Thromboelastography and Thromboelastometry in Patients with Sepsis - A Mini-Review-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Introduction
Coagulopathy is a common finding in patients with sepsis and is considered to be a risk factor for mortality [1].
Mechanisms like imbalance between coagulation and fibrinolysis have
been attributed to coagulopathy in sepsis. The spectrum of coagulopathy
can range from a hypercoagulable state to a hypocoagulable state [2].
Conventional coagulation assays (CCAs) like prothrombin time (PT) and
activated partial thromboplastin time (aPTT) are routinely done to
assess coagulation status in patients with sepsis. However, these
coagulation tests have certain inherent limitations associated with them
[3].
These limitations include their inability to detect hypercoagulable
state and also cannot assess the fibrinolytic system. Rotational
thromboelastography (TEG) and thromboelastometry (ROTEM) evaluate whole
clot formation and can be useful point-of-care tests [3].
There is ongoing research to establish the efficacy of TEG/ROTEM over
conventional coagulation tests in detection of hypo- or hypercoagulable
states in sepsis and in guiding transfusion practices [4].
Basic principles of conventional thromboelastography (TEG®) and thromboelastometry (ROTEM®): [3,4].
The basic principle of functioning is similar in both
thromboelastography (TEG®) and thromboelastometry (ROTEM®) with only
subtle differences. Rotational thromboelastograph (TEG®) analyzer has a
pin and an oscillating cup. However, in thromboelastometry (ROTEM®), the
pin rotates and the cup remains fixed. Once blood begins to clot,
fibrin strands are formed which influence the movement between the cup
and the pin. This process is detected electromechanically and finally
presented as a computerized tracing known as the thromboelastograph.
Thromboelastograph is a waveform which depicts certain parameters that
reflect different phases of the clotting process. These parameters are
mentioned below:
An overview of TEG/ ROTEM with terminologies is presented below
A. Clot formation
Reaction time (R): R time represents the time of
latency from start of test to the first evidence of clot or initial
fibrin (or time taken for clot to achieve an amplitude of 2 mm) and it
correlates with the level of clotting factors. In ROTEM®, R time is
represented by clotting time (CT).
B. Clot kinetics
K time: K time is a measure of clot strength and it
reflects the time taken for clot to reach an amplitude of 20 mm from the
start of clot formation. It is recorded from the end of R time. In
ROTEM®, K time is represented by clot formation time (CFT).
α angle: α angle is the angle along horizontal axis
of thromboelastograph and it measures the speed at which fibrin build up
and cross linking takes place. Hence, it assesses the rate of clot
formation. a angle is the common terminology for this angle in both
conventional thromboelastography (TEG®) and thromboelastometry (ROTEM®).
Either K time (or CFT) and a angle correlate with fibrinogen levels
i. Clot strength
Maximum amplitude (MA): MA measures the ultimate
strength of fibrin clot and correlates with the level of platelets. In
ROTEM ®, MA is represented by maximum clot firmness (MCF).
ii. Coagulation index (CI)
CI is calculated by a complex mathematical formula
calculated from R, K, α and MA and has a normal reference range between
-3 to 3. It is an overall indicator of coagulation and represents
hypocoagulable (CI<-3), normocoagulable (CI -3 to 3) or
hypercoagulable states (CI >3).
iii. Clot lysis (Fibrinolysis)
A30: A30 is the amplitude at 30 minutes post-MA (in both conventional thromboelastography and thromboelastometry).
Lysis index (CL 30%): CL 30 indicates the percentage
decrease in amplitude 30 minutes post-MA. LY 30% represents the lysis
index in thromboelastometry.
Estimated platelet lysis (EPL %): EPL is the computer
prediction of diminution of amplitude 30 seconds post-MA and it is the
earliest indicator of abnormal clot lysis (in bothconventional
thromboelastography and thromboelastometry).
Hypocoagulability is defined as increased CT/R and CFT/K times and/or decreased MCF/MA and alpha angle.
Hypercoagulability is defined as decreased reaction
times (CT/R and CFT/K times) and increased clot formation (increased
alpha angle or high maximal amplitude (MCF/MA).
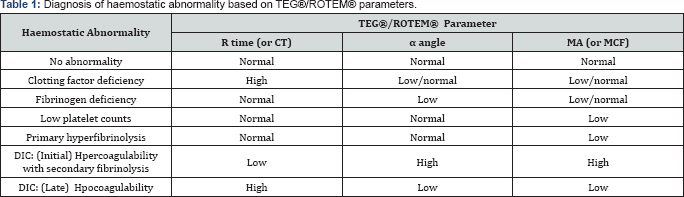
The thromboelastograph parameters are also useful in
the diagnosis and management of hypocoagulability and
hypercoagulability, identification of primary and secondary
hyperfibrinolysis and differentiating between medical and surgical
causes of bleeding (Table 1).
Studies on the ability of ROTEM® and TEG® to detect sepsis-induced coagulopathy or disseminated intravascular coagulation (DIC)
Results of TEG®/ROTEM® in sepsis have varied widely
across the studies. Some patients have shown distinct hypocoagulabilty
while others have shown a predominant hypercoagulable pattern. There are
several reasons to explain this lack of uniformity in test results. The
timing of measurement has varied widely in the studies. The initial
phase of sepsis is characterized by formation of microvascular thrombi
and the later phase manifests as a hypocoagulant phase secondary to
consumptive caogulopathy. So, the timing of measurement has a bearing on
test results. This heterogeneity can also be explained by the
difference in disease severity of study population. Interestingly, there
is no universally validated reference value and definition of
hypocoagulability and hypercoagulability of ROTEM®/TEG® in the available
studies. Overall, if sepsis- induced coagulopathy was present,
ROTEM®/TEG® could detect it in 43-100% patients.
Some of these studies are mentioned below
- Sivula and co-workers in 2009 assessed the role of thromboelastometry (ROTEM®) in severe sepsis and investigated its applicability in diagnosing sepsis-induced coagulopathy. They studied 28 patients with severe sepsis, out of which 12 patients fulfilled the criteria of overt DIC on admission. A total of 10 healthy persons were taken as controls. MCF, CFT and alpha angle values differed significantly between patients with overt DIC, severe sepsis without DIC and healthy controls respectively (MCF 52, 68 and 63 mm, CFT 184, 73 and 88 sec and alpha angle 58, 76 and 72 degrees respectively). There was a trend towards hypercoagulability in patients with severe sepsis without DIC and a trend towards hypocoagulability in those with overt DIC. They concluded that thromboelastometry can easily demonstrate the coagulation capacity of patients with sepsis [5].
- In 2011, Cortegiani and co-workers studied 31 patients with severe sepsis (within 12 hours of diagnosis of severe sepsis) and compared them with 31 postoperative patients by using TEG®. R time, K time, MA, lysis index, and coagulation index were similar between these groups but a angle was significantly lower in the severe sepsis group indicating hypocoagulability in those patients [6].
- Kilic and co-workers in 2014 studied 21 patients with SIRS-sepsis and compared them with 34 patients (without SIRS-sepsis). Blood samples were withdrawn on admission and on day 3 of ICU stay for TEG® analysis. In patients with SIRS-sepsis, hypercoagulability was observed in the form of a significantly higher a angle and lower K value as compared to the control group. They concluded that TEG® can be a useful tool for diagnosing coagulation abnormalities in sepsis [7].
- Additional value of ROTEM® and TEG® in diagnosing coagulation abnormalities as compared to CCAs:
- Luckner and co-workers in 2008 studied a case series of patients with severe sepsis and septic shock who were planned for emergency laparotomy. All patients had significantly prolonged coagulation times with a putatively increased risk of bleeding as per the routine coagulation assays. On the contrary, ROTEM® revealed normal clotting times and even signs of hypercoagulability in these patients (unlike CCAs) and surgery could be performed with minimal blood loss and no transfusions [9].
- Involvement of fibrinolytic system can also be detected by TEG® and ROTEM® (unlike CCAs). Adamzik and coworkers in 2010 studied 56 patients with severe sepsis and compared them with 52 postoperative patients (controls). Blood sampling for thromboelastometry (ROTEM®) was done within 24 hrs of diagnosis of severe sepsis and immediately after surgery in postoperative patients. CRP, procalcitonin (PCT), IL-1 levels, SAPS II and SOFA scores were simultaneously analyzed. ROTEM® parameters like CT, CFT, a angle and MCF were similar between these groups but lysis index was significantly increased indicating an early involvement of fibrinolysis in patients with severe sepsis [10].
Collins and co-workers investigated 38 patients with
severe sepsis by performing global tests of haemostasis and compared
them with 32 controls. They found that although patients with severe
sepsis had a delayed activation of haemostasis but once initiated,
thrombin generation and clot formation were normal or even enhanced in
this group. Routine coagulation assays, which measure only the
initiation of clotting process and not its propagation, poorly evaluate
the coagulation capacity of such patients [8].
Role of ROTEM® and TEG® for anticoagulant treatment in sepsis
There are only few studies attending to this area with very small series of patients [11].
Role of ROTEM® and TEG® in prediction of outcome in sepsis
Hypocoagulability has been found to be an independent predector of poor outcome in some studies as mentioned below:
- Daudel and co-workers in 2009 studied 30 patients with sepsis. Routine clotting tests and thromboelastometry (ROTEM®) were done every 12 hrs during first 48 hrs of admission, and finally at discharge from ICU. It was observed that patients with more severe organ failure (SOFA>10) had higher CFT (125±76 sec vs 69±27 sec) and lower MCF (57±11 mm vs 69±27 mm) as compared to those with less severe organ failure (SOFA<10). The values changed significantly with the intensity of sepsis. Improved organ dysfunction upon discharge from ICU was associated with shortened coagulation time, accelerated clot formation and increased firmness of blood clot [12].
- Adamzik and co-workers in 2011 performed a study in 98 patients with severe sepsis to investigate the role of thromboelastometry (ROTEM®) as a potential predictor of 30-day survival in severe sepsis and compared ROTEM® with simplified acute physiology II (SAPS II) and SOFA scores. CT, CFT, a angle, MCF and SAPS II and SOFA scores were recorded on the day of diagnosis of sepsis. Mean CFT was significantly prolonged (276 ± 194 sec vs. 194 ± 109 sec) and both MCF (52.7 ± 12.1 mm vs. 57.3 ± 11.5 mm) and a angle (53.4 ± 12.8 degrees vs. 58.9 ± 11.8 degrees, P = 0.028) were significantly reduced in non-survivors. SAPS II and SOFA scores were not different between survivors and non-survivors [13].
- Ostrowsky and co-workers in 2013 studied 50 patients with severe sepsis. Patients were divided into 3 groups on the basis of MA value of TEG® on admission: hypocoagulable MA, normocoagulable MA or hypercoagulable MA. Patients progressing to hypocoagulability had higher SOFA and DIC scores and they also showed a higher early mortality [14].
Conclusion
In summary, both thomboelastography (TEG®) and
thromboelastometry (ROTEM®) seem to have a promising role in the
evaluation of coagulation abnormalities in sepsis. But the available
studies in sepsis show heterogeneous results and are of limited quality [4].
TEG/ROTEM measurements in sepsis can show both hypo-
and hypercoagulability. Hypercoagulability is seen more in acute phase
of sepsis. Timing can influence the results because sepsis is a dynamic
process. Sequential measurements of TEG/ ROTEM can enlighten us more
about coagulation derangements associated with sepsis. The current
evidence is limited due to heterogeneity, small sample size, lack of
standardized definitions for hypo- and hypercoagulable states. Larger
trials can establish the utility of TEG/ROTEM to detect coagulation
abnormalities to diagnose DIC and to guide transfusion therapy.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment