Labetalol Hypotensive Anesthetic Protocol Paves the Way to Safe Open Abdominal Myomectomy-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Objectives: Evaluating effect of oral
labetalol pre-medication followed by low-dose intraoperative (IO)
labetalol infusion on IO heart rate (HR) and mean arterial pressure
(MAP), blood loss and need for transfusion and urine output (UOP) of
patients undergoing open abdominal myomectomy.
Patient & methods: Eighty-eight patients
were randomly divided into: Study patients received 200 mg oral
labetalol 2-hr before surgery and IO labetalol infusion (0.2mg/kg/hr)
till completion of myomectomy. Control patients received placebo
infusion and all patients received the same anesthetic protocol.
Results: Operative blood loss and transfusion
needs were significantly lower, but UOP was significantly higher in
study than control patients. Oral labetalol significantly decreased
preoperative HR and MAP of study patients compared to their baseline
measures and to control patients. Oral labetalol significantly decreased
HR and MAP elevations after induction and intubation compared to
control patients. Labetolol infusion significantly decreased HR and MAP
till stoppage of infusion compared to other measures and to control
patients. Labetalol infusion allowed stability of HR and MAP with
non-significant difference between measures till stoppage of infusion.
Extubation significantly elevated HR and MAP in control patients, but
non-significantly in study patients. Postoperative (PO), HR and MAP were
significantly lower in study patients compared to baseline measures and
to PO measures in control patients. PO hemoglobin concentration was
significantly lower in all patients than preoperative concentrations,
but concentration deficit was significantly lower in study than control
patients.
Conclusion: The applied protocol of labetalol hypotensive anesthesia improved anesthetic and surgical outcome of myomectomy.
Keywords: Labetalol; Hypotensive anesthesia; MyomectomyAbbreviations: IO: Intraoperative; PO: Postoperative; MAP: Mean Arterial Pressure; OAM: Open Abdominal Myomectomy; SNP: Sodium Nitroprusside
Introduction
Myomectomy is the gold standard uterine-sparing surgery for symptomatizing uterine fibroid [1], but intraoperative (IO) bleeding is still a challenge [2]. Hypotensive anesthesia allowed significant decrease of blood loss without compromising vital organ perfusion [3] and subsequently reduces transfusion requirements and minimizes allogenic transfusions risks [4]. Labetalol is a combined β- and α1 adrenoceptors antagonist [5]. Oral labetalol is readily absorbed in man [6]. Peak plasma level was achieved after 2.5-minute and 20-120 minutes after intravenous and oral administration, respectively [7], peak effect within 1-4hr after oral intake [8] and elimination half-life of 5 to 8 hours [6].
Hypothesis
Pre-anesthetic medication with oral labetalol
followed by low- dose IO labetalol infusion can improve anesthetic and
surgical outcome of open abdominal myomectomy (OAM).
Objectives: Evaluation of effect of the
proposed hypotensive protocol on IO heart rate (HR) and mean arterial
pressure (MAP), blood loss and need for transfusion and tissue perfusion
judged by urine output (UOP) of patients undergoing OAM.
Design: Prospective comparative study.
Setting: University and Insurance hospitals, Tanta and Benha, Egypt.
Patient & Methods
This study was conducted since Oct 2014 till Nov
2016. Study protocol was approved by the Local Ethical Committee. Women
assigned for myomectomy and signed written fully informed consent were
included in the study. Exclusion criteria included presence of multiple
myomas necessitating hysterectomy, gynecological malignancy, cardiac
diseases or history of coagulopathy. Clinical evaluations entail
collection of demographic data, complete gynecological and
ultrasonographic examinations and routine laboratory investigations.
Women with hemoglobin concentration of≤7gm/dl received preoperative
blood transfusion to adjusted Hb. Conc. of ≥8gm/dl.
Patients fulfilling the inclusion criteria were
randomly, using sealed envelops prepared by blinded anesthetic
assistant, allocated into two equal study groups according to the
applied anesthetic procedure; Study patients followed the hypotensive
protocol and control patients received normotensive anesthesia.
Preparation of labetalol infusion
Labetalol infusion was prepared by mixing 4ml
labetalol (Trandate injection, Aspen Pharmacare, South Africa, 5mg/ml)
in 500cc physiological saline to provide a concentration of 0.04mg/ ml
saline. Infusion rate was adjusted at 6ml/min, to provide the patient by
0.24mg/min, i.e., 14.4mg/hr and if the patient weighs 70kg body weight
so the dose received will be 0.206mg/kg/hr [9]. Labetalol infusion rate was adjusted to provide a target MAP of 55- 60mmHg [10] but not exceeding the recommended safe maximal dose of 300mg on occasion of infusion [11].
Plain saline infusion was prepared as placebo for control patients. An
assistant, not included in the study, was responsible for infusion
preparations and distribution between patients and adjustment of rates.
Hypotensive protocol
Baseline HR and MAP were non-invasively determined,
then study patients received 200mg oral labetalol (Trandate, Aspen
Pharmacare, South Africa, 100mg tablets), while control patients
received a placebo tablet two hours prior to surgery. HR and MAP were
determined preoperatively, after induction of anesthesia and after
tracheal intubation. Then, labetalol and placebo infusions were started
till myomectomy was completed and then were stopped to allow restoration
of blood pressure to achieve perfect hemostasis.
Anesthetic Procedure
Patients of control group were premedicated by
midazolam 0.02mg/kg. Anesthesia was induced, in groups, using propofol
2mg/kg, fentanyl 1-2ug/kg, and rocuronium 0.6mg/kg, and was continued
with sevoflurane, fentanyl and rocuronium. After tracheal intubation,
the lungs were ventilated with 100% O2 in air using a semi-closed circle system for a tidal volume of 6-8 ml/ kg, and end-tidal carbon dioxide (paCO2) of 32-35mmHg. Patients were continuously non-invasively monitored for MAP and HR.
Study outcome
Primary outcome included
- Effect of oral labetalol pre-medication on HR and MAP determined after induction and tracheal intubation.
- Effect of labetalol infusion on intraoperative HR and MAP estimated every 10 minutes till end of surgery and at time of infusion stoppage.
Secondary outcome included
- IO blood loss, frequency of blood transfusion
- Amount of intraoperative UOP.
- Hemoglobin concentration (Hb. Conc.) estimated immediately after surgery and concentration deficit in relation to preoperative concentration.
Statistical Analysis
Sample size was calculated using the standard nomogram proposed by Kraemer & Thiemann [12]
and a sample size of ≥40 patients per group was determined to be
sufficient to detect a difference at the 5% significance level and give
the trial 80% power. Results were analyzed using paired t test, one-way
ANOVA with post-hoc Tukey HSD Test and Chi-square test (X2
test). Statistical analysis was conducted using the SPSS (Version 15,
2006) for Windows statistical package. P value<0.05 was considered
significant.
Results
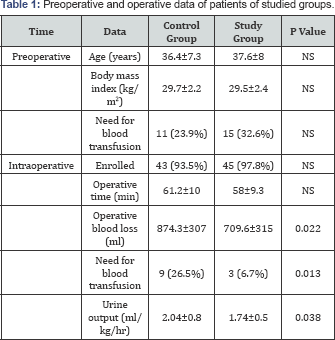
Data are presented as mean±SD, numbers, percentages; P
value indicates difference between both groups; NS: Non-significant,
p<0.05: significant difference
The study included 92 patients, 26 patients (28.3%)
required preoperative blood transfusion for correction of anemia and 4
patients were excluded during surgery. Mean operative blood loss and
need for transfusion were significantly lower, but intraoperative UOP
was significantly higher in patients of study group. Pre- and
intraoperative data are shown in Table 1.
Oral labetalol significantly decreased preoperative HR and MAP of
patients of study group compared to their baseline measures and to
preoperative measures of control patients. Induction of anesthesia and
tracheal intubation significantly increased HR and MAP compared to
baseline and preoperative measures in both groups. However, oral
labetalol significantly decreased these elevations compared estimates of
control patients.
IO labetolol infusion significantly decreased HR and
MAP till stoppage of infusion in comparison to other measures and to
measures of patients of control group. Moreover, labetalol infusion
allowed stability of HR and MAP with non-significant difference between
measures at 10-, 20-, 30-, 40-min
after start of infusion and at time of stoppage of infusion. Extubation
significantly elevated HR and MAP in comparison to other IO
measurements in control group, while the difference was non-significant
in patients of study group. At 1-hr and 2-hr
postoperative (PO), mean HR and MAP levels showed non-significant
difference versus baseline and preoperative measures in control group,
while were significantly lower compared to baseline measures in patients
of study group and to PO measures in patients of control group (Table 2).
Postoperative Hb. Conc. was significantly lower in patients of both
groups compared to preoperative concentration, but was non-significantly
lower in patients of control group than study group. On contrary,
concentration deficit was significantly lower in patients of study group
compared to control group (Table 3).

*: Significant difference versus control group; f:
Significant difference versus baseline measures; f: significant
difference versus preoperative measures; fl: Significant difference
versus after induction estimates; #: Significant difference versus after
tracheal intubation estimates; $: Significant difference versus after
extubation estimates.
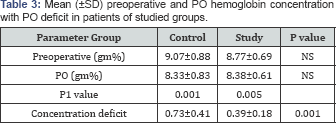
P value indicates difference between both groups; P1
value indicates difference between preoperative and PO measures; NS:
Nonsignificant, p<0.05: significant difference.
Discussion
Oral labetalol pre-medication significantly lowered
preoperative HR and MAP in study patients and allowed blunting of the
pressor reflexes associated with induction of anesthesia and tracheal
intubation than in control patients. These findings spot light on the
possibility for using oral labetalol as a preanesthetic medication and
go in hand with Ryu et al. [13]
who found labetalol injection either before or after laryngoscopy and
tracheal intubation was associated with lower incidence of tachycardia
and less increase in rate-pressure product. Also, Meftahuzzaman et al. [14]
detected significantly minimal increase in HR and MAP in patients
received bolus dose of labetalol or fentanyl prior to tracheal
intubation compared to control patients with significant difference in
favor of labetalol and concluded that labetalol is better agent for
attenuation of laryngoscopic and intubation reflex than fentanyl.
Recently, El-Shmaa & El-Baradey [15]
reported significant decrease in HR and MAP with labetalol and
dexmedetomidine than with saline in response to laryngoscopy and
intubation and Sharma et al. [16]
found both labetalol and nifedipine were effective for control of
persistent postpartum hypertension, but labetalol achieved control
significantly more often with the starting dose and had fewer side
effects. In support of the use of oral β-blockers for preoperative
preparation whenever deliberate hypotension is required, Apipan &
Rummasak [17], Amr & Amin [18,19] and Kim et al. [20]
reported that premedication with oral propranolol, oral atenolol or
oral enalapril before hypotensive anesthesia effectively reduced heart
rate, amount of blood loss, and blood transfused with better quality of
surgical field.
Labetalol infusion allowed proper hemodynamic control
throughout operative time manifested as significantly lower MAP with
subsequent significant reduction of operative field bleeding,
transfusion requirement and significantly lower hemoglobin deficit
compared control patients. These results coincided with previous work
documented that hypotensive anesthesia reduced IO blood loss and
improved the quality of the surgical field [21-]. In line with the use of labetalol infusion for maintenance of low IO blood pressure, Hadavi et al. [24]
detected a little difference between labetalol and nitroglycerine on IO
blood loss and surgical field quality in rhinoplasty surgery and Jeong
et al. [25]
found sevoflurane plus a "supportive" agent either; esmolol, labetalol,
metoprolol, nicardipine, and dexmedetomidine may offer significant
advantage of reducing patients' MAP than sevoflurane alone during
orthognathic surgery.
The reported non-significant differences between IO
measurements of MAP throughout operative time assured the proper control
of labetalol infusion on blood pressure during surgical manipulation.
In support of this finding, Chung et al. [26]
demonstrated that labetalol pretreatment (1.2mg/kg) with supplemental
intravenous sodium nitroprusside (SNP) provides more favorable blood
pressure control during surgical resection of pheochromocytoma than with
SNP alone.
Moreover, immediate and 2-hr PO MAP measures in study
patients were significantly lower compared to baseline measures and to
PO pressure in control patients. These data indicated that labetalol
allowed proper emergence from anesthesia that was maintained
postoperatively. These findings go in hand with Ryu et al. [13]
who found time to return to normotension after the loading dose was
longer with labetalol than nicardipine & Mashour et al. [27]
also found the use of IO esmolol or labetalol is not associated with
stroke after non-cardiac surgery, while metoprolol was associated with a
3.3-fold increase in perioperative stroke. Moreover, Sanath Kumar et
al. [28]
presented four cases of phaeochromocytoma prepared with oral labetalol
and reported rare intraoperative surges in blood pressure during tumor
manipulation and all patients had an uneventful PO recovery.
Sirivanasandha et al. [29]
documented that labetalol is a good alternative drug to control
hypertensive response during emergence from anesthesia for
post-craniotomy.
Conclusion
The applied protocol of oral labetalol pre-medication
and low- dose IO labetalol infusion as a modality for hypotensive
anesthesia improved anesthetic and surgical outcome of myomectomy.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment