A Retrospective Study Evaluating the Efficacy of Identification and Management of Sepsis at a Western Cape Province District Level Hospital Internal Medicine Department, in Comparison to the Guidelines Stipulated in the Surviving Sepsis Campaign 2012-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Background: Currently there is little data on
identification, management and outcomes of patients with sepsis in
developing countries. Simple cost effective measures such as accurate
identification of patients with sepsis and early antibiotic
administration are achievable targets that are within reach without
having to make use of unsustainable protocols constructed by developed
countries.
Aim: The aim of our study is to assess the
efficacy of clinicians at a district level hospital in the Western Cape
at identifying and managing sepsis. Furthermore we will assess the
outcome of patients in terms of in-hospital mortality and length of
hospital stay given the above management.
Methods: A retrospective study design was
applied when analyzing data from the routine burden of disease audit
done on a 3 monthly basis at Karl Bremer Hospital.
Results: The total sample size obtained was 70
patients. A total of 18/70 (26%) patients had an initial triage blood
pressure indicative of sepsis induced hypotension however only 1/18
(5.5%) of these patients received an initial crystalloid fluid bolus of
30ml/kg. The median time for antibiotic administration in septic shock
was 4.65 hours. Further a positive delay in antibiotic administration (p
value= 0.0039) was demonstrated. The data showed 8/12 (66%) of patients
with septic shock received inappropriate amounts of fluids. The
in-hospital mortality for sepsis was found to be 4/24 (17%), for severe
sepsis 11/34 (32%) and a staggering 9/12(75%) for septic shock.
Conclusion: The outcomes of the study
concluded that the initial classification process and management of
sepsis by our clinicians is flawed. This inevitably leads to an increase
in in-hospital mortality.
Background
Sepsis, as defined by the Surviving Sepsis Campaign 2012(SCC) [1]
is the presence of a probable or documented infection together with
systemic manifestations of an infection. In 2004 the World Health
Organization (WHO) [2]
listed three infective causes namely lower respiratory tract infection,
diarrheal disease and tuberculosis on their top 10 list for causes of
death, which is similar to mortality reports documented in the 2013
Western Cape mortality profile [3].
Thus highlighting sepsis and its squeal; which ultimately is caused by
an infection as major contributors to the local and global burden of
disease?
To date there is virtually no accurate data on
incidence, prevalence or mortality rates for sepsis, severe sepsis and
septic shock in the developing countries. Mortality rates have been
reported to be as high as 30% for sepsis, 40% for severe sepsis and 80%
for septic shock [4-6] in developed countries. Worldwide septic shock is still the leading cause for death in intensive care units [5].
Data from developed countries show a continuous increase in the
incidence of sepsis thus further emphasizing the need to review
management protocols in order to reduce morbidity and mortality. In
developed countries the implementation of protocols for the
identification of sepsis and management thereof, have contributed to a
decline in mortality rates [7].
In low income countries major concerns regarding
accessibility to healthcare, limitations due to costs, lack of resources
and delayed presentations of patients with sepsis make implementing
such protocols, based on developed countries patients profile difficult.
Thus in Sub-Saharan Africa there has been a widespread shift towards
protocol development that is cost effective and specific for the
epidemiologic and ecologic data [8,9].
In 2006 a Ugandan based prospective study assessed the management and
outcomes of hospitalized patients with severe sepsis syndromes.
Approximately 85% of their sample was HIV positive.
Factors contributing to mortality included inadequate
fluid administration, lack if uniformity in source appropriate
antibiotic administration and delay in antibiotic administration [8].
A follow-up prospective study was then done in 2008 using the previous
study as the observation cohort. Interventions included early
appropriate antibiotic and intravenous fluid administration. Mortality
at 30 days was significantly lower in the intervention cohort compared
to the observation cohort concluding that simple and inexpensive
management could improve outcome [8,9]. The surviving sepsis campaign [1]
is an initiative that initially was published in 2004 reviewing data on
the management of severe sepsis and septic shock. The recommendations
are intended to be best practice and by no means standard of care.
Currently no data is available in South Africa regarding sepsis
management in our unique setting thus we hope to pilot the way for
further research in this field.
Demographics
Karl Bremer Hospital (KBH) is a large district level
hospital situated in Bellville, Cape Town, with a total of 310 beds. The
hospital services on average 11000 patients per month. The estimated
total cost per day, per patient, is R2105.90 for a ward admission.
Almost 72% of the patients are classified as either earning no income or
have an average earning of less than R3000 per month, and hence are not
obligated to pay for full medical fees. Furthermore there is a 4 bed
high care unit which is shared by the all departments. The high care
unit is able to manage ventilated patients however if a prolonged high
care admission is anticipated, these patients would need to be
transferred to a fully equipped ICU at a tertiary facility such as
Tygerberg Hospital that is managed by a dedicated ICU team. Additionally
the emergency department (ED) has 3 resuscitation beds for all
emergencies that may present to the casualty.
Methodology
The primary aim of our study was to determine the
efficacy of sepsis identification and management by clinicians at Karl
Bremer Hospital. Furthermore we aimed to determine the demographics of
patients presenting with sepsis, and also the burden of sepsis and its
management, on the mortality rates and length of hospital stay amongst
patients admitted. Key determinants of efficacy were assessed using
guidelines outlined in the Surviving Sepsis Campaign 2012 as a means of
comparison. A retrospective descriptive study design was performed in
order to achieve the above. Ethics approval was obtained from the Health
Research Ethics Committee at the University of Stellenbosch. The
internal medicine department performs a routine burden of disease audit
on a three monthly basis. Data for the audit is obtained by means of
triplicate discharge letters, hospital transfer notes and death
certification summaries containing all relevant information of the
patients hospital stay from admission to discharge or death.
Data from the burden of disease audit completed in
October 2015 and January 2016 was reviewed for patient selection. In
order to select patients for the study the data from the burden of
disease audit sheets had to state any one of the following key words
namely sepsis, severe sepsis or septic shock as the diagnosis at
discharge or death. The suspected or confirmed infection had to be
present at emergency department presentation in order to qualify for the
study. Data was assessed using a data collection sheet compiled by the
authors that focused specifically on clinical and blood gas measures
that could be used in the emergency department to classify patients as
sepsis, severe sepsis and septic shock. Time to first dose antibiotics
(grade 1B evidence based on SCC), source appropriate antibiotics (grade
1B), amount of intravenous fluids (grade 1c) and arterial blood gas
(ABG)/lactate measurement was also assessed.
Once the data was obtained we retrospectively
classified patients into either sepsis, severe sepsis or septic shock
based on information that was available to the casualty doctor at the
time of presentation. All data collected was captured onto a Microsoft
Excel© database. Data analysis was done in Microsoft Excel© and
statistical analysis in Statistica©. Statistical significance was
considered if the p value< 0.05. To compare descriptive variables the
sign test was used. To assess for data association logistic regression
testing and negative binomial regression testing was performed. Here the
data was interpreted as odds ratios (OR) with a 95% confidence interval
(Table 1).

Statistical Results
From the 1000 patients reviewed in the burden of
disease audit, 70 patients (7%) were included in the study. Of the 70
patients 34 were male (48.5%) and 36 were female (51.4%). The overall
mean age of patients presenting with a sepsis syndrome was 48 (SD ± 9.5,
min=17, max=85). A total of 25 patients (36%) were HIV positive. The
most common infective cause for sepsis across all spectrums identified
by emergency personnel was a lower respiratory tract infection. Not
surprisingly diarrheal disease/acute gastroenteritis was the second most
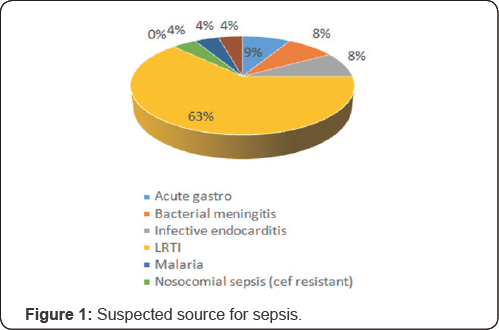
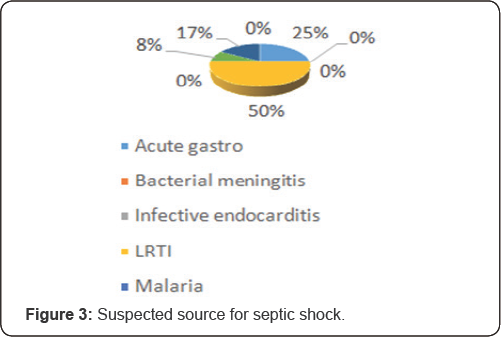
common diagnosis made (Figure 1, 2 &3)

Based on the data collection and subsequent sepsis
sub grouping, evaluated using the initial information available to the
casualty doctor, 24/70 patients (34%) were classified as having sepsis,
34/70 (48%) had severe sepsis and 12/70 (17%) had septic shock. However
18/24 (75%) of patients with sepsis, 8/34 (25%) of patients with severe
sepsis and 3/12(25%) of patients with septic shock had no arterial blood
gas or lactate measured at initial presentation. No patients who had an
initial lactate measured then had a repeat lactate measured in order to
assess for lactate clearance or fluid responsiveness. Thus as a result
many of the patients who likely should have been classified as septic
shock were then classified as severe sepsis based on adherence to
definitions. A total of 18/70 (26%) patients had an initial triage blood
pressure indicative of sepsis induced hypotension however only 1/18
(5.5%) of these patients received an initial crystalloid fluid bolus of
30ml/ kg and subsequent immediate blood pressure recheck for the fluid
responsive status. Furthermore 6/18 (33%) patients had no initial
arterial blood gas or lactate measured, thus authors had no way of
knowing whether the initial classification of the patient was severe
sepsis or septic shock, forcing us to assign patients to the severe
sepsis group.
The most frequently prescribed antibiotic across all categories for sepsis was ceftriaxone (Figure 4).
Bearing in mind the above literature review regarding source
appropriate antibiotics 55/70 patients (78.5%) were deemed to have
received the correct antibiotics prescribed for the respective source.
However no HIV positive patient included in the study received cover for
mycobacterium tuberculosis or pneumocystis jirovecii pneumonia in the
first 24 hours of presentation, despite the clinician having a
documented suspicion thereof.

Interestingly, what is also important to note is that
7/70(10%) of the patients received no antibiotics in the first 24hours
of presentation to hospital despite being identified by the casualty
doctor as having a possible infective cause for clinical symptomatology.
Here the likely source was equally distributed between acute
gastroenteritis and an unknown source for sepsis. Of these patients 3/7
of the patients could be classified as having septic shock based on
initial lactate measurement. The median time for antibiotic
administration in the first 24 hours of presentation across all
subgroups included 3.63 hours for sepsis (range 1.67-10.30, max= 24
hours), 1.58 hours for severe sepsis (range 1.00-2.83, max 24hours) and
4.25 hours for septic shock (range 1.00-23.98, max 24 hours). What is
very important to note here is that this is the time taken from the
attending doctors consult to actual antibiotic administration. Hence the
time from initial presentation to the emergency department to actual
antibiotic given may differ depending on waiting times. This
unfortunately could not be assessed due to lack of documentation of
initial presenting time.
In order to assess whether antibiotics were given
within the 3 hour time frame for sepsis and severe sepsis the sign test
was used to extrapolate the data. The results showed that for both
sepsis and severe sepsis there was no delay in antibiotic administration
( p value = 0.2706 for sepsis and 0.9997 for severe sepsis), bearing in
mind that the 3 hour mark was used as the cut off for optimal time to
initial antibiotic administration. For septic shock however a cut off of
1 hour was used for optimal time to antibiotic administration, here the
sign test showed a positive delay in antibiotic administration (p
value= 0.0039).
Regarding the early appropriate intravenous fluid
administration discussed above, the data showed that 5/24 (20%) of
patients with sepsis, 8/34 (23%) of patients with severe sepsis and 8/12
(66%) of patients with septic shock received inappropriate amounts of
fluids. As mentioned before only 1 patient received an initial fluid
bolus of >30ml/kg for a sepsis induced hypotension. Using the Pearson
chi-square test a positive association between the patients with septic
shock and inappropriate intravenous fluid administration was noted (P
value= 0.009). Furthermore the proportion of septic shock patients that
received appropriate intravenous fluids was less than half that of the
sepsis and severe sepsis group. As mentioned no patients in our study
had repeat ABG'S done in order to assess for lactate clearance, a marker
of response to therapy. Also no invasive measures such as central
venous pressures or arterial line blood pressure readings were used to
optimally assess fluid responsiveness in the first 24 hours of
management.
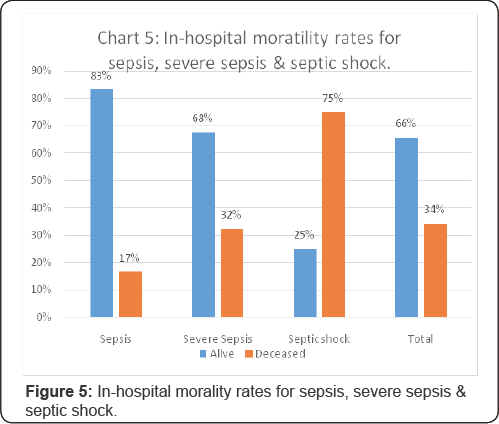
Overall the outcome of patients in the study was
determined by either discharge or in-hospital mortality. The in-
hospital for mortality for sepsis being 4/24 (17%), for severe sepsis
11/34 (32%) and a staggering 9/12(75%) for septic shock (Figure 5).
The mean age of deceased patients across all sepsis syndromes is 53 (SD
± 9.5). Furthermore logistic regression testing was done in order to
investigate for a possible association between in- hospital mortality
rates and various sepsis management principles. A positive association
between in-hospital mortality and the following was found:
1. Time to first dose antibiotic administration
(OR=1.07, P value= 0.027, 95%CI=1.008-1.14). For every 1 hour delay in
antibiotic administration the chance of death increased by 7%.
2. Source appropriate antibiotics (OR=0.17, P value=
0.005, 95% CI= 0.048-0.59). The chance of death amongst patients that
received source appropriate antibiotics is 83% less than those who did
not.
3. Early appropriate intravenous fluid administration
(OR=0.33, P value=0.040, 95% CI= 0.11-0.95). An appropriate intravenous
fluid was associated with a 67% reduction in inhospital mortality.
The mean length of stay for all sepsis syndromes was 6.3 days (SD ± 2.3 days).
Discussion
The statistics above depict clear faults in the
identification of sepsis and its resultant suboptimal management.
Evidence to support the poor recognition of sepsis syndromes is noted by
the lack of adequate fluid boluses for patients that met the definition
for hypotension at admission. This indicates that clinicians lack the
understanding of hypotension as a clinical indicator of organ
dysfunction in sepsis. Clinicians at Karl Bremer Hospital do not have
access to laboratory results for a minimum of 12 hours post consult and
are thus forced to make use of clinical judgment regarding severity of
disease. This can be aided by blood pressure monitoring, urine output
and blood gas measurement for lactate and PF ratios to determine fluid
responsiveness and organ dysfunction. Further data supporting
inadequacies in sepsis identification is evidenced by the 3/7 patients,
that could be classified as septic shock based on the initial blood gas
lactate measurement, who did not receive antibiotics for the first 24
hours after presentation. This indicates a poor understanding of the
effect of delayed antibiotics on mortality rates related to sepsis. The
overall median time to initial antibiotic administration was 4.25 hours
in septic shock versus 1.58 hours in severe sepsis. Because these 3
patients were patients with septic shock it significantly increased the
median time to initial antibiotic administration in this subgroup.
Kumar, et al. [10]
showed a decrease in survival by 7.6% for every 1 hour delay in
antibiotic therapy over the ensuing 6 hours.Comparatively our study
showed a 7% increase in mortality for every hour delay in antibiotic
administration. As mentioned median time to first dose antibiotics was
assessed from time of doctor/patient consult to initial antibiotic
administration. The minimum waiting time in the ED from arrival at the
hospital to doctor consult is 45-60min. Thus regardless of the
difference neither group is meeting the target 3 hour and 1 hour
administration time frame. This can be attributed to both poor
identification as discussed above and resource limitations. The nursing
staffs in the ED who are responsible for drug and fluid administration
often oversee the management of 10-20 patients at any given moment. This
makes it difficult for them to perform important tasks in a timorously
manner. Bed constraints and lack of resuscitation room availability mean
that severely ill patients will often lie in the general ED area where
there is no appropriate monitoring.
Regarding source appropriate antibiotics a positive association with mortality was shown in our study. Leibovici L, et al. [11]
showed improved survival when empiric antibiotic treatment matched the
in vitro susceptibility of the likely pathogen. The concern with this is
that we have limited evidence regarding source appropriate antibiotics
in a HIV prevalent society. Infective etiologies in sub -Saharan Africa
differ from those reported in the surviving sepsis guidelines; in fact
certain studies reviewed by the committee excluded HIV positive
patients. Begging the question which is the early source appropriate
antibiotics that should be administered given the unique sub-Saharan
Africa ecology and what is the effect on outcome in HIV positive
patients.
Appropriate intravenous fluid administration is a
further area for debate in the HIV prevalent South African setting. Both
studies done in Uganda and Zambia [12]
reported concerns regarding large fluid boluses with a resultant
worsening respiratory failure in this setting. Despite this our findings
show a 67% reduction in in-hospital mortality with appropriate
intravenous fluid administration. Again concerns regarding appropriate
monitoring in the emergency department make appropriate fluid
administration difficult, patients receiving large fluid boluses run the
risk of becoming fluid overloaded unless adequately monitored.
Recommendations
It is evident from the above that education for all
health care providers involved in sepsis identification and management
is necessary. A suggestion for process formation perhaps in the form of a
sepsis check sheet may lead to improved management. Re-evaluation of
outcomes in the form of length of hospital stay and in-hospital
mortality will need to done in order to evaluate the impact of process
formation. Further areas that need attention is improved availability of
early laboratory results which aids decision making. Also increasing
physician availability to decrease ED waiting times.
Conclusion
The primary aim of our study was to evaluate the
identification and management of the sepsis syndromes at a district
level hospital in the Western Cape Province. The outcomes of the study
concluded that the initial classification of sepsis, severe sepsis and
septic shock by our clinicians is flawed. This is largely due to a lack
of understanding by medical personnel regarding the clinical evidence
needed to support the classification process. This clinical evidence is
not dependent on delayed laboratory results, but can be found on basic
clinical assessment and investigations available in the emergency
department.
Priorities in the management of the sepsis syndromes
that have been shown in our study to negatively effect in-hospital
mortality include early source appropriate antibiotics and early
appropriate intravenous fluid administration. These should be the
cornerstones of management and can be instituted regardless of resource
availability. In conclusion it is evident that additional research is
needed in the field of sepsis identification and management in a
resource limited setting, however basic management principles can still
be implemented with the potential for an inordinate impact on patient
survival.
Acknowledgement
A special thank you to Dr Zirkia Joubert and all the
internal medicine medical officers at Karl Bremer Hospital, for granting
us the time we needed to work on this study as well as for all their
assistance with patient identification and data collection. We would
like to thank Mr. MT Chirehwa for the data analytics and his subsequent
interpretation of the statistical outcomes. Finally, we would like to
thank Iesrafeel Jakoet and Brendon Versfeld for all their help with the
write-up and editing of our study.
Conflict of interest
The authors have no conflict of interest to report. The project was funded solely by the named authors below.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment