Ultrasound Guided Serratus Plane Block for Post-Mastectomy Pain Syndrome after Mastectomy with Axillary Node Dissection-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Introduction
Breast cancer is the most common cancer among women
of all races. In 2017, it’s estimated that 127 new cases per 100,000
women will be diagnosed in the United States alone [1]. Thirty-six
percent of those diagnosed with stage I or II breast cancer undergo
mastectomy and 72% of those diagnosed with stage III will [2].
Breast cancer treatment besides surgical procedures
includes adjuvant radiation treatment, chemotherapy, and endocrine
therapy, all of which carry an increased risk of postoperative pain.
Post-mastectomy pain is common and can be difficult to manage.
Studies estimate that Post-Mastectomy Pain Syndrome
PMPS develops in about 25% to 60% of women [3], leading to disability,
psychological distress, and diminished quality of life. There is no
standardized definition for PMPS it has been described as a type of
neuropathic pain, a complex chronic pain state commonly associated with
nerve fiber injury [4-5]. Pain is typically localized to the
anterior/lateral chest wall, maxilla, and/or medial upper arm and
persists more than 3 months after surgery when all other causes of pain
have been excluded [6]. Post-mastectomy pain is characterized by the
classic features of neuropathic pain such as burning, tingling,
shooting, stinging, or stabbing pains, and hyperesthesia.
A recent systematic review of the literature [7]
found that non-interventional and interventional treatments have been
proposed for PMPS, but that the majority of the studies lacked
descriptive information and clear reports of statistical tests.
Though the review did not evaluate studies on the use
of regional analgesia, the Serratus Plane Block (SPB) is gaining
popularity for treating (PMPS).
Case One
A 71-year-old woman with moderate hypertension,
well-controlled non-insulin-dependent diabetes mellitus, and a history
of left breast lumpectomy, underwent left mastectomy with axillary node
clearance under general anesthesia with postoperative infiltration of
the surgical wound by the surgeon at the end of the operation.
During the postoperative period she reported mild,
mainly axillary pain rated from 2 to 4 on an 11-point numerical rating
scale (NRS) for pain. She was treated with non steroidal
anti-inflammatory drugs (NSAIDs) and tramadol. Fifteen days after
discharge from the hospital, she was referred to a pain clinic because
of axillary pain with multiple daily exacerbations and dysesthesia in
the left axilla. Initial treatment with oral NSAIDs, pregabalin,
tramadol daily with oral administration of morphine sulphate (Oramorph®)
for breakthrough pain was unsuccessful.
The pain gradually worsened, causing physical limitation and
anxiety. Radiographic studies were unremarkable. The pain
severity increased to 8-9 as measured on the NRS and was
described as burning and shooting pain. In discussions with the
patient, we proposed an ultrasound-guided, single shot deep SPB
as done with the technique described in our previous report [8].
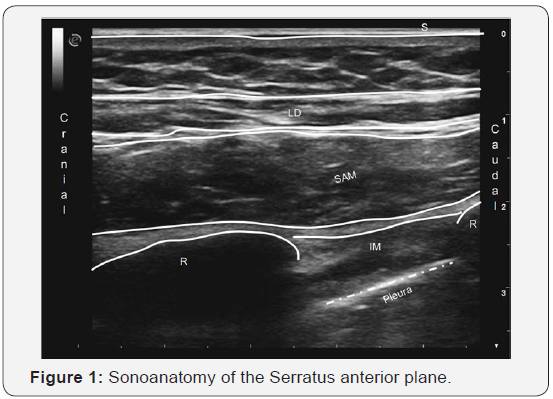
The left arm was gently abducted, a linear ultrasound probe
(high frequency linear probe connected to MyLabTM Alpha,
Esaote, Genova, Italy), was placed in the sagittal plane over the
midclavicular region of the left chest wall. The ribs were counted;
the fifth was identified and followed laterally towards the
midaxillary line, and the site was then marked. The right side of the
chest was prepared by disinfecting the skin with a chlorhexidine
0.5% in alcohol 70% antiseptic, and a sterile cover was applied
over the probe. With the patient in supine position, the ultrasound
probe was placed along the midaxillary line on the landmark at
the level of the fifth rib. In this way, we were able to identify, from
the surface inwards, the latissimus dorsi, the serratus anterior
muscle, the ribs, and the pleura.
At the caudal extremity of the probe, the skin entry point
and subcutaneous tissues were anesthetized with 4 mL of
1% lignocaine. Under real-time ultrasound guidance, a 50mm
22-gauge needle (Pajunk, Geisingen, Germany), was positioned
with an in-plane technique in caudocranial direction between
the surface of the rib and the serratus anterior muscle (Figure 1)
and a total of 10mL of LA (7mL of ropivacaine 0.25% + 3 mL of
lignocaine 1%) plus dexamethasone 4 mg were then injected. Ten
minutes later, the NRS score decreased from 10 to 1 the patient
was able to move her left upper arm without major limitation she
was discharged home and instructed to continue with pregabalin
therapy. Fifteen days later, the patient reported experiencing
recurrence of pain (NRS score 5to7). A second SPB was performed
as described previously. Three months after this last block she
remains pain free and is able to carry out daily physical activities
without major limitations.
Case Two
A 43-year-old woman in otherwise good health underwent left
mastectomy with skin expander implantation plus axillary node
dissection under general anesthesia plus pectoral nerves (PECS
I+II) block. Starting the second postoperative day, she reporteed
moderate pain (NRS score of 5) iv morphine and NSAIDs were
administered, and the pain regressed. She was discharged with a
prescription of acetaminophen if needed.
Four months later, she was readmitted because of intense
left thoracic pain. Radiographic studies were normal. Ten
minutes after the SPB was performed (as described above), the
pain severity was rated as 2 on the NRS. She was discharged
with a prescription for pregabalin 75 mg twice a day + tramadol
200 mg/die. At the follow-up visits planned at 15 and 40 days
postoperative, two SPBs were performed because of pain rated as
6 and 4, respectively, on the NRS. Oral therapy was continued. At
6 months after the first (SPB), the pain was rated 1 on the (NRS),
without causing any limitation of physical activity.
Discussion
The serratus anterior is a broad flattened sheet of muscle
originating from the first nine ribs and passes posteriorly around
the thoracic wall before inserting into the costal surface of the
medial border of the scapula [9] Blanco first described [10] and
identified the serratus plane as a potential space in which the
branches of the intercostals nerves run within two potential
spaces, one superficial and one deep to the serratus anterior
muscle itself.
Since then, SPB has been used mainly for postoperative
analgesia in ipsilateral thorax [11] more recently for posttraumatic
pain relief [8] and for (PMPS) in a few cases [12].
The serratus muscle is superficial, so his ultrasound
identification, essential for the (SPB), is relatively easy. No major
complications have been reported in the literature; continuous
visualization of the pleura and accurate control of needle
trajectory/tip are essential to minimize the risk of potentially
serious complications.
Conclusion
These two cases demonstrate the efficacy of ultrasoundguided
deep (SPB) as a multimodal treatment for patients with
(PMPS). Although this technique holds promise, further studies
are needed to assess the real efficacy, potential adverse effects,
and complications of (SPB) for (PMPS).
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment