Surviving Major Trauma with Hemipelvectomy-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Traumatic hemipelvectomy is a life threatening,
however rare injury associated with high lethality. It comes along with
excessive blood loss, related hemodynamic instability and injuries of
the genitor-urinary system or the rectum. The real incidence is unknown
because most patients die before reaching the hospital. The treatment
requires a rapid, multidisciplinary team approach focused on hemorrhage
control to correct coagulopathy and clear persistent signs of tissue
hypoperfusion to save the patient’s life [1].
Improvements in prehospital rescue systems and initial trauma response
have resulted in increased chances of survival. Most survivors are
young, healthy individuals, who are able to tolerate massive hemorrhage
and soft-tissue destruction [2-6].
We present a case of an open fracture of the ileosacral joint, wide
open symphysis, complete hemipelvectomy and severe soft tissue trauma,
including a decollement around the pelvis and the left abdomen.
Case Report
A case of an 18-year-old woman surviving traumatic
hemipelvectomy is presented. The woman was involved in a high speed
motorcycle accident. She was caught by a gusting wind and thereby
accidently left the road by crossing the midline onto the oncoming lane
and crashed frontally into an oncoming car. In primary survey on scene
the assessment following Adult Trauma and life Support (ATLS) guidelines
revealed an AB stabile and cardial compensated patient with Glasgow
Coma Scale (GCS) of 15 points, despite a considerable blood loss, an
unstable pelvis and a cold, mottled, pulse less left leg. Her lower left
limb showed an open third degree femur-fracture, as well as a grotesque
deformation of the lower limb and left hemi-abdomen. The woman was
wearing full motorcycle clothing and a helmet. On site the thorax only
showed some excoriations and no instability, as far as visible. Because
of the extensive trauma which came along with fulminate pain, anesthesia
was introduced by the flying doctor to perform an appropriate pain
management. The woman was managed with fluid to maintain a hemodynamic
stability. Hemorrhage control was obtained with compression of the
wounds and she was then transferred by HEMS to the next trauma centre.
There were no further diagnoses set in the secondary survey.
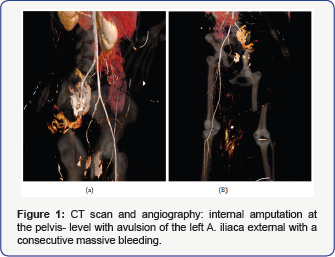
Upon arrival at the trauma center she was
hemodynamically unstable, due to a covered aortic rupture loco typical,
an internal amputationatthe pelvic level with consecutive
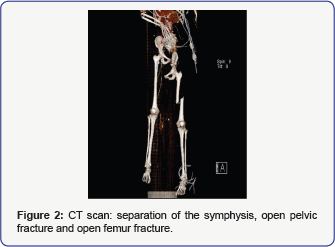
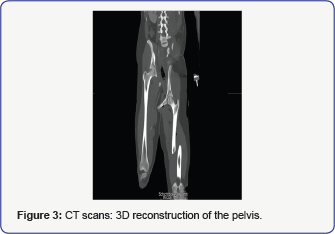
massivehemorrhage (Figure 1a,1b), separation of the symphysis (Figure 2 & 3), an open pelvic fracture (Figure 2 & 3)
and an open femur fracture (Injury severity score = 59). Explicitly the
whole body trauma computer tomography revealed the following principal
diagnosis. A covered aortic rupture loco typical, an internal amputation
at the pelvis- level with avulsion of the left a iliaca external with a
consecutive massive bleeding (Figure 1a).
Separation of the symphysis, an open pelvic fracture with gas inclusion
at the caudal spinal cord coming from a SWK4/5 fracture, and an open
femur fracture was seen (Figure 2 & 3).
Additionally there was no perfusion seen in the angiography providing
blood for the left lower limb, which was actively bleeding at that
moment. An urgent angiogram revealed occlusion of the left external
iliac artery. There was a haemathothorax seen on the left side of the
thorax, shifting the trachea and the esophagus to the right, however
without leading to oxygenation problems. No intracranial pathology was
found in the computer tomography. Immediate surgical homeostasis and
debridement was attempted for primary damage control. To save the
patient’s life it was necessary to perform aggressive surgery with a
complete amputation of the left hemi pelvis including the left lower
limb. Additionally, a skin flap was provided. A limb- saving procedure
would have endangered the patient’s life. Furthermore, the patient
underwent embolization of the left common iliac artery and vein and a
Thoracic Endovascular Aortic Repair (TEVAR) of the aortic rupture.
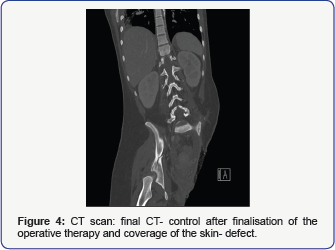
In the further hospital course, frequent second-look
operations and numerous revisions of the soft tissue injury,
reconstructive surgery and dedicated surgical care to avoid septic
complications were needed. In the following the woman was throughout in a
stable mental state, nevertheless psychological assistance was directly
started after completion of the first surgery. After finalization of
the operative therapy and coverage of the skin defect the woman was
transferred to a rehabilitation centre 9 weeks after the accident (Figure 4).
She then was transferred to a trauma centre to adjust an artificial
limb. In summary, this patient is one of the few survivors of an ISS of
59 points reported in the world literature [2-4].
She was able to survive a major trauma by accurate and rapid early
management, rapid transport to the operating room and an aggressive
surgical approach all contributed to survival.
Conclusion
The leading injury was a traumatic hemipelvectomy
coming along with the disruption of the pelvic neurovascular integrity
and a covered aortic rupture loco typico. The accepted definition of
traumatic hemipelvectomy is as follows: unstable ligament us or osseous
hemi pelvic fracture/amputation, (open or closed) accompanied by an
injury with rupture of the pelvic neurovascular bundle [5].
Most survivors are young, healthy individuals, who are able to tolerate
massive hemorrhage and soft-tissue destruction. When the criteria or
traumatic hemipelvectomy are fulfilled, surgical completion of the
hemipelvectomy is mandatory to safe a patient's life [4,6].
Whereas mortality in open pelvic fractures is around 40%, it is 60 to
100% in traumatic hemipelvectomies, and bleeding is the main cause of
death [3,6].
In conclusion, traumatic hemipelvectomy is a rarely seen, often fatal
injury which requires immediate life support and surgery. This injury
always requires a rapid, multidisciplinary team approach, including an
orthopedist, vascular surgeon, general surgeon, urologist and
anesthesiologist focused on hemorrhage control to correct coagulopathy
and clear persistent signs of tissue hypo perfusion. Furthermore, the
involvement of rehabilitation specialists is advantageous for personal
well-being and social reintegration. Eighty percent of injuries occur as
a result of motorcycle accidents [3].
Although hemipelvectomy is a devastating injury, patients can be
successfully rehabilitated to an active and productive role in society.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment