Our Scalp Block Results in Craniotomy Cases-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Aim: The aim of this study is to investigate
the effect of scalp block performed with 0,5% of bupivacaine in
craniotomy cases in preventing hemodynamic response due to the incision
and its effect on postoperative analgesia and the need of analgesics.
Materials and method: The study was planned as
a randomized, placebo controlled, double-blind study. 40 patients
between the ages of 40-85 with ASA II-III classification were included
in the study for elective craniotomy after the approval of the ethics
committee and informed consents of the patients were received and they
were separated into two groups (Group S: 20ml 0,9% normal saline, n=20),
(Group B: 20ml0, 5% Bupivakain, n=20). Scalp block was performed 15
minutes before craniotomy. The mean arterial pressure (MAP) and heart
rate (HR) of the patients wererecorded. Postoperative complications
observed in the recovery room (bradycardia, hypotension, drug allergy,
nausea, vomiting) were recorded. Pain was evaluated in postoperative
conscious patients in the 2, 4, 8, 12, 16 and 24th hours with a 10cm
visual analogue scale; and it was planned to administer 75mg of
intramuscular meperidine if the VAS score was 5 and above in the
postoperative period.
Result: During the craniotomy the MAP and HR
values of the patients in Group S were significantly higher than Group B
(p<0.05 respectively p=0.002, p=0.029). The VAS scores were also
significantly higher in Group S compared to Group B in the postoperative
1, 2, 4, 6 and 12th hours (p<0.05 respectively p=0.022, p=0.031).
Use of additional medication in Group S due to perioperative
hypertension and tachycardia was significantly higher in comparison with
Group B (p<0.001). Similarly, in terms of postoperative analgesic
need, Group B had significantly less need for analgesics. Regarding the
complications, however, no significant difference was found between the
two groups.
Conclusion: In conclusion, scalp block ensures
the stabilization of hemodynamic responses by reducing the sympathetic
response in the intraoperative period in craniotomy cases and helps
reduce the pain in the early postoperative period. We think that
bupivacaine can be effectively used in scalp block procedures.
Keywords: Scalp block; Craniotomy; BupivacaineIntroduction
The aim of neuroanesthesia is to prevent the increase
of intracranial pressure without distorting the cerebral autoregulation
and to ensure convenient surgical conditions and a safe anesthesia for
the patient by maintaining a sufficient level of cerebral perfusion
pressure (CPP). Anesthetic agents have obvious effects on cerebral
metabolism, cerebral blood flow, cerebrospinal fluid (CSF) dynamics,
intracranial volume and pressure [1].
As the intracranial pressure is directly related to the blood pressure,
it is crucial to prevent the elevation of blood pressure due to any
reason whatsoever in craniotomy patients. Radical elevations in systemic
arterial pressure may temporarily distort cerebral autoregulation and,
if not prevented, may cause cerebral edema by increasing the pressure in
cerebral capillaries. Particularly, in interventions related to lesions
involving intracranial areas, the detrimental effects of acute
hypertension are more obvious as intracranial compliance is already
decreased. Especially if the autoregulation capacity of cerebral vessels
is already compromised, this increase will lead to an increased
intracranial pressure [2].
Since increased intracranial pressure may cause a decrease in cerebral
perfusion pressure or a shift effect in the brain, it should absolutely
be prevented before durotomy [3].
Painful stimulants and sudden increases in blood
pressure and heart rate cause herniation, cerebral aneurism and
arteriovenous malformation rupture by increasing the intracranial
pressure, and lead to ischemia in subarachnoid hemorrhage patients, who
develop vasospasms, and an increase in the potential morbidity risk.
Furthermore, hemodynamic instability will lead to adverse effects in
those with atherosclerotic heart disease in the preoperative period [4,5].
Cranial surgical procedures involve continuous change in the intensity
of painful stimulants, therefore they require a very close monitoring of
the level of anesthesia [3,6].
The aim of scalp block is to block the nerves
innervating the scalp at their exit points from the scalp before they
form branches with the use of local anesthetic agents. Minor and major
occipital nerves innervating the scalp, supraorbital and supratrochlear
nerves, zygomaticotemporal nerve, auriculotemporal and major auricular
nerve are blocked. As a result, the transmission in the fibers located
in the nerve trunk in the area where the drug is delivered is blocked.
Scalp block was first defined by Pinosky and bupivacaine was used as the
local anesthetic agent. The most frequently used agent has also been
bupivacaine in further studies, however there are also some studies
performed with lidocaine, ropivacaine and levobupivacaine [5,7,8].
Mainly bupivacaine, ropivacaine and lidocaine have been used for scalp block in the studies [8-10].
Scalp block is a difficult technique requiring the use of local
anesthetics in high volumes, which in turn increases the risk of local
anesthetic toxicity in patients [9,11].
In awake craniotomies, an average of 150-175mg of levobupivacaine is
used for the scalp block and maximum concentration measured in the
plasma is 0.98-2.51µg/ml and the time needed to reach this level of
concentration is 5-15 minutes and no central nervous system or
cardiovascular system toxicity is observed at this level of
concentration. It is reported that post-craniotomy pain is less than the
pain experienced after operations such as lumbar laminectomy or fascial
reconstruction ]12[.
However, in contradiction to the general opinion, moderate or severe
pain after craniotomy is reported to be quite common and it is observed
that this pain is very intense particularly in the first 2 hours after
craniotomy [13].
For the treatment of this pain, either local anesthetics are injected
to the scar area or systemic nonsteroidal anti-inflammatory agents,
drugs such as ketamine, opioids, or tramadol are given. In the meantime,
there is still an ongoing search for an ideal analgesic agent and or
approach in craniotomy cases complaining of severe pain. If the patient
is conscious and have a perception of pain, postoperative analgesia
should absolutely be used [14-16].
Bupivacaine is an amide type local anesthetic and was developed by
Ekenstom et al. in 1963, it is available as hydrochloride salt in the
market. It provides analgesia without motor block in low densities.
Since it is highly fat-soluble, its systemic absorption is slow. It is
metabolized in the liver except for a small portion excreted through the
kidneys. It becomes effective within 5-10 minutes. This duration may
reach up to 20 minutes in caudal and peridural injections. Motor and
sensorial blockade may last up to 3 hours. It reaches maximum plasma
concentration after 30-45 minutes. Its half-life is 9 hours in adults.
It is one of the longest acting local anesthetics (5-16 hours). Scalp
block is a method used to relieve pain in the early postoperative period
and to help ensure hemodynamic stabilization in the intraoperative
period [17].
In this study we aimed to investigate the effect of scalp block
performed with bupivacaine in elective craniotomy cases in preventing
hemodynamic response due to incision, and its effect on postoperative
analgesia and the need for analgesics.
Materials and Method
The ethics committee approval was received from the
Clinical Studies Ethics Committee of Samsun Ondokuz Mayis University,
Faculty of Medicine (Approval number B.30.2.ODM.0.20.08/1192). The study
was planned between June/1/2015-December/31/2015. The study was started
after receiving the consents of the patients planned to be included in
the study. 40 patients, who were accepted at the Neurosurgery clinics of
Ordu University Training and Research Hospital and Ordu State Hospital
for elective craniotomy due to intracranial mass, were included in the
study. Our study was a multicenter, randomized, placebo controlled,
double-blind study. 40 patients to undergo elective craniotomy in the
study were between the ages. of 40-85, in ASA II-III groups according to
the risk classification of the American Society of Anesthesiologists
(ASA) defining the physical condition of the patients. All the patients
were informed about the study beforehand, and written consents were
received from the volunteers who accepted to participate in the study.
Those who had a systemic disease under ASA IV risk class, who had
allergy against bupivacaine, advanced stage organ failure, alcohol and
substance addiction and who were below the age of 40 and over the age of
85 were excluded from the study In our study, patients were not
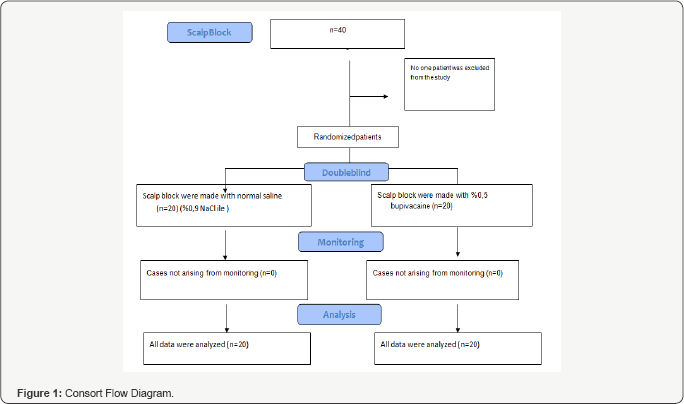
excluded from the study and all data were analyzed. Attached consort
diagram drawn for our scientific work (Figure 1).
The patients were randomized with the sealed envelope
method before the induction into 2 groups each comprising 20 patients;
20ml of 0.5% bupivacaine (Group B) and 20ml of 0.9% normal saline as the
control group (Group S). Preoperative routine monitoring of the
patients was done with Datex-Ohmeda Cardiocap™/5 (GE, Finland) device,
followed by electrocardiogram (ECG), peripheral oxygen saturation (SpO2)
and noninvasive blood pressure monitoring. Before the induction of
anesthesia all the patients were premedicated with 0.05mg/kg of
intravenous midazolam. After the induction of anesthesia with 2-3mg/kg
of intravenous propofol, 2µg/kg of intravenous fentanyl and 0.6mg/kg of
intravenous rocuronium, invasive arterial monitoring was performed by
inserting a 20G intra-arterial cannula into the radial artery.
Anesthesia was maintained with 6mg/kg/h of propofol infusion, 0.15mg/kg
of intravenous rocuronium and 0.25µg/kg/min of continuous intravenous
infusion of remifentanil. The patients were exposed to mechanical
ventilation to reach an EtCO2 level of 30-35 mmHg with an air mixture of 50% O2.
Once the baseline hemodynamic values were recorded before and after the
induction, scalp block was performed. Skull-pin head holder was placed 5
minutes after the block was done. The medication to be used for the
scalp block was prepared in a 20ml syringe by an anesthesiologist, who
would not attend the surgery. 20ml of normal saline was put in the
syringe for Group S. After being numbered according to the results of
randomization, the responsible anesthesiologist made the injections with
a 23G needle on the outer layer of the skull by inserting the needle
into the skin with a 45° angle. Supraorbital and supratrochlear nerves
were blocked by the injection of a 2ml solution on the bilateral
supraorbital notch above the eyebrows. Bilateral auriculotemporal nerves
were blocked by injecting a 2ml solution at 1.5cm anterior to the ear
at tragus level. Bilateral postauricular nerves were blocked by
injecting a 3ml solution at 1.5cm posterior to the ear at tragus level.
Finally; the major, the minor and the third occipital nerves were
blocked by injecting a 3ml solution at the intersection point of the
midsection of the line between protuberentia occipitalis and mastoid
process, and the upper nuchal line. Skull-pin head holder was placed by
the neurosurgeon 5 minutes after the block.
Regarding the systolic blood pressure (SBP),
diastolic blood pressure (DBP), mean arterial blood pressure (MAP),
heart rate (HR), peripheral oxygen saturation (SpO2) and end- tidal carbon dioxide (ETCO2)
of the patients; the time when the patient was taken into the operating
room before the scalp block was accepted as 0 min (= control value).
After the scalp block was done, in the 1st, 5th and 10th minutes and then in the 20th, 30th, 40th, 50th, 60th, and 70th minutes, all the parameters were recorded until the end of the operation with 10-minute intervals.
Postoperative pain was evaluated in patients, who were conscious after the operation, in the 2nd, 4th, 8‘h, 12th, 16th and 24th
hours with a 10cm visual analogue scale (0 is no pain, 10 is the worst
possible pain). It was planned to give 75mg of intravenous diclofenac
sodium to patients with a VAS score above 2 and 75mg of intramuscular
meperidine to patients with a VAS score above 5. Postoperative analgesic
needs and the amount of analgesics used were recorded.
Decrease of SpO2 below 94% for 45 seconds was
accepted as hypoxia and elevation of ETCO above 45mmHg was assessed as
hypercapnia. Hypertension was accepted as an increase of SBP by 20%
above the control value and tachycardia was defined as a heart rate of
at least 20% above the control value, and it was planned to administer
2µg/kg of intravenous fentanyl and to increase the propofol infusion
dose to 9mg/kg/h. It was planned to administer 0.01mg/kg of bolus
intravenous nitroglycerin if SBP and HR were still 20% above the control
values.
Hypotension was accepted as an SBP value of 20% of
the control value and less and 5-10mg of intravenous ephedrine was
planned to be administered. Bradycardia was assessed as 20% below the
control value or a value less than 40beats/ minute, and 0.5mg of
intravenous atropine was planned. 10mg of intravenous metpamid was
planned for the treatment of postoperative nausea and vomiting, and in
the case of blurred vision or tinnitus the plan was to keep the patient
in the recovery room for a longer period of time and observe.
SPSS for Windows 21.0 package program was used for
the statistical analysis of this study. For measurable parameters (age,
weight, amount of remifentanil, duration of anesthesia, duration of
operation) the Kolmogorov-Smirnov test was used in order to identify
whether the distribution was normal or abnormal. For those with normal
distribution, Student t test was employed in independent groups to see
whether there were differences between the groups. Data, such as gender
and ASA, were analyzed with the Chi-square test. Heart rate and MAP data
were assessed with repeated measures analysis of variance. In cases of
differences, the comparison between the groups was done with the
intergroup Posthoc-Scheffe test. Intragroup control values of HR and
MAP, for which it was determined that the time factor was crucial
according to the repeated measures analysis of variance, were compared
by using the Post hoc Bonferroni test. Mann-Whitney U test was employed
for the comparison of postoperative VAS scores between the two groups.
For statistical analyses p<0.05 was accepted as significant.
Results
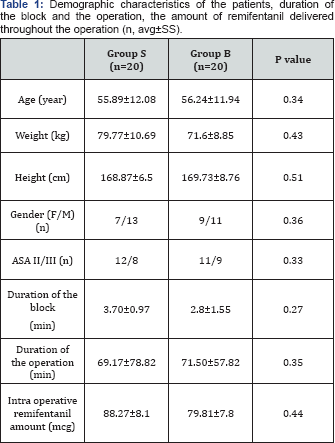
None of the 40 patients in the study was excluded
from the study. The age, body weight, height, gender, ASA classification
of the patients, duration of anesthesia and operation, the total amount
of remifentanil used during the operation were found to be similar. All
the patients were referred to the surgical intensive care units of Ordu
University Training and Research Hospital and Ordu State Hospital
postoperatively (Table 1). Demographic characteristics of the groups did not indicate any statistically significant difference.
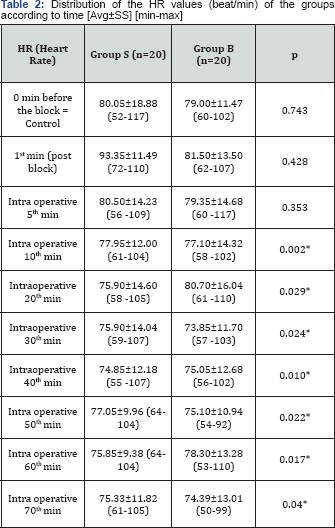
The average values of the heart rate (HR) according to the time of measurement are given in Table 2.
While there was no difference between the groups in the control
measurements in terms of average heart rates, the HR value after
intubation was found to be significantly lower in Group B as compared to
Group S (p<0,05). When the intragroup HR values measured at
different times were compared according to the control value, it was
observed that the average HR values were not statistically different
from the control HR average values in both groups. The average values of
the mean arterial pressure (MAP) according to the measurement times are
given in Table 3.
While there was no significant difference between the groups in terms
of mean arterial pressure values in the control measurements, the MAP
values acquired in the intraoperative 20th and 30th minutes after the
scalp block were found to be significantly lower in Group B compared to
the control group (normal saline group) (p<0,05). When the intragroup
differences were investigated, on the other hand, intraoperative MAP
values measured in the 10th, 20th, 30th, 40th, 50th, 60th, and 70th
minutes after the scalp block in Group B were observed as significantly
lower than the control values (p<0.05).
*p<0.05: in comparison with Group S.
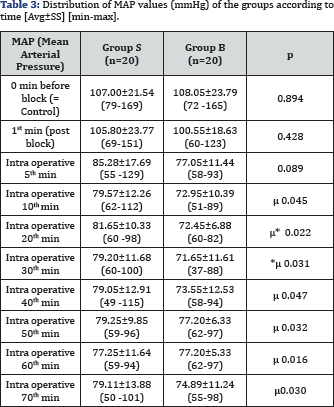
*p<0.05: in comparison with Group S, µ: p<0,05: in comparison with the control measurement values.
**p<0.01: in comparison with Group S
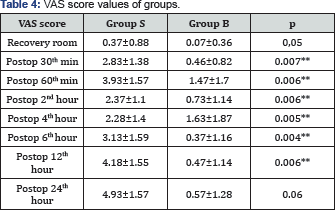
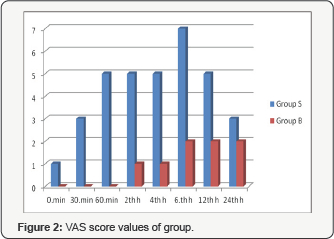
Postoperative pain assessment results of the conscious patients according to the visual analogue scale are given in Table 4 and Figure 2. The VAS scores acquired in the postoperative 30th min, 60th min, 2nd, 4th, 6th and 12th
hours were found quite significantly lower in Group B as compared to
Group S. The values in the recovery room and postoperative 24th
hour were close to the statistical significance level in Group B
(p=0.05 and p=0.06 respectively). No serious complications such as
nausea, vomiting, bradycardia, and hypotension was observed in any of
the patients in the postoperative period. In Group B, except for the
patient, who needed 75mg of diclofenac sodium, no patients required
meperidine. In Group S, on the other hand, 12 patients (60%) required
meperidine in addition to diclofenac sodium particularly in the
postoperative 12th and 24th hours.
Discussion
There is a common belief that those undergo
neurosurgery suffer from minimum postoperative pain and need analgesics.
While it is obvious that this group of patients experience relatively
less pain when compared to those underwent orthopedic surgery or
thoracic surgery, more than 60% of these patients feel moderate to
severe postoperative pain. In a study conducted by Benedittis et al.90%
of the patients suffered from post-craniotomy pain in the first 12
hours, which sometimes extended to 48 hours [18].
Our results overlap with those reported in the study of Benedittis et
al. Likewise, in our study, there were many patients with a VAS score of
5 and above in the control group (normal saline group, Group S)
particularly in the 12th and 24th hours. In a
retrospective study conducted by Quient et al. postoperative pain in
elective craniotomy patients was assessed in the first 24 hours. In the
first 2 postoperative hours, 18% of the patients complained about
severely distressing pain; 37% of the patients had severe, 29% had
medium and 4% had mild pain. Only 12% of the patients did not describe a
post-craniotomy pain in the first 24 hours [19].
Persistent post-craniotomy headache has also been identified and its
incidence increases with postoperative unsuccessful analgesia [20,21]. In a study by Kaur et al. [21]
22 out of 126 supratentorial surgery patients developed persistent
headache. 7 of these cases (5.6%) had headache for a period of longer
than 2 months but shorter than 1 year; 15 cases (11.9%) had headaches
for more than a year in the postoperative period.
In neurosurgery cases, laryngoscopy, skull-pin
applications, interventions to the periosteum and dura cause painful
stimulants. Even in cases with sufficient anesthetic depth, skullpin
application and skin incision lead to acute hypertensive response [2,22].
Following the skull-pin placement, efferent pain sensation generated
from the periosteum results in severe acute hypertensive response due to
sympathetic system activation and eventually, intracranial pressure
increases . This technique, which was defined for the first time by
Pinosky et al. [10]
and had not been implemented in practice before, was compared in a
prospective, randomized, double-blind study in terms of the effect of
scalp block performed by using 0.5% bupivacaine and normal saline on
hemodynamic response to skull-pin placement and on the anesthesia need;
and they were able to show that scalp block was successful in
controlling the hemodynamic response to skull-pin placement. In our
study, we followed the exact description of Pinosky et al. [10]
while performing the scalp block. Lee et al. investigated the effect of
scalp block performed with 0.25% bupivacaine under general anesthesia
on hemodynamics and plasma catecholamine metabolites. 16 elective
craniotomy patients were included in this prospective, randomized,
double-blind study. One group underwent scalp block procedure with
normal saline under general anesthesia induced with isoflurane and 50%
N20-02, while the other group underwent the same procedure with a total
of 20ml of 0.25% bupivacaine. Looking at the heart rate and mean
arterial pressure measurements, it was revealed that scalp block led to
more stable hemodynamics and decreased the need of intravenous or
volatile anesthetics [23]. We used 0.5% bupivacaine and obtained more stable perioperative hemodynamics just as Lee et al. did in their study.
Gazoni et al. [8]
compared perioperative results of the scalp block performed with
ropivacaine in patients, who had supratentorial brain tumor, with
remifentanil. In the prospective, randomized, double-blind study, while
one group received 0.5% ropivacaine during the scalp block procedure,
theother group received remifentanil infusion. Although, it was reported
that scalp block did not bring along significant advantages in terms of
postoperative pain and narcotic analgesics need when compared to
remifentanil infusion, it was observed that hemodynamic parameters (MAP,
HR) were more stable with the scalp block procedure.
Geze et al. compared the effects of scalp block and
local infiltration on hemodynamics and stress response in craniotomy
cases with skull-pin placement. In this prospective, randomized,
placebo-controlled study, one group had scalp block with 0.5%
bupivacaine and another group had local anesthetic infiltration with
0.5% bupivacaine; in the control group, on the hand, in order to prevent
excessive hemodynamic responses, after an IV bolus of 0.5µg/kg
remifentanil or a loading dose of 500µg/kg/ min esmolol, an IV infusion
of esmolol 50µg/kg/min for 4 min was administered. In the study, it is
reported that in the scalp block group, increase in blood pressure and
heart rate due to skull-pin placement was prevented; there was no need
for an additional anesthetic and antihypertensive agent, and blood
pressure and heart rate were more stable when compared to the local
infiltration and the controlgroups. When the groups are compared in
terms of their metabolic and endocrine responses to surgery, stress
response was significantly lowered after skull-pin placement in the
scalp block group in comparison with the control group. In our study, we
also used 0.5% bupivacaine and obtained well-matched results with that
of Geze et al. We also observed perioperative hypertension and
tachycardia in patients included in the normal saline group. 86% of the
patients have pain with somatic features indicating that the source of
pain is pericranial muscles and soft tissue. It is also known that local
anesthetics administered before the skin incision on scalp have
preemptive analgesic effect [24].
Therefore, scalp block is a technique that can be preferred to be used
as a stand-alone analgesic method or to decreasethe dose of analgesics [25]. Taking all these remarks into account, we interviewed our conscious patients in the postoperative 30thmin, 1st, 2nd, 4th, 6th, and 24th
hours on VAS and the use of additional analgesics. Our VAS scores were
significantly lower in the bupivacaine group compared to the normal
saline group.
Ayoub et al. [26]
investigated the efficacy of scalp block in a group of 50 patients
following remifentanil-based anesthesia. In this double-blind study,
anesthesia was induced with 1-3mg/ kg of propofol and 1.0µg/kg of IV
bolus remifentanil; followed by 0.1µg/kg/min of intravenous remifentanil
infusion. The patients were randomized into two groups; one group
having scalp block with bupivacaine or lidocaine and the other group
having 0.1mg/kg intravenous morphine during dural closure at the end of
the surgery. As an additional analgesic agent, codeine was administered
subcutaneously in both groups. Both groups had similar pain scores.
There was no significant difference between the two groups in terms of
the total dose of codeine administered and the first codeine dose. While
there was no difference between the groups in terms of confusion,
nausea and vomiting was higher in the morphine group. The authors
indicated that scalp block offered the same analgesic quality with a
postoperative hemodynamic profile similar to morphine. Scalp block is an
adjuvant method that can be used in order to avoid nausea and vomiting
experienced with opioids [26].
Similarly, Bala et al. performed scalp block in 40 supratentorial
craniotomy patients with bupivacaine or placebo following skin closure
and they used intramuscular diclofenac or intravenous tramadol as
analgesic. Patients without a scalp block had moderate to severe pain
and had more frequent needs of additional analgesics. In this study too,
it was revealed that the pain scores recorded after 6 hours were equal [27].
In our study, on the other hand, we obtained pain-free postoperative
periods of over 12 hours, even extending to 24 hours. Scalp is a highly
vascularized area, there are some studies analyzing the rate of
transmission of local anesthetics applied to this area to the systemic
circulation [7,28].
In our study, bupivacaine was administered very slowly in order to
avoid drug toxicity, as it was required in high volumes in scalp block
procedures and prior to the administration of bupivacaine, needle
aspiration was performed in order to avoid accidental intra-arterial
injection. After making sure that there was no blood, local anesthetic
agent was injected. Although the patients were not monitored for QT
intervals, there was no arrhythmia or asystole observed in routine ECG
monitoring. In the postoperative period, no findings such as blurry
vision, tinnitus or convulsion indicating systemic toxicity were
reported.
Conclusion
In conclusion, in craniotomy cases, scalp block
provides stabilization of hemodynamic responses by decreasing
sympathetic response intraoperatively and helps reduce the early
postoperative pain. Therefore, we believe that scalp block should play a
more important role in anesthesiology practices and should be performed
in all craniotomy patients.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment