved with the
King Vision™ VL using the cadaveric model. Two meta-analyses of
VL (GlideScope, X-Lite, Storz, McGrath, and Pentax-AWS) versus
DL found equivocal results in success rate, but a significantly
better view in difficult airways for VL. This is consistent with a
study by Murphy comparing King Vision™ to DL [6,10,11]. One
frequent finding is that increased visualization of the glottic
opening using VL may not proportionally translate to improved
success or faster intubation times [2,6,11,13,14]. DL failures are
typically due to inability to visualize glottic opening [14]. Most
failures with VL are not from poor visualization but instead, are
due to the inability to pass the ETT into the trachea [14-16]. This
is often due to incongruence between the location of the glottic
opening on VL and the trajectory of the ETT and is likely due to
advancing the VL blade too distally, positioning of the rigid stylet
used in the King Vision™ VL, or a very anteriorly placed glottis.
Subtle maneuvers, equipment modifications and practice can
reduce difficulties in passing the ETT. A Japanese meta-analysis
showed significant improvement in success and time to success
in VL (Airtraq and Pentax-AWS) with a channeled blade vs. DL
[9], facilitating placement of the tip of the endotracheal tube
much more anteriorly. The current investigation used a model
of the King Vision™ VL with the channeled blade. Although we
demonstrate a low failure rate consistent with most studies of
King Vision VL, the most common reason observed for a King
Vision™ VL intubation failure is poor technique, which can be
remedied using adequate training and briefly retraining if the
device is rarely used [17].
The King Vision™ VL may used as a teaching tool for
novice intubators similar to other VL, and has advantages over them for
training purposes due to its portable nature. Use of VL to train
novice intubators has shown higher success rates using DL for
endotracheal intubation in patients with normal airways as
compared to training utilizing DL [5]. The shortcomings of DL
for emergent intubators include significant training and practice
to become competent with the direct laryngoscope and poor
first-attempt tracheal intubation success rates [10]. The rapid
progression in time to intubation with the King Vision™ VL seen
in this data set is consistent with a study by Ayoub et al. which
demonstrated a more rapid acclimatization to VL with a drastic
decrease in time to intubation over 3 successive attempts when
compared to DL on surgical patients undergoing anesthesia
[5]. Several studies have demonstrated the ease of use of many
videolaryngoscopes with a shorter learning curve as compared
to DL [5,13]. In addition, any level user can easily gain skills in VL
because glottic visualization is not diminished to the same degree,
nor by the same factors that limit DL [4,18]. This is especially
pronounced in the difficult airway setting with VL success of
76.4% compared to DL of 8.8% in one study [4]. In addition to
steep learning curve and worse success with difficult airways,
another pitfall of DL is the deterioration of skills if not frequently
practiced. Murphy elaborates, ‘even in larger institutions and systems,
the opportunities to maintain intubation skill is limited,
with a significant proportion of practitioners having one or no
intubations per year’ [10]. Having a device that is easy to use and
portable makes continuing training easier to access and allows
the retention of intubation skills even in a setting of infrequent
intubation opportunities. Furthermore, it has been shown
that training on manikins is an adequate strategy if events to
train are rare or unpredictable [13]. Use of VL accelerates skill
acquisition, can be used as the primary training technique, and
can be used to retrain on manikins for infrequent practitioners
with sufficient quality in training.
The King Vision™ VL has several clinical advantages over
many other VL currently on the market in addition to ease of use
and portability. Two case reports discuss the King Vision™ VL
and its use clinically. One describes the success of King Vision™
VL for a difficult awake intubation of a patient with restricted
mouth opening in a remote area with limited resources [19]. The
King Vision™ VL was the only VL on the market that could have
successfully intubated this person as no other VL has as narrow
of a blade [19]. VL are also known for being easier to use than
fiberoptic intubating scopes in most patients as the approach to
intubating with VL is more similar to DL, the traditional method
used for intubating. The second case series used the King
Vision™ VL in awake intubations in patients with pathologic
abnormalities in airway anatomy making normal visualization
with standard DL impossible [17]. King Vision VL can be used
in the pre hospital environment. Studies with paramedics in a
simulated environment have shown King Vision™ VL is at least as good as and may be situationally more effective than DL under
unusual circumstances such as, entrapped patients with both
normal and difficult airways [10,20,21]. Other potential uses and
future studies include unexpected in-hospital code situations
on ward beds, international travel emergencies, public arenas,
disaster scenarios, and pre-hospital intubation.
There were several limitations to the current investigation.
The most obvious limitations were the small sample size and
the simulated environment in which this study was conducted.
In order to observe repeated measures data, ideally a repeat
study will be performed with sample size of significant power to
test the effects of different cadavers, the order in which the two
methods were applied, and all interactions to better determine
the factors that impact successful intubation. With the current
preliminary study, we do not have the sample size needed to
handle these more vigorous repeat measures analyses. We
believe with a more concrete selection process, we will likely
be able to confirm that, for most beginners, intubation using
the King Vision™ VL method will consistently demonstrate
improved C-L views, success rates, and time to intubation. The
King Vision™ VL is a relatively new device and as of the writing of
this article, a PubMed review did not identify any hospital based
clinical trials completed, although a large Swiss multicenter trial
protocol is written and currently ongoing with an objective of
comparing 6 VL, 3 channeled blades (King Vision™, Airtraq™, A.
P. Advance™)and 3 unchanneled blades (C-MAC™, GlideScope™,
McGrath™) in surgical intubation and an expected completion
date of August 2015 [22].
Conclusion
The King Vision™ VL not only improves visualization of the
glottic opening and intubation success rate, but it is easy to
use. Although intubation times were insignificantly longer with
the King Vision™ VL, cadavers were still successfully intubated
rapidly and students demonstrated drastic improvement with
successive intubations. Given the greater success rate of the King
Vision™ VL, the utility in intubating patients with a more difficult
airway most likely parallels other videolaryngoscopes. It is a
useful tool for training students and maintenance of intubating
skills. Considering the portable nature, low cost, ease of use, and
easy maintenance; the King Vision™ VL should be considered
to be an excellent videolaryngoscopic device in any emergent
setting where advanced airway management is required.
Acknowledgements
Ngosi, in memoriam.
Support
King Vision™ provided videolaryngoscopes and training
technicians for this study. All materials returned promptly at
end of study.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment