Dexmedetomidine V/S Fentanyl with 0.75% Ropivacaine for Epidural Anaesthesia in Lower Abdominal Surgeries - A Comparative Study-Juniper Publishers
Juniper Publishers-Journal of Anesthesia
Abstract
Background: Opioids as epidural adjunct to
local anaesthetics have been in use since long and a-2 agonists are
being increasingly used for similar purpose. This study was done to
compare the effects of epidurally administered dexmedetomidine and
fentanyl in combination with Ropivacaine 0.75% in lower abdominal
surgeries.
Methods: 80 patients of either sex, aged 18-55
years, ASA grade I-II posted for elective lower abdominal surgery were
divided into two groups (n=40) by open label randomization chit method.
Group RD received 1^g/kg Dexmedetomidine and group RF received 1^g/kg
Fentanyl along with 15 ml Ropivacaine 0.75%. Onset and time of complete
sensory and motor blockade, two segmental dermatomal regression,
duration of analgesia, first 24 hour total LA consumption and
complications were recorded. Data were compiled and analysed using
Chi-square test and Fisher's exact test.
Results: Onset of complete sensory and motor
block was significantly earlier in the RD(9.375 ± 0.2256 min and 14.65 ±
0.3588 min) as compared to group RF (11.45 ± 0.3281 min and 17.1 ±
0.4294 min) (p<0.0001). Postoperative analgesia was significantly
prolonged in group RD as compared to group RF (374.3 ± 6.793Vs283.5 ±
5.576 min) (p<0.0001).Total duration of motor and sensory block was
longer in group RD (276.6 ± 5.668 and 140.9 ± 3.602 min) as compared to
group RF (198.4 ± 4.509 and 117.8 ± 2.715 min) (p<0.0001). Total LA
consumption was lesser in group RD as compared to group RF (112.5 ±
7.869 mgVs 132.5 ± 8.758 mg) (p<0.0001). Hypotension, bradycardia and
dry mouth was significant in group RD while nausea and vomiting was
significant in group RF.
Conclusion: Dexmedetomidine is better
alternative to fentanyl as an epidural adjuvant, due to comparatively
faster onset of blockade, prolonged postoperative analgesia and lower
consumption of post-op LA.
Keywords: Dexmedetomidine; Fentanyl; Epidural anaesthesia Introduction
Epidural anaesthesia is an integral part of today's
practice of anaesthesia, as it gives the anaesthesiologist the
opportunity to place it at any level of the vertebrae to provide
anaesthesia and analgesia, to supplement general anaesthesia, decrease
the need for deep levels of general anaesthesia and therefore provide
haemodynamically stable operative course. As early postoperative
mobilization and rehabilitation with minimally associated pain and
discomfort is the most desirable feature for modern orthopaedic and
general surgeries so epidural becomes desirable technique of anaesthesia
[1]. It not only provides perioperative surgical anaesthesia but also post-op analgesia in lower abdominal and limb surgeries [2].
Epidural bupivacaine was used since long but it is
highly cardiotoxic. Recently ropivacaine became better alternative in
choice of LA, due to long duration and less cardiovascular effects [3]. Very slow reversal of Na+
channel blockade after a cardiac action potential, which is the
hallmark of bupivacaine, is considerably faster with ropivacaine, also
the negative inotropic potency of ropivacaine on isolated cardiac tissue
appears to be considerably less than that of bupivaicaine [4].
Adding adjuvants to LA have proven better and faster onset of blockade,
prolonged duration of action and postoperative analgesia with lower
consumption of local anaesthetic. Adjuvants like opioids can perform
these activities but as to their certain side effects like pruritus,
urinary retention, nausea and vomiting, newer adjuvants are been
considered.
Fentanyl, a highly lipophilic opioid, has relatively
rapid onset of action following administration. It has become very
popular additive in recent times. However, it has side effects like
pruritus, nausea and vomiting, hence, there was need for an alternative
which was deprived of these side effects but has same or better
qualities like opioids when used as adjuvant.
Dexmedetomidine is a new addition of a-2 agonist
which has got numerous beneficial effects when used through epidural
route. It does cause manageable hypotension and bradycardia but the
striking effect of it is lack of opioid related side effects. Because of
paucity of comparative studies between fentanyl and dexmedetomidine as
an adjuvant to ropivacaine for epidural anaesthesia, we decided to
compare both these drugs in our institute in terms ofonset and time of
complete sensory and motor blockade, two segmental dermatomal
regression, duration of analgesia, first 24 hour total LA consumption
and complications.
Methods
Present study was conducted in the Department of
Anaesthesiology and Critical care, Pt. J.N.M. Medical College and Dr.
B.R.A.M. Hospital Raipur (C.G) after approval from the institutional
ethics committee. It was a prospective randomizeddouble blind study, 80
patients of ASA I-IIaged 18-55 years of either sex undergoing lower
abdominal surgeries were randomly allocated by chit method into 2 Groups
(n=40). Group RD received dexmedetomidine 1μg/kg and Group RF received
fentanyl 1μg/kg along with ropivacaine 0.75% 15 ml. Before the study,
power of study was calculated by using software G power 3.0.10, taking
mean value for onset of sensory blockade from Bajwa S, et al. [5]
and considering a probability level of 0.05 (α-error) and power of 0.80
(1-β) yielded a sample size of 40 patients in each group.
Patients with history of drug allergy, gross spinal
abnormality, localized skin sepsis, hemorrhagic diathesis, neurological
disease, hepatic and renal diseases, peripheral neuropathy and
psychiatric diseases were excluded from the study.
After preoperative assessment, written informed
consent was taken from all patient and kept nil orally for 8 hrs before
surgery. On the day of surgery, intravenous line was secured and
preloaded with Ringer Lactate solution 10 ml /kg over 20 minutes prior
to the procedure, all patients were premedicated with i.v. 50 mg
Ranitidine and i.v. Ondensatron 4 mg 15 min prior to epidural
anaesthesia.
Epidural anaesthesia was performed in sitting
position and under all aseptic precautions, L3-L4 or L2-L3 interspace
was identified and local infiltration by 2 ml 2% lignocaine with
adrenaline was done at one of the interspaces. An epidural needle
(Tuohy's) 18G was inserted through the midline approach and epidural
space was located by loss of resistance to air method. Direction of the
bevel was kept cephalad in all the cases. A disposable sterile multi
hole epidural catheter was threaded 3-5 cm cephalad in the epidural
space and was secured with adhesive tape. Test dose of 3 ml 2%
lignocaine with adrenaline 1:200000 was injected, followed by total
volume of 15 ml of either of the study drug were injected through the
epidural catheter.Epidural supplementation was done on requirement of
analgesia in postoperative period by 0.2% ropivacaine 10ml.
Sensory block was assessed by pin prick method at
every 2 min interval till 30 min and then every 15 min until the return
of normal sensation at dermatome levels S3, S1, L5, L3, L1, T12, T10, T8 and T6
and the maximal sensory blockade level was noted. Onset and end of all
degrees of motor blocks were assessed bilaterally according to the
Modified Bromage scale [6]
until the return of Bromage 1. [0= No motor block (ability to move
hips, knees and ankles), 1 = inability to raise extended leg (able to
flex knee); 2 = inability to flex knee (able to flex foot only); 3 =
inability to flex ankle joint (unable to flex foot or knee)].
Onset of sensory blockade (time interval from
epidural injection of drugs to sensory blockade at T10), onset of motor
block (time interval from epidural injection of drug to achieve modified
Bromage scale grade I), extent of block (highest dermatomal level of
sensory block achieved), duration of sensory block (time to two
segmental dermatome regression), duration of motor block (time interval
fromachievement of Bromage
I to regression of motor blockade to Bromage I), duration of analgesia
(time from onset of sensory block to first complain of pain), sedation
score was observed and recorded. Hemodynamic parameters like PR, SBP,
DBP, MBP, RR, and SpO2 were recorded before induction and at
every 5 minutes intervals for 30 minutes and later at 15 minutes
intervals lasting for the entire duration of surgery.
Sedation score5was assessed by Ramsay Sedation Score
and recorded just before the initiation of surgery and thereafter every
20 minutes during the surgical procedure (1-alert and wide awake,
2-arousable to verbal command, 3-arousable with gentle tactile
stimulation, 4-arousable with vigorous shaking, 5-unarousable). Total
dose consumption of local anaesthetic over 24 hours (total dose required
till 24 hours including surgery and post-operative period) was
recorded.
Fall in SBP and DBP ≥ 20% of baseline was considered
as significant hypotension. It was managed with fast fluid
administration and i.v. mephentermine 6 mg. Heart rate <50/ min was
considered as bradycardia and treated with atropine
0. 5 mg i.v. Supplement O2 via face mask was given when SpO2
fell below 95%. Nausea and vomiting was treated with inj.
metaclopramide 10mg.
Throughout the procedure, patients were observed for
any side effects and complications related to technique and anaesthetics
drugs by lumber epidural anaesthesia and recorded. Statistical analysis
was done using Graph pad prism 7 Software. Data were analyzed by student t unpaired test and chi square test.
The results were analyzed by various statistical techniques like
percentage, mean and standard deviation. P-value <0.05 was considered
significant and p-value <0.0001 was considered highly significant.
Results
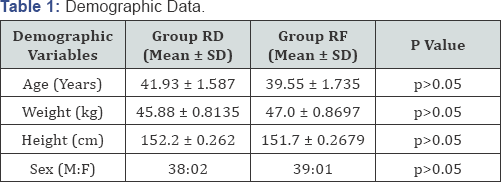
The two groups were statistically comparable with regard to demographic data (Table 1).
Onset of sensory and motor blockade in group RD was significantly
faster as compared to group RF, andthe difference was statistically
highly significant (p< 0.0001) (Table 2).
The highestlevel of sensory block achieved was T5-T6
level in group RD which was higher than group RF i.e. T6-T7 level. The
number of patients who achieved grade III and grade II motor blockade
was 36 and 04 in group RD as compared to 34 and 06 in Group RF. This
difference between both the groups proved higher level of block was
achieved in group RD compared to group RF.
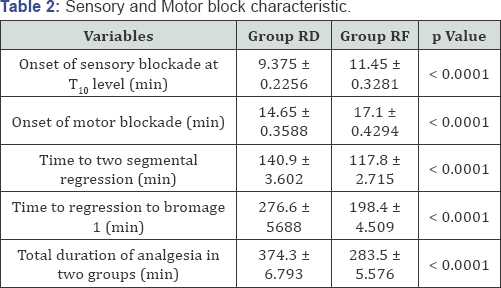
Duration of sensory blockwas significantly prolonged
in group RDas compared to group RF, and the difference was statistically
highly significant (p< 0.0001) (Table 2).
Duration of motor blockade and duration of analgesia was also
significantly prolonged in group RD as compared to group RF, and the
difference was statistically highly significant (p< 0.0001) (Table 2).
Total LA dose consumption over first 24 hours was 112.5 ± 7.869 mg in
group RD and 132.5 ± 8.758 mgin group RF. This was significantly low in
RD group (p<0.0001).
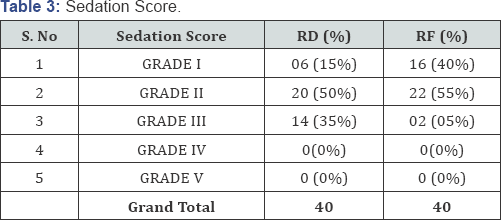
Maximum number of patients in both groups had grade
II sedation score i.e. 20(50%) in Group RD and 22 (55%) in Group RF.
Higher number of patients in Group RD had grade III of Ramsay Sedation
Score i.e. 14 (35%) as compared to 02 (05 %) in Group RF (Table 3).
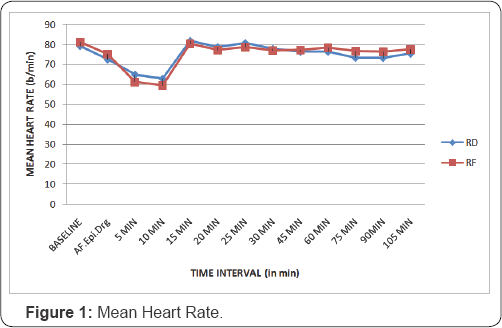
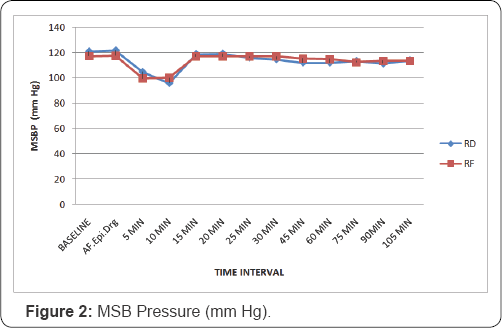
The fall in HR and mean SBPfrom baseline was
significant at 5 min and 10 min interval after injecting epidural drug
in both the Groups (p < 0.0001). But the change in HR and mean SBP
was statistically comparable between two at various other time intervals
(p>0.05) (Figure 1 & 2).
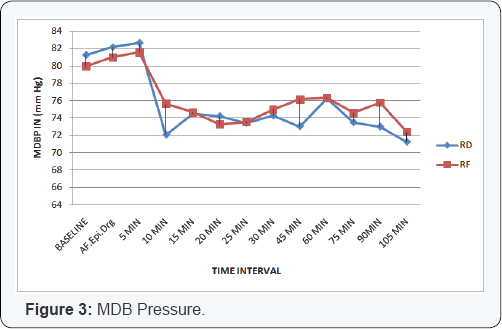
The fall in mean DBP from the baseline was significant at 5 min, 10
min, 15 min, 20 min and 25 min in Group RD while it was significant at
15 min and 20 min in Group RF after injecting epidural drug (p<
0.0001). But the change in DBP was statistically comparable between two
Groups RD and RF at various other time intervals (p>0.05).
Figure 3 Mean RR and SPO2 was comparable in both the
groupsRDand RF during our entire study period, respectively (p>0.05).
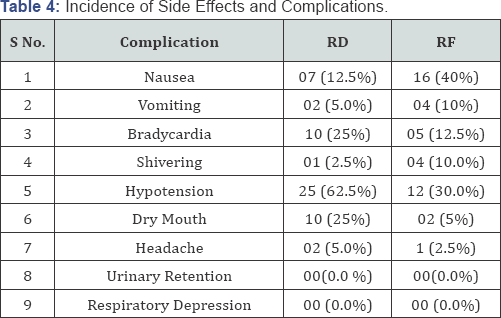
Comparison between the groups showed statistically no significant
difference in the complications/side effects (p >0.05). Incidence of
hypotension, bradycardia and dry mouth was significantly high in Group
RD, while nauseaand vomiting was significantly high in Group RF (p
<0.05) (Table 4).
Discussion
The aim of this study is to evaluate and compare the
efficacy of 0.75% ropivacaine and fentanyl with 0.75% ropivacaine and
dexmedetomidine in epidural anaesthesia in patients undergoing lower
abdominal surgeries.
I. The primary objective of this study is to compare the onset of sensory block between dexmedetomidine and fentanyl.
II. The secondary objective of this study is to
compare the onset of motor blockade, extent of block, duration of
sensory and motor block, duration of analgesia, sedation score, total LA
consumption and occurrence of side effects in the intraoperative period
between the two drugs.
In our study onset of sensoryand motor block was
earlier in group RD as compared to group RF, and the difference was
statistically highly significant (p<0.0001). It correlated with
findings of Vasupalli R et al. [6] and Agrawal S et al. [7]. The amount of study drug and adjuvants used in both the studies were similar to the amount of drugs used in our study.
Highest level of sensory block achieved was T5-T6 in
group RD (34 patients) and T6-T7 in group RF (35 patients). This showed
the block was higher in group RD in maximum number of patients compared
to group RF. Similar results were observed in group RD as compared to
group RF in Bajwa S, et al. [5] and in Vashisth, et al. [8] where highest level was T5 in group RD and T6 in group RF. The result of Bajwa S et al. [5] and Vashisth, et al. [8]
was similar as the study and adjuvants dexmedetomidine, clonidine and
fentanyl used was 1 |ig/kg which is similar to our study.
Duration of sensory block wasprolonged in group RD
compared to group RF andthe difference was statistically highly
significant.(p<0.0001)Similar results were seen in study of Bajwa SJ,
et al. [9]
when same amount of drug was given as in our study. Duration of motor
block and duration of analgesia was also longer in group RD as compared
to group RF, and the difference was also statistically highly
significant (p<0.0001). Similar results were seen in study of Singh R
et al. [10] where duration of motor block was prolonged in group RD as compared to group RF and in Mittal AA et al. [3] where duration of analgesia was prolonged in group RD compared to group RF.
Total LA consumption was significantly lesser in
group RD as compared to group RF.This was similarly seen in study of
Mittal AA, et al. [3] and Baglur S, et al. [11], where dexmedetomidine was given in same dose as in our study proving dexmedetomidine a better alternative to fentanyl.
In our study maximum number of patients in both the
groups had grade II sedation score and higher number of patients in
group RD had grade III and grade II score as compared to group RF. This
showed dexmedetomidine provided better sedation scores compared to
fentanyl, similar results were shown in study of Singh R, et al. [12] where 36% and 46% patients had grade II and grade III sedations scores compared to 18% and 4% in patients of group RF.
Mean RR was comparable in both the Groups and was
statistically insignificant throughout the surgical procedures
(p>0.05). Mean RR was above 12/min in both the Groups throughout
whole duration of procedure. SpO2 was above 95% in all the
patients of Group RD and Group RF throughout the study period and the
difference was statistically insignificant (p>0.05).
Significant decrease in mean HR and SBP from the
baseline was observed in group RD and RF was observed after 5 min and 10
min of injecting study drug but was comparable after 10 mins to
throughout the procedure, this correlated with the studies of Bajwa SJ,
et al. [9] and Singh RB, et al. [12] as same adjuvant and study drug was used. The fall in mean DBP in group RD correlated with studies of Rastogi B et al. [13] and Singh RB, et al. [12] while in group RF correlated with Singh RB, et al. [12].
Incidence of nausea was higher and significant in
Group RF as compared to Group RD and vomiting was slightly higher in
Group RF as compared to Group RD. The findings of our study that
fentanyl when used as adjuvant causes nausea and vomiting correlates
with Singh RB, et al. [12]
and Harinath G et al. The incidence of hypotension and bradycardia was
higher in Group RD patients as compared to and patients in Group RF. The
difference was comparable and stastically significant (p<0.05). The
findings observed in Baglur S, et al. [11] and Singh RB, et al. [12])
that there was comparable difference in hypotension and bradycardia as
clonidine was used, which is also an alpha
2 agonist, correlates with our study. The incidence of shivering in
Group RD and Group RF was comparable and statistically not significant.
(p>0.05) The incidence of dry mouth was statistically significantin
Group RD as compared to in Group RF (p <0.05). The incidence of
headache was not significant in both the groups while none of the
patients had urinary retention in either Group (p >0.05) (Table 3).
Conclusion
Our study shows faster onset, prolonged duration and
excellent sensory and motor blockade along with better sedation, stable
hemodynamics following epidurally administered dexmedetomidine with
ropivacaine compared to fentanyl with ropivacaine. Thus it could be
concluded that dexmedetomidine is better alternative to fentanyl as an
adjuvant for epidural anaesthesia with ropivacaine for lower abdominal
surgeries.
For more articles in Journal of Anesthesia
& Intensive Care Medicine please click on:
https://juniperpublishers.com/jaicm/index.php
https://juniperpublishers.com/jaicm/index.php
Comments
Post a Comment