Insulinoma-Anaesthetic Implications with Review of Literature-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Insulinomas are rare tumours that present with
recurrent hypoglycaemic episodes. They are often misdiagnosed or
diagnosis is often delayed due to their bizarre clinical presentation.
Diagnosis of insulinoma is made based on history (Whipple's Triad),
biochemical tests and imaging modalities. Treatment includes medical and
surgical management. We intend to describe the anaesthetic management
of three cases of insulinoma observed over a period of one year and
review the existing literature. Though rare, when they do occur, these
tumours pose a great challenge to anaesthesiologists. Vigilant
monitoring of blood sugars intraoperatively is a must to counteract
these wide swings, hence providing a better patient outcome.
Keywords: Insulinoma; Anaesthetic management; Hypoglycaemia; Whipple's Triad; Intraoperative ultrasound (IOUS)Introduction
Insulinomas are rare tumours with an incidence of 1-4 per million per year [1].
They are the most common functional variety of neuroendocrine tumours
of pancreas. They are usually small (<2cm), solitary and benign
(approximately 90%). Patients present with adrenergic or neuroglycopenic
symptoms due to recurrent hypoglycaemia [1-4].
Weight gain is a common finding in 20-40% and is primarily due to
overfeeding to overcome hypoglycaemia. Diagnosis of insulinoma must be
suspected in otherwise normal patients who present with repeated
episodes of hypoglycaemia and they warrant further investigation [1,2].
Because of the bizarre nature of the presenting symptoms, many patients
will present to neurologists or psychiatrists and hence delay in early
diagnosis or misdiagnosis. Surgical excision is the definite treatment.
Case Series
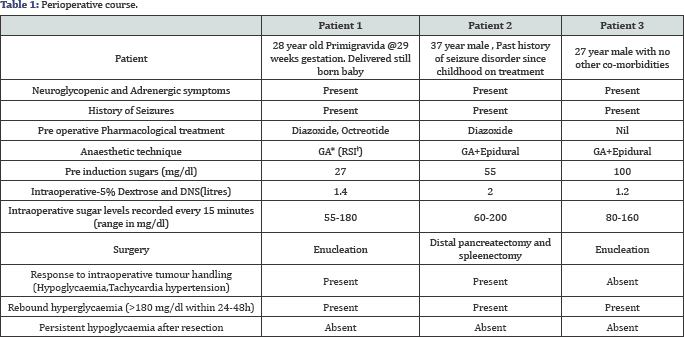
Three young patients; a 28 yr old primigravida@29
weeks gestation, a 37 year old male with past history of seizure
disorder on treatment and a 29 year old male, presented with complaints
of recurrent episodes of drowsiness, excessive sweating, delayed waking
from sleep, seizures and altered sensorium. In view of neurological
symptoms, all three were initially evaluated by neurologists. However,
it was incidentally observed that they had severe hypoglycaemia during
these episodes (GRBS<50mg/ dl). Diagnosis of insulinoma was then made
based on history (Whipple's Triad), biochemical tests and imaging
modalities (Table 1).
Discussion
The median age of presentation is approximately 47 years, with a mild female preponderance (female: male 1.4: 1) [5-7].
Diagnosis of insulinoma is clinical, biochemical and localization of
the tumour. Clinical diagnosis is based on Whipple's Triad which
includes repeated attacks of hypoglycaemia, serum blood glucose levels
<50mg/dl during that period and relief of symptoms with glucose
administration [1,2].
Biochemical diagnosis includes the 72-h fasting test which is
considered as gold standard. During the fasting period, the patient is
allowed to drink calorie-free fluids and physical activity is
encouraged. Blood glucose should be measured 6-hourly till it reduces to
60mg/dL and then every 1 or 2 hours till it reduces to 40-45mg/dL. When
symptoms of hypoglycaemia appear, blood should be sampled and diagnosis
of insulinoma is made when-
- Plasma glucose <55mg/dl during episode of hypoglycaemia,
- Increased serum Insulin (>5-10microU/mL)
- Elevated C-peptide (>200micromol/L) and
- Increased proinsulin level (>25%).5
Localizing insulinomas are difficult with a failure rate of 10-27% [1,5,8].
It includes CT, MRI, Somatostatin receptor scintigraphy. Recently, the
use of Endoscopic Ultrasound is shown to have increased sensitivity.
Intraoperative ultrasound (IOUS) with surgical palpation has a high
success rate (85-90%) [1,5,8].
Treatment includes medical and surgical management. Medical management
includes dietary modification and pharmacological agents. Patient is
advised frequent small meals throughout the day to avoid hypoglycaemia.
Diazoxide is often started in these patients as it decreases release of
insulin by stimulating alpha adrenergic receptors and thereby inhibits
beta cells of islets of pancreas.
Somatostatin analogues like octreotide and lanreotide
is used as they bind to somatostatin receptors on insulinomas and
decrease insulin Secretion [9-11].
Steroid therapy has been considered as it inhibits insulin mediated
glucose uptake and promotes release of glucose. However its value is
doubtful and even considered harmful as it can cause exaggeration of the
normal rebound hyperglycaemia that is seen postoperatively and there is
a high risk of infection. Surgical management includes enucleation
which is the treatment of choice. Some cases may require distal or
partial pancreatectomy.
Anaesthetic implications-Any neurologic damage that
has occurred as a result of previous hypoglycaemic episodes must be
documented. Intravenous infusion of 5% Dextrose or 10% Dextrose should
be started during the fasting period prior to surgery. Aim is to
maintain blood glucose of more than 50mg/ dl [1,5].
Adequate NPO may not be achieved as patients may become symptomatic
even after a few hours of fasting and due to poor patient compliance.
Hence the risk of aspiration must be considered while inducing these
patients and adequate care must be taken.
Administration of anaesthesia for removal of these
tumours is challenging due to difficulty to maintain a normal blood
glucose level. Wide fluctuations in blood glucose levels during tumour
handling are often observed. Hypoglycaemia may be masked under general
anaesthesia because signs of hypoglycaemia such as sweating,
tachycardia, and hypertension and dilated pupils which can also occur
due to hypovolemia, surgical stimuli, lighter surgical planes and drugs.
Hence, detecting hypoglycaemia under anaesthesia is difficult.
Intraoperative hypoglycaemia can cause CNS damage and such patients may
often require postop ventillatory support.
It is recommended that blood glucose level must be
checked before induction and every 15-30 from then on. It is imperative
that glucose levels must be monitored in the recovery period also
because
- Risk of rebound hyperglycaemia after resection
- Multiple adenomas may exist which can cause early postoperative hypoglycaemia which is not seen intraoperative.
Due to frequent blood sampling requirement, an
arterial line is essential. Anaesthetics which decrease cerebral
metabolic rate like propofol or thiopentone should be used. General
anaesthesia with propofol combined with epidural is preferred choice of
anaesthesia for insulinoma excision [1].
Post resection blood sugars may be high because of anti insulin
hormones like GH, glucagon and glucocorticoids, which persist at high
levels for a few days after removal of tumour. This hyperglycaemia is
self limiting. Post op hypoglycaemia however, should raise the suspicion
of either tumour not been found or multiple other insulinomas
persisting.
Conclusion
Though rare, when they do occur, these tumours pose a
great challenge to anaesthesiologists due to inadequate fasting,
preoperative neurologic damage due to repeated hypoglycaemic episodes
and wide swings in sugars during handling of tumour. Vigilant monitoring
of blood sugars intraoperatively is a must to counteract these wide
swings, hence providing a better patient outcome.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment