Incidence and Prevalence of Anxiety, Depression, and Post-Traumatic Stress Disorder Among Critical Care Patients, Families, and Practitioners-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
OBackground: WAnxiety,
depression, and post-traumatic stress disorder (PTSD) are common
complications of critical illness. Their prevalence is known to be
higher among patients than among the general population. Little is known
about their prevalence among families and among critical care staff.
Setting: Igeneral systems intensive care unit in a tertiary care university hospital
Methods: We measured the
features of PTSD, anxiety, and depression using validated scales
(PSS-SR, Zung anxiety scale, and PHQ-9 respectively), employing an
anonymous survey of sequential consenting patients admitted with
critical illness, their associated family next-of-kin (NOK), and members
of the clinical staff involved (medical, nursing, and allied health).
Survey was administered to patients and NOK at 28 days after ICU
discharge, and to staff at patient admission.
Results: 30 patients,
next-of-kin, and associated medical/nursing/allied health staff were
approached. Participants included 60%, 50%, and 58% of eligible
patients, NOK, and staff respectively. Among patients, NOK, and staff
respectively, features consistent with the diagnoses of PTSD (50%, 33%,
19%), anxiety (61%, 33%, 41%), and depression (39%, 20%, 16%) were
observed, substantially higher than expected based on population
prevalence estimates.
Background
A critical illness is a life-threatening event that
induces an intense response in its victim. Common, primordial responses
to imminent threats to life include fear and anger. Sadness, also a
basic emotion, intervenes concurrent with a sense of loss, whether acute
or chronic. Long term adverse sequelae after exposure to intense
life-threatening events include anxiety, depression, and post-traumatic
stress disorder (PTSD). Not surprisingly, these conditions occur more
frequently among critical care survivors than among the rest of the
population. Less is known about the incidence and prevalence of these
conditions among the families of critical care survivors and among
critical care practitioners [1-11].
Anxiety is characterized by excessive and usually
irrational concern about erstwhile non-threatening events or possible
events that is disruptive because it interferes with normal social or
economic function. It is distinguished from fear, a basic human emotion,
in that fear is directed at a realistic threat e.g. imminent death
during a critical illness. The life-time prevalence of anxiety in the
general population is approximately 10%. Generalized anxiety disorder is
described in the Diagnostic and Statistical Manual IV as including
three or more symptoms of restlessness, difficulty with sleep,
irritability, difficulty concentrating, or muscle tension in response to
normal stressors, and that interfere with usual function.
Depression similarly has a life-time population
prevalence of approximately 10%. As a major mood disorder, its
diagnostic features include significant variations in appetite, sleep,
concentration, and interactions with others, that interfere with usual
social and economic function.
PTSD is a mood disorder that is related to both depression
and anxiety, including features of each. The most distinct feature
of PTSD is its beginning with a traumatic event or series. Other
features include intrusive thoughts in relation to the traumatic
event that interfere with normal function, avoidance of scenarios
or places that may facilitate recall of the instigating event, and
biologic manifestations of a stress response such as sweating,
tachypnea, tachycardia, and flushing.
We sought to evaluate the incidence of anxiety, depression,
and PTSD among critical care survivors and their families, and
the prevalence of these among critical care practitioners. Our
objective was to determine whether these conditions occurred
at a different frequency compared to the non-critically ill
population and their families, and if so which of them was most
frequent.
Methods
The University of Alberta Hospital is a tertiary care centre,
within which the General Systems ICU (GSICU) includes 28 beds
for patients with medical, surgical, and traumatic critical illness.
After institutional approval, we conducted a survey of patients
(survivors), their families (immediate next-of-kin (NOK)), and
the providers involved in their care..
In June 2012, thirty consecutive unselected surviving ICU
patients and their NOK were approached and invited to provide
informed written consent for this investigation. Staff members
were invited to participate on the basis of providing care to
the participating patients at the time of their admission to the
ICU. Invited participating staff included the nurse, respiratory
therapist, resident, dietician, pharmacist, physiotherapist, and
attending staff for each patient. Staff members were limited to
participating once.
The survey was delivered to patients and their NOK at 28
days after ICU discharge, either using the standard postal
service if the patient had been discharged or transferred, or via
hand delivery if the patient remained in hospital. Surveys were
contained within a stamped self-addressed return envelope that
did not include personal identifiers. Surveys were delivered to
staff using hospital mail, using the same method of stamped selfaddressed
return envelope. The investigation was announced
and described to providers, who were advised of the study
methods. Provider consent was implied by survey completion,
and surveys did not include identifying information.
The survey consisted of three combined scales, and
nonidentifying
demographic descriptors. To assess the presence
of anxiety and depression, we used the Zung self-reported
anxiety scale and the patient depression questionnaire (PHQ-
9) respectively. PTSD was assessed using the post-traumatic
symptom scale (PSS-SR). Using the Zung scale, anxiety was
defined as a score of greater than 15. Depression was defined as
a score of greater than 15 on the PHQ-9. PTSD was defined as a score of
greater than 17 on the PSS-SR scale. Each of these scales
has been validated independently and shown to provide good
inter-rater and intra-rater reliability and validity [12-17].
Results
Of 30 patients and NOK approached, 18 patients (60%) and
15 NOK (50%) responded. Of ICU staff, 30 nurses, 5 respiratory
therapists, 2 dieticians, 2 physiotherapists, 2 pharmacists, 8
resident physicians and 6 attending physicians were invited to
participate. Responses were received from 20 nurses (67%), 3
respiratory therapists (60%), 6 resident physicians (75%), and
3 attending physicians (50%). No responses were received from
dieticians, physiotherapists, or pharmacists. The subsequent
results are based on the total of 65 responses received (overall
response rate 57%).
Considering Table 1, among patients participating after
surviving a critical illness, 50% met diagnostic criteria for PTSD
at 28 days after ICU discharge using the screening questionnaire
PSS-SR. This was also observed among 33% of the participating
NOK and among 19% of staff.
Also in Table 1, anxiety was present according to the Zung
scale among 61% of participating surviving patients and among
33% of the participating NOK. Anxiety was present among 41%
of critical care staff.
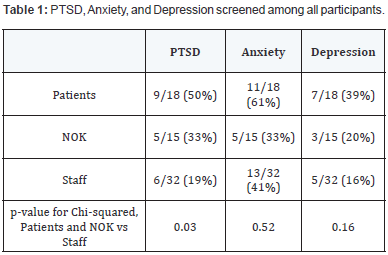
With regard to depression as measured by the PHQ-9, this
was present among 39% of participating surviving patients and
was present among 20% of their NOK. Depression was present
among 16% of participating staff.
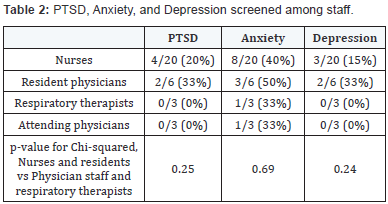
In Table 2, the presence of PTSD, anxiety, and depression
was considered among participating staff according to staff
category (e.g. nurse, physician, etc.). Symptoms of each of
PTSD, anxiety, and depression were more common among
participating nursing staff and resident physicians than among
participating respiratory therapists and attending physicians. It
was previously noted that none of the invited physiotherapists,
pharmacists, and dieticians participated in the survey, and no
conclusions can be drawn about these groups.
Discussion
The critical care unit in any hospital admits patients with the
greatest degree of physiologic disturbance and greatest threat
to life of patients in the hospital. The threat to life can leave
survivors and their NOK with persistent residual disturbances
in mood as a consequence of that threat. Constant exposure to
patients and NOK under threat to life may also be associated
with mood disturbance among bedside staff.
In this survey, we discovered that the prevalence of each of
PTSD, anxiety and depression were substantially higher among
patients, NOK, and staff than would have been expected based
on the general population prevalence of these conditions. While
detection of these mood disorders in ICU survivors and NOK
has been reported in the literature [1-11], this study represents
possibly one of the first that describes these conditions among
ICU staff. Further exploration of the causes and consequences of
these relatively increased incidences and prevalence, as well as
attention to prevention and treatment, may be appropriate.
Each of PTSD, anxiety, and depression are disorders that can
occupy a spectrum of implications on those with these conditions
ranging from mildly inconvenient to debilitating. Socially, their
recognition continues to carry varying levels of stigma that may
further reduce both their perceived prevalence and reported
significance. Consequently, the social burden of these conditions
may be substantially greater than measured in studies such as
this [12-13].
While we detected relatively increased prevalence of these
conditions among surviving patients and NOK, we were unable
to measure the duration of the conditions. Further investigation
to determine duration of these disorders would be appropriate.
We did not have the medical nor nursing resource to
address the effectiveness of possible preventive or therapeutic
manoeuvres. While we did advise participants to contact their
family physicians in event of concerns, we did not wish to
raise expectation bias in survey completion by emphasizing
therapeutic options.
The therapies available for these conditions range from
cognitive behavioural therapy to pharmaceutical. In the most
severe scenarios, patients may be treatment-resistant and debilitated. Consequently, identification of preventive strategies
may be beneficial [12-18].
The higher prevalence of these disorders among nursing
staff and resident physicians is somewhat in keeping with
other findings in the literature showing higher prevalence
of such conditions among first-responders to critical events.
First-responders have less ability to remove themselves from
exposure to events that are life-threatening to patients, and may
suffer from internalization of this exposure. On the other hand,
attending staff and associated staff (e.g. pharmacists, dieticians)
may be unaware of the significance of the perceived threats to
life on bedside providers. A greater level of awareness of this
may be appropriate for both first-responders and for those more
removed from the moment-to-moment intensity.
This study was too small to evaluate association between
severity of patient illness and its effect on immediate NOK or
on immediate care givers. Further investigation could evaluate
these hypotheses.
Considering the prevalence of these conditions among
patients, it is noted that this was a sequential (cross-sectional)
non-randomized survey that was done at 28 days after ICU
discharge and was obviously limited to survivors. Administration
of this survey later after discharge may have resulted in a
different detected prevalence of these conditions. However, due
to timing constraints, we were not able to include patients that
were admitted during the study period and survived but that
remained within the ICU due to severity of illness. These patients
would likely have been exposed to greater threat, as would
also have been the case for their NOK. A randomized design
performed over a longer period of time may have achieved
a different result, as the conclusions of this study may have
been affected by timing of administration. Finally, the response
rate (60%) among patients was reasonable to allow some
generalization to the surviving non-responding patients. The
response rate among NOK was slightly lower, and was limited
to study of NOK of surviving patients. Interestingly, the response
rate among staff was similar to that among patients, and is also
probably appropriate for some generalization.
Within these limitations, the incidences of PTSD, anxiety,
and depression were higher among patients and NOK, as well
as among staff, than expected among the population at large.
Consideration of further investigation to determine causes
of these conditions in these groups, as well as to evaluate
prevention, treatment, and long-term sequelae, would be
appropriate.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment