The Effect of Different Intrathecal Doses of Meperidine on Postoperative Pain Relief in Patients Undergoing TURP Surgery-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Introduction: The purpose of this study was to
investigate the effect of adding different doses of meperidine to
intrathecal hyperbaric bupivacaine on anesthetic characteristics and
postoperative pain relief in patients undergoing elective transurethral
resection of prostate (TURP) surgery.
Methods: ASA I-III 90 patients undergoing
elective transurethral resection surgery with spinal anesthesia were
included in this prospective, randomized, double-blinded study.
Following a spinal tap, patients were randomly divided into 3 equal
groups: In group B; 12.5 mg of 0.5% hyperbaric bupivacaine was given
intrathecally. In BM15 and BM30 groups, meperidine with dose of 15 mg or
30 mg was added to 10 mg hyperbaric bupivacaine, respectively.
Results: The maximum sensory block level is T8
in all groups and the duration time to reach to T8 was found shortest
in Group B (Compared to Group BM 30 and Group BM 15) (p = 0.029, p =
0.017 respectiveliy). In Group B, motor block level is higher and
termination time of motor block is longer compared to both meperidin
added groups (p = 0.019, p = 0.022). Sensory block levels of Group BM 15
and Group BM 30 were found longer compared to Group B (p = 0.004, p =
0.006 respectively) and motor block levels of theese groups were found
more shorter compared to Group B (p=0,048). In BM15 and BM30 Groups,
postoperative pain scores were found lower (p≤0,001) and side effects
and complications were similar between theese groups.
Discussion and Conclusion: Combination of
hyperbaric bupivacaine with meperidine may offers the advantage of
better postoperative analgesia and it may be used as an alternative to
pure hyperbaric bupivacaine solution in spinal anesthesia, for TURP
surgery.
Keywords: Spinal anaesthesia; Transurethral resection of the prostate; Meperidine.Introduction
Transurethral resection of prostate (TURP) surgery
has still continued to be the gold standard among the surgical
treatments applied for benign prostatic hyperplasia (BPH), today [1].
TURP operations, it is more commonly preferred compared to general
anaesthesia since it allows the early diagnosis of negativities such as
regional anaesthesia fluid loading, bladder perforation, and TURP
Sydrome. When the local anaesthetics are used appropriately and
attentively in spinal anaesthesia, they have very few side effects. [2-4]
Most of the patients who underwent a TUR-P operation are in their
advanced ages and have respiratory and cardiac comorbidities. Therefore,
it is important for such patients to prevent hypotension, bradycardia,
and respiratory distress related to spinal anaesthesia [4].
(4) In order to achieve an efficient anaesthesia for the TUR-P
operation, it is required to form the block at T10 level. Insufficient
anaesthesia causes additional problems for the patient. Injection of low
dose opioids together with local anaesthetics in regional blocks
increases the potency of analgesia [5-7].
One of postoperative pain treatment methods is intrathecal multimodal analgesia [8].
It has been shown through experimental studies that the application of
analgesia before the surgical trauma may reduce post-traumatic
sensitivity and secondary hyperalgesia in the spinal cord [9,10]. For this purpose, multimodal or balance analgesia occupies a significant place recently in the postoperative pain treatment [11,12].
The main purpose of postoperative pain treatment is to reduce and
eliminate the discomfort, contribute to the recovery period, reduce the
side effects caused by the treatment or control them efficiently and
reduce the costs of the treatment. Nowadays, spinal anaesthesia has
still maintained its popularity method in lower abdominal, orthopaedic,
obstetric and gynaecologic surgeries, elective, emergency or ambulatory
surgery [13].
Sensory block level is important for a successful
spinal anaesthesia. As is known, sensory block is affected by these
factors: baricity, dose, volume, concentration, and injection rate of
the local anaesthetic, patient's position, barbotage, patient's
characteristics (such as height, body weight, and age) and other
adjuvant agents. Among these factors; the baricity of the local
anaesthetic which is associated with the patient’s position is defined
as the most important factor in the distribution of the local
anaesthetic [14].
An undesirable hypotension is encountered as a result of the
cardiovascular effect associated with the sympathetic blockage caused by
the spinal anaesthesia, and this rate is reported to be 33% in a study [15]. This creates a secondary ischemia risk especially in the advanced age group with high incidence of coronary disease [16].
Considering that most of cases undergoing TURP operations are old
patients with low cardiac reserves, this presents importance. Therefore,
dose of the local anaesthetic used for protection from hypotension was
reduced; however, this time the aimed sensory block could not be
reached. Due to this problem, the aimed sensory block was tried to be
reached through minimal hemodynamic exposure by providing synergistic
analgesia after adding opioid into the local anaesthetic agent used
intrathecally [17,18].
The purpose of this study was to investigate the
effect of adding different doses of meperidine to intrathecal hyperbaric
bupivacaine on anesthetic characteristics and postoperative pain relief
in patients undergoing elective TURP surgery.
Materials and Methods
After receiving an ethical committee approval from
Ondokuz Mayis University and written consents of patients, a total of 90
male patients between 50-80 years of age and ASA (American Society of
Anesthesiologists) I-III undergone elective endoscopic TUR surgery under
spinal anaesthesia were included in the study. Patients, who refused
the spinal anaesthesia, with motor or sensory deficit and
contraindications to spinal anesthesia such as coagulaton disorder and
infection at the puncture site were excluded from the study. It was also
planned to exclude the patients, who demonstrated insufficient block
after the practice, whose preoperative VAS score was 4 and above, or who
needed the use of additional analgesic during surgery and were required
to be transferred to general anaesthesia, from the study.
Preoperatively, 10ml/kg of 0.9% NaCl solution was infused to patients
before spinal anaesthesia and no additional premedication was used. In
the operating room, standard monitoring including non-invasive arterial
pressure, electrocardiography (ECG) and pulse oximetry (SPO2)
was established for all patients. Spinal anaesthesia was applied using a
midline approach from the 4th-5th lumbar segment in sitting position
with a 22 G Quincke type spinal needle (B Braun, Spinocan, Melsungen,
Germany). Patients were divided into 3 groups randomly using a computer
generated random number table: In group B (n=30); 12.5 mg of 0.5%
hyperbaric bupivacaine (Bustesin® Spinal Heavy 0.5%, VEM llaf, Istanbul,
Turkey) was given intrathecally.In group BM15 (n=30), 15 mg meperidine
(Aldolan®, 100 mg, G.L. Pharma GmbH, Lannach, Austria) and in group BM30
(n=30), 30 mg meperidine with 10 mg of 0.5% hyperbaric was administered
intrathecally. Patients' blood pressure, heart rate and oxygen
saturation were monitored and recorded every 5 minutes during the
operation. While sensory block level was evaluated by using pin prick
test, motor block degree was assessed by using Bromage scale. (Bromage
scale 0: no motor block; 1: cannot move hip, can move knees and feet; 2:
cannot move knees and hip, can move feet; 3: cannot move hip, knees and
feet). Disintegration of the motor block was recorded as the period
that Bromage scale regressed to point 0. Sensory block's duration of
reaching to T8 dermatome, the maximum sensory block level, the maximum
motor block level and the duration of reaching to this level were
recorded. Surgery was initiated when sensory block formed at T8 level.
At the beginning of the surgery, the pain level was scored with VAS
scale. After spinal anaesthesia, the decrease of the Mean Arterial
Pressure (MAP) above the rate of 25% compared to the measurement before
administration or the decrease of systolic blood pressure below 90mmHg
considered as hypotension and 5mg iv ephedrine doses were injected in
order to bring the blood pressure to normal limits. The decrease of
heart apex beat under 40 beats/minute was accepted as bradycardia and
atropine doses of 0.5mg were injected in order to increase the heart
beat rates above 50 beats/minute. Within the period until the sensory
and motor block effects of spinal anaesthesia disappeared; patients were
followed up in terms of side effects such as hypotension, bradycardia,
nausea, vomiting, uneasiness, and shivering; and problems such as
headache, back and leg pain, loss of strength, urination and fecal
incontinence until being discharged from the hospital. In the first 24
postoperative hours, VAS scores of patients were assessed for 7 times in
post-operative 1st, 2nd, 4th, 6th, 12th and 24th
hours with the first assessment being in the hour 0 in the recovery
unit; patients who needed additional analgesic, the first minute that
the need for analgesic was arisen and the total amount of analgesic used
as mg were recorded. 50 mg of dexketoprofen trometamol was administered
intravenously to patients who needed analgesic (Leodex 50 mg /2ml
ampoules, Bilim llaf, Istanbul, Turkey). SPSS (Statistical Package for
Social Sciences) for Windows 19.0 program was used to conduct
statistical analyses. Regarding assessment of the data of the study;
along with descriptive statistical methods (mean, Standard deviation),
Oneway Anova test was used to compare parameters demonstrating normal
distribution among groups for comparing quantitative data, and Tukey HDS
test was used for the determination of the group that caused
difference. On the other hand, Chi-Square test was used to compare
qualitative data. While the presence of a difference between groups in
terms of VAS was examined by using MannWhitney U-test, changes within
groups were assessed by using Friedman test. Significance level was
accepted as p<0.05.
Results
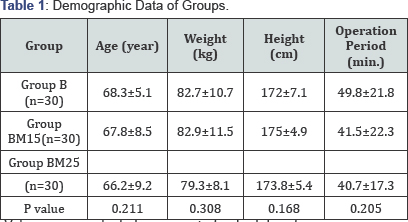
Values were evaluated as mean � standard deviation.
The demographic data of patients and surgery periods were found to be similar among groups. It is shown in Table 1.
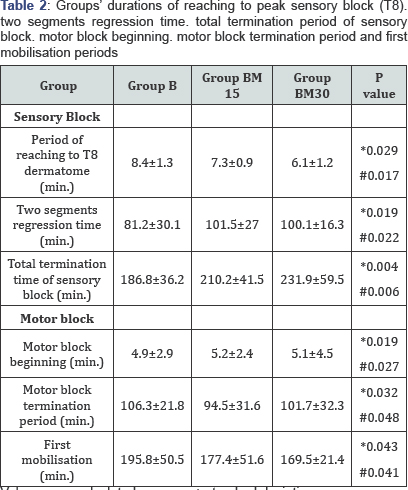
(p>0.05) The maximum sensory block level was T8 in all 3 groups.
Sensory block’s duration of reaching to T8 dermatome and the total
sensory block duration were 8.4±1.3 minute and 186.8±36.2 minute in
Group B; 7.3±0.9 minute and 210.2±41.5 minute in Group BM15; and 6.1±1.2
minute and 231.9±59.5 minute in Group BM30. The durations of reaching
T8 dermatome of Group B were moderate higher than Group BM15 (p=0.029)
and Group BM 30 (p=0.017). Sensory block duration of Group B was lower
than Group BM15 and Group BM30 (p=0.004, p=0.006; respectively). The
longest sensory block duration was found in Group BM30. The sensory
block duration in Group BM 15 was shorter than Group BM30 and longer
than Group B (Table 2).
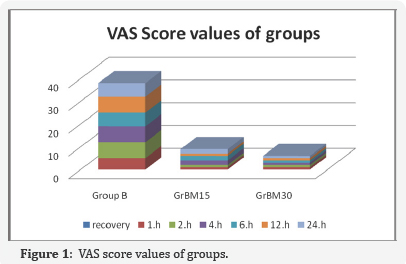
Post-operative average VAS (Visual analogue scale) values were
significantly lower in Group BM15 and Group BM30 compared to Group B in
second, fourth, sixth and twelfth hours. (p< 0.001) (Table 3) VAS scores were found to be similar in all 3 groups in recovery unit (hour 0) and post-operative 1st and 24th hours (Figure 1).

**p: Comparison of Group B-Group BM15
***p: Comparison of Group B-Group Group BM 30
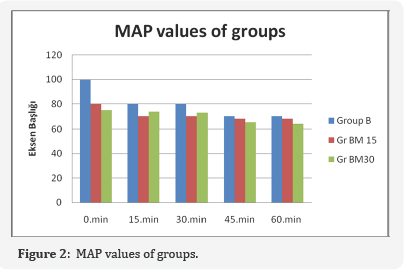
Our perioperative vital results, MAP; heart rate (HR)
values,were recorded separately for all 3 groups. Measurement times of
vital results were realised for 6 times with 15-minute intervals. The
first measurement time was preoperative value; measurement value right
after applying spinal anaesthesia was accepted as minute 0 of the
operation. Following measurements were recorded as perioperative results
of 0. ,15th, 30th, 45th, 60th minutes. Postoperative results were recorded as 60th, and 70th minutes in the recovery unit. Mean Arterial Pressure (MAP) was similar among the groups in all measurement times (Figure 2). Similarly, heart rate (HR) values have also been found to be similar in all measurement times among groups (Figure 3).
Perioperative hemodynamic findings were observed to be more stable in
the groups to which intrathecal meperidine was administered as a
clinical observation in Groups BM15 and BM30. Especially after spinal
anaesthesia was used, the bradycardia and hypotension appearing
depending on sympathetic blockage were not observed at all in Groups
BM15 and BM30. Postoperative pain scores were significantly low in terms
of both statistics and clinical observation in the groups to which
intrathecal meperidine was added.

Satisfaction level was very good among all cases and
surgeons in Group BM30. One surgeon reported a moderate level of
satisfaction and two cases again reported a moderate level of
satisfaction in Group B. One surgeon reported a moderate level of
satisfaction and patient satisfaction was very good among all patients
in Group BM15. Bradycardia and hypotension developed in three patients
in the 13th, 16th and 21st minutes of
the operation in perioperative Group B, 5 mg ephedrine i.v was
administered and fast responses were received. No significant
perioperative side effect was observed in other groups. Serious side
effects such as nausea, vomiting, itching, and hypotension were not
observed in all 3 groups in the postoperative period. Itching
complication was observed in only one case in Group BM30 and itching was
recovered with administration of 10 mg oral antihistaminic cetirizine. 3
patients needed additional analgesic (10%) in Group BM15 within the
first 24 hours in the postoperative period; whereas, only 2 patients
(6.6%) in Group BM30 and 18 patients (60%) in Group B needed additional
parenteral analgesic.
Discussion
This study has revealed that meperidine added
intrathecally in TURP operations ensured a significant hemodynamic
stabilisation in the perioperative period and allowed the patient to
feel less pain in the postoperative period and therefore ensured a
comfortable postoperative period.
In a study conducted by Anaraki et al. [19]
77 cases to undergo open prostatectomy received spinal anaesthesia with
hyperbaric lidocaine and half of the cases also received intrathecally
0.3mg/kg meperidine in addition to hyperbaric lidocaine. In the group
with a low dose of meperidine; it was observed that there was no
difference in terms of hemodynamic stability in the perioprative period;
however, there were long painless periods in the postoperative period
and blood loss reduced evidently [19].
The study conducted by Anaraki et al., had totally parallel results
with our study, because similarly in our study, no difference was
observed in terms of hemodynamic stability in groups to which a low dose
of meperidine was added; whereas, these groups had a significant
advantage in terms of postoperative analgesia (Table 3). In another study conducted by Patel et al. [20]
42 cases, who were planned to undergo endoscopic urological surgery,
were divided into two groups; and while one group received intrathecal
0.5 mg/kg 5% lidocaine, the other group received 0.5 mg/kg meperidine
intrathecally. The duration of reaching the peak sensory level was found
to be significantly short in the group that received lidocaine, and
when sensory block termination times and motor block beginning and motor
block termination periods were compared, no difference was observed
between the two groups. When compared in terms of hemodynamic stability;
while the group administered with meperidine was more stabile in
hemodynamic aspect, a more significant decrease was observed in mean
arterial pressures in the group that received lidocaine and it was
observed that there were many patients that needed intervention with
intravenous ephedrine [20].
Our clinical observation results showed that hemodynamics were more
stabile in groups that received meperidine; because bradycardia and
hypotension developed in 3 patients in the group that received 12.5 mg
hyperbaric bupivacaine were intervened with 5 mg of ephedrine i.v. In
this study, the reason for not finding any significant difference in
terms of hemodynamic stability may be associated with the fact that we
used hyperbaric agents in all groups. In this study, no bradycardia and
hypotension cases that needed intervention with ephedrine were
encountered in groups where we added meperidine, because this may be
related to the fact that the added meperidine increased bupivacaine
baricity even more [21].
In a study conducted by Murto et al., 42 patients to undergo TUR-P
operations were divided into three equal groups; one group was
administered with 5% lidocaine 75 mg intrathecally, the second group
received 0.15 mg /kg meperidine in addition to 75 mg of 5% lidocaine,
and the third group received 0.30 mg/kg meperidine along with the same
dose of lidocaine. Sensory block's duration of reaching T10 dermatome
level was only found faster in the group that received lidocaine, and
slower in groups administered with meperidine. In a study conducted by
Chun et al., 0.2 mg /kg and 0,4 mg / kg meperidine with 8 mg of 0.5%
hyperbaric bupivacaine for 25 cases to undergo TUR-P operation was
reported to prevent considerably shivering, which may be a commonly
encountered situation of TUR-P operations, in the postoperative period [21]. When Chun et al. [21]
compared the group which received only 8 mg of 0.5% hyperbaric
bupivacaine with the groups which received meperidine in terms of other
side effects, it was observed that there were more itching complication
in the group that received meperidine [21].
In our study, only one patient had an itching complication in group
BM30, which was recovered by one oral dose of Cetirizine 10mg (Zyrtec®,
10 mg tablets, UCB Pharma, England). In a study conducted by Movafegh et
al., [22]
56 patients to undergo an inguinal hernia repair received 15 mg
meperidine in addition to 15mg of 0.5% hyperbaric bupivacaine
intrathecally and the patients were divided into two equal groups. No
premedication was given to the control group while the study group
received premedication with 0.1 mg/kg i.v dexamethasone. Possible side
effect profiles of the groups (nausea, vomiting, pruritus, and
respiratory depression) were observed in the postoperative period. In
cases premedicated with dexamethasone, all possible side effects were
less observed in the postoperative period and even the patients were
reported to have much higher postoperative pain scores [22].
Although it was emphasized that premedication with dexamethasone may
not be reliable for every patient (particularly for the patients with
diabetes); it was stated that it may have created a synergism with
meperidine in the postoperative pain control [22].
In our study, no additional premedication was administered on any of
the patients and no serious side effect was observed in all the groups.
No respiratory depression was observed in any of 56 cases in the study
conducted by Movafegh et al. [22].
Similarly in our study, no respiratory depression was observed among
the cases; however when we reviewed the literature, it has been reported
that isolated cases have had the respiratory depression with a dose of
intrathecal meperidine above 0.5 mg/kg [23].
Comparative studies have been conducted on the
elective caesarean section cases related to the use of meperidine as
intrathecally isolated or in combination with local anaesthetics. In a
study conducted by Kafle, 50 pregnant women who reached the last stage
(mature gravida) were divided into two groups and one group received 5%
meperidine intrathecally with a dose of 1mgs/kg; whereas, the other
group received 5% lidocaine with a volume of 1.2-1.4 ml intrathecally.
While pruritus and tendency to sleep were more commonly observed in the
group to which meperidine was administered, the hypotension was more
commonly encountered in the lidocaine group. The minimum postoperative
painless period was 6 hours in the meperidine group; whereas, the
postoperative painless period was limited with only one hour in the
lidocaine group and therefore, there was a high need for analgesic in
the lidocaine group [24]. Similarly, Atalay et al., [25]
divided 80 pregnant women, in their term stages among elective
caesarean section cases, into 4 equal groups; 10 mg hyperbaric
bupivacaine was administered to the first group, 5 mg isobaric
bupivacaine and 25 mg meperidine to the 2nd group, and 30 and
35 mg meperidine respectively along with 5 mg isobaric bupivacaine to
the last two groups. Hemodynamic stabilities of groups in the
perioperative period were noted, and their motor block levels, sensory
block levels, side effects such as nausea, vomiting and itching and the
Apgar scores of the newborns were compared in the postoperative period
by using Bromage scale. Motor block time was found to be better in
groups that received meperidine. Postoperative analgesia quality was
once again found to be higher in groups that received meperidine;
however, no additional benefit was reported when the group receiving 35
and 30 mg meperidine and the group receiving 25 mg meperidine as the
lowest dose were compared. Additionally, the group that received a low
dose of meperidine (25 mg meperidine) was emphasized to be more
advantageous in terms of postoperative side effect profile compared to
all groups. These results are in parallel with our study because the
group BM15 achieved a postoperative analgesia quality as high as the
group BM30, and did not provide any additional advantage in terms of
perioperative hemodynamic stability [25]. In a study conducted by YektaŞ [26]
for the purpose of intrathecal multimodal analgesia; 100 male cases to
undergo inguinal hernia repair were divided into 5 groups that consisted
of 20 patients and, 15 mg hyperbaric bupivacaine and 0.5 ml
physiological saline solution were administered to the first group, 17.5
mg hyperbaric bupivacaine the 2nd group, 25 mcg fentanyl and 15 mg hyperbaric bupivacaine to the 3rd group, and 2.5 mcg sufentanyl to the 4th
group; whereas, the last group received TIVA (Total Intravenous
Anaesthesia). When the postoperative pain scores of groups were
compared, they were better in the groups, which received fentanyl and
sufentanyl (3rd and 4th groups) with the purpose of intrathecal multimodal analgesia, compared to all groups [26].
Similar results were obtained in our study; postoperative analgesia
quality was higher in groups in which meperidine was added to
intrathecal hyperbaric bupivacaine.
Consequently, low dose of meperidine added to
bupivacaine by reducing the hyperbaric bupivacaine dose in TURP
operations ensured more reliable hemodynamic conditions in perioperative
terms and increased analgesia quality in the postoperative period.
Endoscopic urologic interventions are commonly performed on the
population of geriatric patients with poor cardiac reserves; therefore,
the combination of a low dose of bupivacaine with a low dose of
meperidine may be a good option for this patient population. At the same
time; it may be an alternative option for lower extremity surgery,
inguinal hernia repair, obstetrics and gynaecology for the purpose of
intrathecal multimodal analgesia. In our study and in similar studies,
it has been reported that the intrathecal use of a high dose of
meperidine does not provide any additional advantage; nevertheless
future studies are required in order to research the optimum intrathecal
dose of meperidine.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment