Weaning Pattern Characteristics, Based on Simplified Acute Physiology Score 3, of Critically Ill Patients Requiring Ventilator Care-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Background: The Simplified Acute Physiology
Score 3 (SAPS 3) scoring system was developed through a worldwide
prospective study to predict hospital mortality in critically ill
patients. The present study focuses on how outcomes, according to SAPS 3
score, differ in patients receiving or not receiving mechanical
ventilation.
Methods: We retrospectively reviewed
electronic medical records of patients admitted to the surgical or
medical ICU from October to December 2014. The SAPS 3 model scores were
evaluated for all patients, and for subgroups of patients receiving
mechanical ventilation (MV group) or not (Non-MV group). The MV group
was further subdivided into two groups, based on the ventilator weaning
(simple [MV-SW] and others [MV-Others]), to compare patient
characteristics and mortality, based on SAPS 3 scores.
Results: The SAPS 3 score and mortality were
significantly higher, and the length of ICU stay was significantly
longer in the mechanical ventilation group (p = 0.004, p < 0.001, and
p = 0.007, respectively) compared to the non-mechanical ventilation
group. The MV-SW group included patients requiring significantly more
postoperative care, while the MV-Others group had more patients
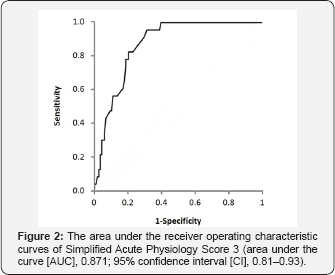
intubated due to hypoxemia (p < 0.001). The AUC value, indicating
discrimination, was 0.871.
Conclusion: The present study, conducted using
the SAPS 3 score, showed good discrimination. It is believed that this
method will be useful in predicting weaning difficulties and mortalities
of patients requiring mechanical ventilation.
Keywords: Intensive care unit; Mechanical ventilation; Mortality; SAPS 3; Ventilator weaningIntroduction
Severity scoring systems are used to predict and
compare outcomes, to help guide the allocation of limited resources and
to evaluate the process of care in intensive care units (ICU). In
critically ill patients, several scoring systems have been developed
over the last three decades [1,2].
The Acute Physiology and Chronic Health Evaluation (APACHE) and the
Simplified Acute Physiology Score (SAPS) are the most widely used
scoring systems in ICUs. Recently, the SAPS 3 was developed through a
worldwide prospective study to predict hospital mortality in critically
ill patients. It is based on 20 different variables, that are easily
measured at patient admission, and dissociating patient status from the
quality of care in the ICU [3-7].
There has, however, been no investigation into how outcomes differ in
patients receiving or not receiving mechanical ventilation.
The aim of this study was to evaluate the
epidemiology and prognostic performance of the SAPS 3 in a retrospective
electric chart review, and to describe the weaning pattern
characteristics of patients receiving mechanical ventilation.
Material and Methods
The study protocol was approved by the institutional review board.
Patient population
All patients admitted to the surgical or medical ICU
from October to December 2014 were included in the present study. In
addition, patients who were admitted to the ICU with serious medical or
surgical postoperative complications were also included. Pediatric
patients (<18 years of age), patients with an ICU stay < 24 h, and
patients who were readmitted after an initial ICU discharge were
excluded.
Data Collection
One individual retrospectively reviewed the
electronic medical records. These records provided all of the data
required to predict the mortality rate using the SAPS 3 model. The SAPS 3
score was obtained from the most severe laboratory findings 1 h before
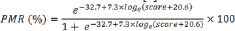
or after ICU admission. Predicted hospital mortality rate (PMR) was
calculated using the following equation; where score means SAPS 3
admission score [6].
The performance of the model was evaluated in all
patients, as well as, in two subgroups of patients who had received
mechanical ventilation (MV group) or not (Non-MV group). Based on the
ventilator weaning pattern, the MV group was further subdivided into two
groups to compare the characteristics and prolonged, or chronic
mechanical ventilation weaning.
Statistical Analysis
Statistical analyses were performed using IBM SPSS
Statistics 21 for Windows. Data were reported as means ± standard
deviation (SD) or medians with 25th and 75th quartiles for continuous
variables, and percentages for quantitative variables. Student's t-test,
chi-squared test, or Fisher's exact test were used depending on whether
the variables were continuous or categorical. P-values less than 0.05
were used to indicate statistical significance. The area under the curve
(AUC) of the receiver operating characteristic (ROC) curve was used to
measure discrimination for hospital mortality.
Results
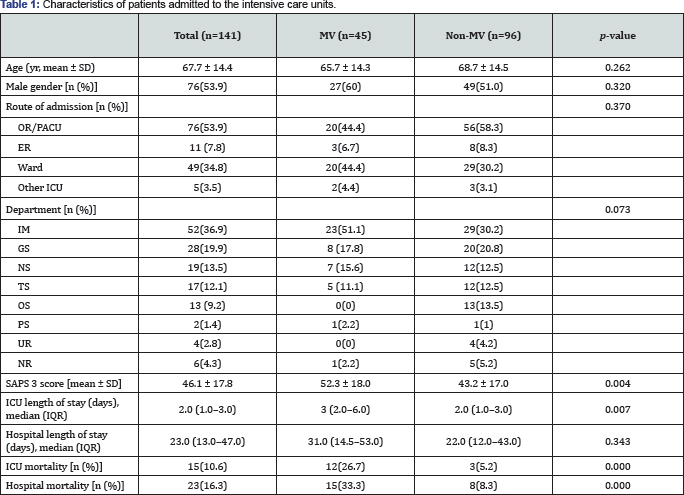
MV: patients who received mechanical ventilation;
Non-MV: patients who did not received mechanical ventilation; OR:
operating room; PACU: postanesthetic unit; eR: emergency room; ICU:
intensive care unit; IM: internal medicine; GS: general surgery; NS:
neurosurgery; TS: Thoracic surgery; OS: orthopedic surgery; PS: plastic
surgery; UR: urosurgery; NR: neurology; SAPS: Simplified Acute
Physiology Score; IQR: Interquartile range.
Of the 154 patients admitted to the ICU between
October and December 2014, 2 pediatric patients, 4 readmissions, and 7
patients with missing data, mostly due to ICU length of stay < 24 h,
were excluded. The study group, therefore, comprised 141 patients: 76
males (53.9%) and mean age 67.7 yr. The characteristics of the study
group are shown in (Table 1).
There were no significant differences in demographic characteristics
between patients in the MV group and the Non-MV group. The SAPS 3 score
and ICU mortality were significantly higher in the MV group (p = 0.004
and p < 0.001, respectively). In addition, length of ICU stay was
significantly longer (p = 0.007) for the MV group.
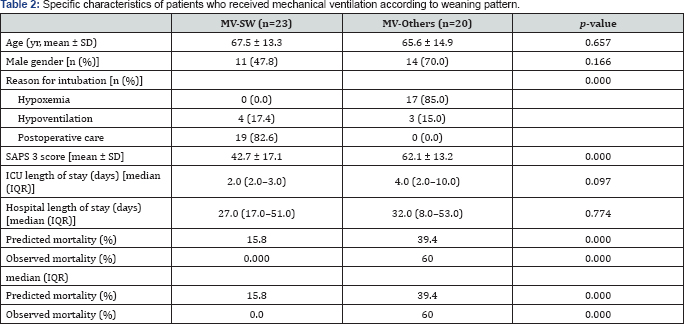
MV-SW: patients who received mechanical ventilation
and simple weaning; MV-Others: patients who received mechanical
ventilation and all other weaning groups; SAPS: Simplified Acute
Physiology Score; IQR: inter-quartile range.
The MV group (n = 43; excluding 2 patients with
missing weaning protocol data) was subdivided based on weaning pattern.
When the reason for the intubation was compared between subgroups, the
MV-SW group included patients requiring significantly more postoperative
care, while the MV-Other group had significantly more intubations due
to hypoxemia (p = 0.001). Observed mortality, SAPS 3 score, and
predicted mortality were significantly higher in the MV-Other group (Table 2), and observed mortality (60.0%) was higher than the predicted mortality (39.4%).
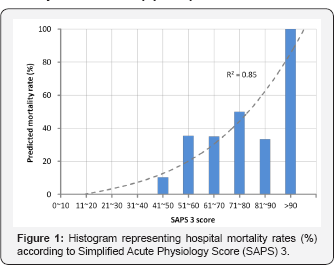
Hospital mortality was considerably greater in
patients with higher SAPS 3 scores. The highest hospital mortality rate
was observed in patients with a SAPS 3 score greater than 90 (Figure 1). Discrimination, as measured by the AUC, was good (AUCs = 0.871), (Figure 2).
Discussion
In the present study, the mean SAPS 3 score of all
patients was 46.1; the score was 10 points higher for the group
requiring mechanical ventilation compared to the group without. Although
there were no significant differences in gender, age, route of
admission, and department between the groups, the group requiring
mechanical ventilation exhibited longer ICU stays and higher mortality.
Among members of the MV group, those capable of simple weaning showed
lower severity scores and mortality.
Many previous studies have shown that SAPS 3 is a scoring system model with good discrimination but poor calibration [5,8-10].
In the present study, the AUC value, which indicates discrimination,
was 0.871; this is similar to previous studies (0.8-0.89) and indicates
favorable discrimination [5,11].
While there were no in-hospital mortalities in patients with SAPS 3
scores of <40 points, patients with scores of 41-90 points had a
mortality rate under 50%, and the mortality rate increased rapidly for
patients with scores >90.
Unlike previous SAPS 3 studies that compared
discrimination or calibration to outcomes from other scoring models or
investigated regional variations [10,12-14],
the present study focused on how outcomes differed in patients
receiving or not receiving mechanical ventilation. This is because,
among various factors affecting SAPS 3, the effect of applying
mechanical ventilation on the score is minimal; however, a significant
number of patients in the ICU receive ventilator care and applying
mechanical ventilation has a clinically significant impact on the
clinical course of critically ill patients.
The patient group requiring mechanical ventilation
was divided into two subgroups based on the weaning pattern. The simple
weaning (MV-SW) group included patients with successful 1st extubation
after the 1st SBT. The other (MV-Other) group included all other weaning
groups: Difficult weaning (failed 1st SBT trial, but succeeded within
the 3rd SBT trials or successful weaning within 7 days after the 1st
SBT); prolonged weaning (failed weaning on the 3rd SBT trial or required
more than 7 days on the 1st SBT); and chronic mechanical ventilation
weaning (the same as tracheostomy) [15,16].
The majority of patients from our hospital had
chronic mechanical ventilation weaning when simple weaning failed; for
this reason, we consolidated the three groups into one. Since most of
the patients who had simple weaning were those who underwent extubation
after maintaining mechanical ventilation for postoperative care due to
old age, prolonged operation time, or underlying diseases (19 subjects,
82.6%), they not only showed lower SAPS 3 scores, but also lower
mortality rates compared to the MV-Other group. Conversely, most ofthe
patients within the MV-Other group were intubated for mechanical
ventilation because of hypoxemia caused by impairment of normal
ventilation function (17 subjects, 85%), which may have manifested as an
increase in the severity of weaning.
The mean length of hospital stay for the MV-Other
group, whose conditions were more severe, was not significantly
different from the MV-SW group; this may be attributed to a shortened
overall length of hospital stay due to the larger number of "do not
resuscitates" (DNRs) and patients who passed away in this group.
Moreover, it can be surmised that the observed mortality rate (60.0%) in
this group was higher than the predicted mortality (39.4%) because of
the influence limited proactive management for patients who were
expected to have unfavorable prognosis and had effectuated DNRs in
advance.
The limitations of this study include having a small
number of participants, which resulted in a low number of patients in
the ventilated group and corresponding subgroups. In addition, at the
time of data collection, the hospital did not have a standard weaning
protocol; weaning was carried out either by applying a T-piece or a
pressure support ventilation (PSV) mode after the SBT and the protocol
used was determined by the doctor in charge of the department.
Consequently, the reason for a patient not having been placed into a
weaning subgroup may not have been due to the patient's condition.
Furthermore, while all charts were reviewed by a
single person responsible for the ICU, the SAPS 3 scores were inputted
by different doctors who were in charge of the department at the time of
admission; for this reason, individual evaluator errors cannot be
eliminated. We plan to perform future studies with a larger number of
patients; furthermore, the hospital plans to implement a standard SBT
protocol, therefore data obtained after the protocol is applied may be
compared to the results presented to allow the mechanical ventilation
subgroups to be more clearly defined to determine any differences.
Conclusion
In conclusion, in the present study, conducted on
patients who were hospitalized in the surgical or internal medicine ICU,
SAPS 3 score assisted-evaluations showed good discrimination. It is
believed that this will be a useful method for predicting weaning
difficulties and mortalities in patients requiring mechanical
ventilation.
Acknowledgement
This work was supported by a research grant from Jeju National University Hospital in 2015.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment